Abstract
Study Design
Retrospective, comparative case series from the study group database.
Objectives
The primary objective was to report the neurologic injury rate for rib-based distraction surgery and determine whether preoperative diagnosis affects this rate. The secondary objective was to describe these injuries and outcome.
Summary of Background Data
Posterior distraction-based systems are commonly used to treat early-onset scoliosis. General complication rates for these surgeries are high; however, there are few reports in the literature on neurologic injury after rib-based distraction surgery. p ]Methods This was a retrospective review of the Children’s Spine Study Group database from 2004 to 2013. The researchers used the chi-square test to compare the distributions of proportions between diagnoses.
Results
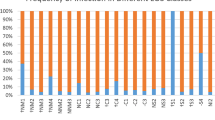
A total of 524 patients were identified and treated with rib-based distraction surgery. The preoperative diagnoses consisted of 222 congenital/structural, 163 neuromuscular, 63 syndromic, 67 idiopathic, and 9 unknown. There were 9 neurologic injuries (7 clinical and 2 neuromonitoring alerts) for a neurologic injury rate of 1.7%. Using the Classification for Early-Onset Scoliosis, 8 patients were classified as congenital and 1 as neuromuscular. The neurologic injury rate in the congenital curves group was 3.6% and was 0.34% in non-congenital curves (p =.005). The proportion of injured patients with an additional secondary diagnosis was 3.82%, compared with 0.82% patients with only a primary diagnosis (p =.01). Eight injuries occurred at initial implantation and 1 at revision surgery. Most were brachial plexus (n = 5) with no complete spinal cord injuries. Four patients required return to surgery and 1 needed intraoperative intervention. At 4.2 years’ follow-up, 7 of 9 patients had full resolution of symptoms and 2 patients had residual upper extremity weakness. p ]Conclusions The rate of neurologic injury for patients treated with rib-based distraction surgery was 1.7%. Most injuries occurred with congenital diagnoses and they were more likely in patients with additional secondary diagnoses. These injuries were predominantly to the brachial plexus and generally resolved.
Similar content being viewed by others
References
Sankar WN, Skaggs DL, Yazici M, et al. Lengthening of dual growing rods and the law of diminishing returns. Spine (Phila Pa 1976) 2011;36:806–9.
Campbell Jr RM. Operative strategies for thoracic insufficiency syndrome by Vertical Expandable Prosthetic Titanium Rib expansion thoracoplasty. Oper Techn Orthop 2005;15:315–25.
Campbell Jr RM, Smith MD, Mayes TC, et al. The effect of opening wedge thoracostomy on thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am 2004;86:1659–74.
Bess S, Akbarnia BA, Thompson GH, et al. Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am 2010;92:2533–43.
Sankar WN, Skaggs DL, Emans JB, et al. Neurologic risk in growing rod spine surgery in early onset scoliosis. Spine (Phila Pa 1976) 2009;34:1952–5.
Watanabe K, Uno K, Suzuki T, et al. Risk factors for complications associated with growing-rod surgery for early-onset scoliosis. Spine (Phila Pa 1976) 2013;38:E464–8.
Wang S, Zhang J, Qiu G, et al. Dual growing rods technique for congenital scoliosis: more than 2 years outcomes: preliminary results of a single center. Spine (Phila Pa 1976) 2012;37:el639–44.
Hasler C-C, Mehrkens A, Hefti F. Efficacy and safety of VEPTR instrumentation for progressive spine deformities in young children without rib fusions. Eur Spine J 2010;19:400–8.
Sankar WN, Acevedo DC, Skaggs DL. Comparison of complications among growing spinal implants. Spine (Phila Pa 1976) 2010;35:2091–6.
Gadepalli SK, Hirschl RB, Tsai WC, et al. Vertical expandable prosthetic titanium rib device insertion: does it improve pulmonary function? J Pediatr Surg 2011;46:77–80.
Lucas G, Bollini G, Jouve JL, et al. Complications in pediatric spine surgery using the VEPTR (Vertical Expandable Prosthetic Titanium Rib): the French experience. Spine (Phila Pa 1976) 2013;38:E1589–99.
Emans JB, Caubet JF, Ordonez CL, et al. The treatment of spine and chest wall deformities with fused ribs by expansion thoracostomy and insertion of vertical expandable prosthetic titanium rib: growth of thoracic spine and improvement of lung volumes. Spine (Phila Pa 1976) 2005;30 (17 Suppl):S58-68.
Skaggs DL, Choi PD, Rice C, et al. Efficacy of intraoperative neurologic monitoring in surgery involving a vertical expandable prosthetic titanium rib for early-onset spinal deformity. J Bone Joint Surg Am 2009;91:1657–63.
Vitale MG, McCalla DJ, Matsumoto H, et al. The classification for early-onset scoliosis (C-EOS) predicts timing of VEPTR anchor failure. J Child Orthop 2012;6:439–59.
Corona J, Miller DJ, Downs J, et al. Evaluating the extent of clinical uncertainty among treatment options for patients with early onset scoliosis. J Bone Joint Surg Am 2013;95:e67.
Auerbach JD, McGowan KB, Halevi M, et al. Mitigating adverse event reporting bias in spine surgery. J Bone Joint Surg Am 2013;95:1450–6.
Raynor BL, Bright JD, Lenke LG, et al. Significant change or loss of intraoperative monitoring data: a 25-year experience in 12,375 spinal surgeries. Spine (Phila Pa 1976) 2013;38:E101–8.
Phillips JH, Lopez D, Knapp DR, et al. The recognition, incidence, and management of spinal cord monitoring alerts in early onset scoliosis surgery. J Child Orthop 2012;6:439–59.
Smith JT, Johnston C, Skaggs D, et al. A new classification to report complications in growing spine surgery: a multicenter consensus study. J Child Orthop 2012;6:439–59.
Mcelroy MJ, Sponseller PD, Dattilo JR, et al. Growing rods for the treatment of scoliosis in children with cerebral palsy: a critical assessment. Spine (Phila Pa 1976) 2012;37:el504–10.
Gomez JA, Vitale MG. Measuring outcomes in children with early-onset scoliosis. Semin Spine Surg 2012;24:140–3.
Phillips JH, Knapp DR, Herrera-Soto J. Mortality and morbidity in early onset scoliosis surgery. Spine (Phila Pa 1976) 2013;38:324–7.
McCalla DJ, Matsumoto H, Nair K, et al. The Early-Onset Scoliosis Questionnaire (EOSQ) reflects improvement in quality of life after growing surgery. J Child Orthop 2012;6:439–59.
Schroerlucke SR, Akbarnia BA, Pawelek JB, et al. How does thoracic kyphosis affect patient outcomes in growing rod surgery? Spine (Phi-la Pa 1976) 2012;37:1303–9.
Reinker K, Simmons JW, Paul V, et al. Can VEPTR® control progression of early-onset kyphoscoliosis? A cohort study of VEPTR® patients with severe kyphoscoliosis. Clin Orthop Relat Res 2011;469:1342–8.
Samdani AF, Ashgar J, Pahys J, et al. Concurrent spinal cord unte-thering and scoliosis correction: case report. Spine (Phila Pa 1976) 2007;32:e832–6.
Hamzaoglu A, Ozturk C, Tezer M, et al. Simultaneous surgical treatment in congenital scoliosis and/or kyphosis associated with intraspinal abnormalities. Spine (Phila Pa 1976) 2007;32:2880–4.
Mehta VA, Gottfried ON, McGirt MJ, et al. Safety and efficacy of concurrent pediatric spinal cord untethering and deformity correction. J Spinal Disord Tech 2011;24:401–5.
Ayvaz M, Akalan N, Yazici M, et al. Is it necessary to operate all split cord malformations before corrective surgery for patients with congenital spinal deformities? Spine (Phila Pa 1976) 2009;34:2413–8.
Hui H, Tao HR, Jiang XF, et al. Safety and efficacy of 1-stage surgical treatment of congenital spinal deformity associated with split spinal cord malformation. Spine (Phila Pa 1976) 2012;37:2104–13.
Gavriliu S, Vlad C, Georgescu I, et al. Diastematomyelia in congenital scoliosis: a report of two cases. Eur Spine J 2014;23 (Suppl 2):262–6.
Lao L, Zhong G, Li X, Liu Z. Split spinal cord malformation: report of 5 cases in a single Chinese center and review of the literature. Pe-diatr Neurosurg 2013;49:69–74.
Ayvaz M, Alanay A, Yazici M, et al. Safety and efficacy of posterior instrumentation for patients with congenital scoliosis and spinal dys-raphism. J Pediatr Orthop 2007;27:380–6.
Oda JE, Shah SA, Mackenzie WG, et al. Concurrent tethered cord release and growing-rod implantation—is it safe? Global Spine J 2012;2:207–12.
Hui H, Luo ZJ, Yan M, et al. Non-fusion and growing instrumentation in the correction of congenital spinal deformity associated with split spinal cord malformation: an early follow-up outcome. Eur Spine J 2013;22:1317–25.
Campbell RM, Smith MD, Hell-Vocke AK. Expansion thoracoplasty: the surgical of opening-wedge thoracostomy: surgical technique. J Bone Joint Surg Am 2004;86 (Suppl 1):51–64.
Emans J, Caubet JF, Ordonez Cl, et al. The treatment of spine and chest wall deformities with fused ribs by expansion thoracotomy and insertion of vertical expandable prosthetic titanium rib: growth of thoracic spine and improvement of lung volumes. Spine (Phila Pa 1976) 2005;30 (Suppl 17):S58–68.
Nassr A, Larson AN, Crane B, et al. Iatrogenic thoracic outlet syndrome secondary to vertical expandable prosthetic titanium rib expansion thoracoplasty: pathogenesis and strategies for prevention/ treatment. J Pediatr Orthop 2009;29:31–4.
Joiner ERA, Andras LM, Skaggs DL. Mechanisms and risk factors of brachial plexus injury in the treatment of early-onset scoliosis with distraction-based growing implants. J Bone Joint Surg Am 2013;95:el611–7.
Akbarnia BA, Emans JB. Complications of growth-sparing surgery in early onset scoliosis. Spine (Phila Pa 1976) 2010;35:2193–204.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: LG (non-financial support from Children’s Spine Study Group during the conduct of the study); YM (non-financial support from Children’s Spine Study Group during the conduct of the study); SA (none); ALM (non-financial support from Children’s Spine Study Group during the conduct of the study); JMF (personal fees from Biomet, LWW outside the submitted work); REH (non-financial support from Children’s Spine Study Group during the conduct of the study; grants from Depuy-Synthes Spine, Medtronic Canada; personal fees from Depuy-Synthes Spine, Halifax Biomedical, Inc., outside the submitted work).
This work was supported by the Children’s Spine Study Groups, formerly known as the Chest Wall and Spine Deformity Study Group
Rights and permissions
About this article
Cite this article
Gauthier, L.E., Mandourah, Y., Soroceanu, A. et al. Perioperative Neurologic Injury Associated With Rib-Based Distraction Surgery. Spine Deform 2, 481–488 (2014). https://doi.org/10.1016/j.jspd.2014.08.003
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2014.08.003