Abstract
Study Design
Clinical case series.
Objective
To characterize the postoperative course and histopathology of peri-implant tissue of adolescent idiopathic scoliosis patients who experienced postoperative development of an aseptic soft tissue reaction, with granulomas adjacent to the sublaminar polyethylene terephthalate strap—titanium clamp used in Zimmer’s Universal Clamp (UC) spinal fixation system after spinal surgery.
Background Summary
The UC was designed for use with spinal deformity procedures in place of pedicle screws, hooks, or sublaminar wiring in fusion constructs. Recent studies of the UC lack emphasis on implant-related postoperative complications.
Methods
A total of 26 consecutive patients who underwent spinal deformity correction for scoliosis were reviewed for implant-related postoperative complications. Histology, scanning electron microscopy with energy-dispersive X-ray spectroscopy, fractional culture/biopsy, and Gram stain examination of the peri-implant tissue of patients with complications was performed.
Results
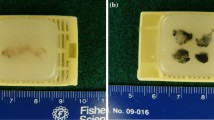
The authors reviewed 26 cases for correction of scoliosis. Two patients with adolescent idiopathic scoliosis who used the UC experienced implant-related complications with development of an aseptic soft tissue reaction with granulomas adjacent to the sublaminar polyethylene terephthalate straps—titanium clamp mechanism of the UC 8 months after AIS correction surgery. There were no signs or symptoms of wound infection. Gram stain revealed no organisms. There were many neutrophils and the surface of the wound revealed rare Staphylococcus aureus but the deep portions of the wounds were negative for organisms. Histopathology revealed extensive granulation tissue and histiocytes with engulfed birefringent particles or debris, and scanning electron microscopy with energy-dispersive X-ray spectroscopy analysis revealed macrophages containing many particles identified as titanium.
Conclusions
adolescent idiopathic scoliosis patients who use the novel UC construct may develop postoperative foreign-body reaction.
Similar content being viewed by others
References
Ilharreborde B, Even J, Lefevre Y, et al. Hybrid constructs for tridimensional correction of the thoracic spine in adolescent idiopathic scoliosis: a comparative analysis of universal clamps versus hooks. Spine (Phila Pa 1976) 2010;35:306–14.
Mazda K, Ilharreborde B, Even J, et al. Efficacy and safety of posteromedial translation for correction of thoracic curves in adolescent idiopathic scoliosis using a new connection to the spine: the universal clamp. Eur Spine J 2009;18:158–69.
Jouve J, Sales de Gauzy J, Blondel B, et al. Use of the universal clamp for deformity correction and as an adjunct to fusion: preliminary results in scoliosis. J Child Orthop 2010;4:73–80.
Kock H, Sturmer K, Letsch R, Schmit-Neuerburg K. Interface and biocompatibility of polyethylene terephthalate knee ligament prosthesis: a histological and ultrastructural device retrieval analysis in failed synthetic implants used for surgical repair of anterior cruciate ligaments. Arch Orthop Trauma Surg 1994;114:1–7.
Seitz H, Marlovits S, Schwendenwein I, et al. Biocompatability of polyethylene terephthalate (Trevirahochfest) augmentation device in repair of the anterior cruciate ligament. Biomaterials 1998;19:189–96.
Legnani C, Ventura A, Terzaghi C, et al. Anterior cruciate ligament reconstruction with synthetic grafts: a review of literature. Int Orthop 2010;34:465–71.
Seemann M, Steadman J. Tibial osteolysis associated with Gore-Tex grafts. Am J Knee Surg 1993;6:31–8.
Lukianov A, Richmond J, Barrett G, Gillquist J. A multicenter study on the results of anterior cruciate ligament reconstruction using a Dacron ligament prosthesis in “salvage” cases. Am J Sports Med 1998;17:380–6.
Gillquist J, Odensten M. Reconstruction of old anterior cruciate ligament tears with a Dacron prosthesis: a prospective study. Am J Sports Med 1993;21:358–66.
Barrett G, Line L, Shelton W, et al. The Dacron ligament prosthesis in anterior cruciate ligament reconstruction: a four-year review. Am J Sports Med 1993;21:367–73.
Maletius W, Gillquist J. Long-term results of anterior cruciate ligament reconstruction with a Dacron prosthesis: the frequency of osteoarthritis after seven to eleven years. Am J Sports Med 1997;25:288–93.
Klein W, Jensen K. Synovitis and artificial ligaments. Arthroscopy 1992;8:116–24.
Cunningham B, Orbegoso C, Dmitriev A, et al. The effect of titanium particulate on development and maintenance of a posterolateral spinal arthrodesis: an in vivo rabbit model. Spine (Phila Pa 1976) 2002;27:1971–81.
Dubousset J, Shufflebarger H, Wenger D. Late “infection” with C-D instrumentation. Orthop Trans 1994; 18:121 [abstract].
Wang J, Yu W, Sandhu H, et al. Metal debris from titanium spinal implants. Spine (Phila Pa 1976) 1999;24:899–903.
Hallab N, Cunningham B, Jacobs J. Spinal implant debris-induced osteolysis. Spine (Phila Pa 1976) 2003;28:S125–8.
Wimmer C, Krismer M, Gluch H, et al. Autogenic versus allogenic bone grafts in anterior lumbar interbody fusion. Clin Orthop Relat Res 1999;360:122–6.
Takahashi S, Delecrin J, Passuti N. Intraspinal metallosis causing delayed neurologic symptoms after spinal instrumentation surgery. Spine (Phila Pa 1976) 2001;26:1495–9.
Gaine W, Andrew S, Chadwick P, et al. Late operative site pain with isola posterior instrumentation requiring implant removal: infection or metal reaction. Spine (Phila Pa 1976) 2001;26:583–7.
Botolin S, Merritt C, Erickson M. Aseptic loosening of pedicle screws as a result of metal wear debris in a pediatric patient. Spine (Phila Pa 1976) 2012;38:E38–42.
Wimmer C, Gluch H. Aseptic loosening after cd instrumentation in the treatment of scoliosis: a report about eight cases. J Spinal Disord 1998;11:440–3.
Senegas J, Vital J, Pointillart V, et al. Long-term actuarial survivorship analysis of an interspinous stabilization system. Eur Spine J 2007;16:1279–87.
Konno S, Kikuchi S. Prospective study of surgical treatment of degenerative spondylolisthesis: comparison between decompression alone and decompression with Graf system stabilization. Spine (Phila Pa 1976) 2000;25:1533–7.
Hadlow S, Fagan A, Hillier T, et al. The Graf ligamentoplasty procedure: comparison with posterolateral fusion in the management of low back pain. Spine (Phila Pa 1976) 1998;23:1172–9.
Cunningham B, Dawson J, Hu N, et al. Preclinical evaluation of the Dynesys posterior spinal stabilization system: a nonhuman primate model. Spine J 2010;10:775–83.
Golish S, Anderson P. Bearing surfaces for total disc arthroplasty: metal on metal versus metal on polyethylene and other biomaterials. Spine J 2012;12:693–701.
Pandit H, Glyn-Jones S, McLardy-Smith P, et al. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br 2008;90:847–51.
Campbell P, Ebramzadeth E, Nelson S, et al. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res 2010;468:2321–7.
Cunningham B, Hallab N, Hu N, et al. Epidural application of spinal instrumentation particulate wear debris: a comprehensive evaluation of neurotoxicity using an in vivo animal model. J Neurosurg Spine 2013;19:336–50.
Cunningham BW, Towson, MD. Personal communication.
Punt I, Austen S, Cleutjens J, et al. Are periprosthetic tissue reactions observed after revision of total disc replacement comparable to the reactions observed after total hip or knee revision surgery? Spine (Phila Pa 1976) 2012;37:150–9.
Margevicius K, Bauer T, McMahon J, et al. Isolation and characterization of debris in membranes around total joint prosthesis. J Bone Joint Surg Am 1994;76:1664–75.
Reames D, Smith J, Fu KM, et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society morbidity and mortality database. Spine (Phila Pa 1976) 2011;36:1484–91.
Sansur C, Smith J, Coe J, et al. Scoliosis Research Society morbidity and mortality of adult scoliosis surgery. Spine (Phila Pa 1976) 2011;36:E593–7.
Mirra J, Marder R, Amstutz H. The pathology of failed total joint arthroplasty. Clin Orthop Relat Res 1982;170:175–83.
Goodman S, Chin R, Chiou S, et al. A clinical-pathologic-biochemical study of the membrane surrounding loosened and non-loosened total hip arthroplasties. Clin Orthop Relat Res 1989;244:182–7.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: JWD (none); RAB (none); ATT (none); JLA (none).
The authors thank Bryan W. Cunningham, PhD, Orthopaedic Spinal Research Institute and Scoliosis and Spine Center, University of Maryland St. Joseph Medical Center, for assistance.
Rights and permissions
About this article
Cite this article
Bailey, R.A., Duncan, J.W., Tran, A.T. et al. Mega-granuloma After Using the Universal Clamp for Adolescent Idiopathic Scoliosis: What Is It and Can It Be Prevented?. Spine Deform 2, 392–398 (2014). https://doi.org/10.1016/j.jspd.2014.04.009
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2014.04.009