Abstract
Study Design
A reliability analysis of Cobb angle, vertebral rotation (VR), and spinous process angle (SPA) measurements in adolescent idiopathic scoliosis.
Objective
To determine the intra- and interobserver reliability of semi-automated digital radiograph measurements.
Summary of Background Data
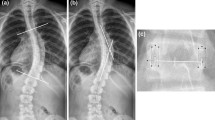
Cobb angle measurements on posteroanterior radiographs are commonly used to determine the severity of scoliosis. Vertebral rotation helps assess scoliosis 3-dimensionally and has a role in predicting curve progression. Recent studies have shown that the spinous process angle is a useful parameter in assessing scoliosis when using ultrasound imaging. Because the reliability of SPA measurements on radiographs has yet to be determined, it is important to compare the reliability of these 3 parameters (Cobb angle, VR, and SPA) using a computer assisted semi-automated method.
Methods
Sixty posteroanterior radiographs of patients with adolescent idiopathic scoliosis were obtained and measured twice by 3 observers who were blinded to their previous measurements, using an in-house developed program. Measurements were obtained using a semi-automated method to minimize variability resulting from observer reliability. The intra- and interobserver reliabilities were analyzed using intra-class correlation coefficients (ICCs) as well as BlandeAltman’s bias and limits of agreement.
Results
Over 350 (intra) and 90 (inter) sets of curves with an average Cobb angle of 26° ± 9° (range, 10° to 44°) were compared for each parameter. Intra-observer reliabilities for each parameter were excellent (ICC[2,1],.82; 1.00), with mean absolute differences under 3° between most measurements. Interobserver reliability (ICC[2,1],.72;.95) was mostly good to excellent, with mean absolute differences ranging from 2.0° to 5.6°.
Conclusions
Both the intra- and interobserver assessment of the Cobb, VR, and SPA from the semi-automated measurements had clinically acceptable reliability ranges and may be considered for clinical implementation. Additional studies will be conducted to determine the accuracy and sensitivity to change of these scoliosis severity measurements.
Similar content being viewed by others
References
Tanure MC, Pinheiro AP, Oliveira AS. Reliability assessment of Cobb angle measurements using manual and digital methods. Spine J 2010;10:769–74.
Zhang J, Lou E, Hill D, et al. Computer-aided assessment of scoliosis on posteroanterior radiographs. Med Biol Eng Comput 2010;48:185–95.
Gstoettner M, Sekyra K, Walochnik N, et al. Inter- and intraobserver reliability assessment of the Cobb angle: manual versus digital measurement tools. Eur Spine J 2007;16:1587–92.
Kuklo TR, Potter BK, O’Brien MF, et al. Reliability analysis for digital adolescent idiopathic scoliosis measurements. J Spinal Disord Tech 2005;18:15–9.
Wills BP, Auerbach JD, Zhu X, et al. Comparison of Cobb angle measurement of scoliosis radiographs with preselected end vertebrae: traditional versus digital acquisition. Spine (Phila Pa 1976) 2007;32:98–105.
Chen YL, Chen WJ, Chiou WK. An alternative method for measuring scoliosis curvature. Orthopedics 2007;30:828–31.
Stokes IAF, Aronsson DD. Computer-assisted algorithms improve reliability of King classification and Cobb angle measurement of scoliosis. Spine (Phila Pa 1976) 2006;31:665–70.
Allen S, Parent E, Khorasani M, et al. Validity and reliability of active shape models for the estimation of Cobb angle in patients with adolescent idiopathic scoliosis. J Digit Imaging 2008;21:208–18.
Mok JM, Berven SH, Diab M, et al. Comparison of observer variation in conventional and three digital radiographic methods used in the evaluation of patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2008;33:681–6.
Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am 1984;66:1061–71.
Drerup B. Principles of measurement of vertebral rotation from frontal projections of the pedicles. J Biomech 1984;17:923–35.
Kuklo T, Potter BK, Lawrence L. Vertebral rotation and thoracic torsion in adolescent idiopathic scoliosis: what is the best radiographic correlate? J Spinal Disord Tech 2005;18:139–47.
Perdriolle R, Vidal J. Thoracic idiopathic scoliosis curve evolution and prognosis. Spine (Phila Pa 1976) 1985;10:785–91.
Weinstein SL, Ponseti I. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 1983;65:447–55.
Heidari B, Fitzpatrick D, McCormack D, et al. Correlation of an induced rotation model with the clinical categorisation of scoliotic deformity—a possible platform for prediction of scoliosis progression. Stud Health Technol Inform 2006; 123:169.
Cheung J, Veldhuizen AG, Haiberts JP, et al. Geometric and electromyographic assessments in the evaluation of curve progression in idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:322–9.
Lam GC, Hill DL, Le LH, et al. Vertebral rotation measurement: a summary and comparison of common radiographic and CT methods. Scoliosis 2008;3:16.
Sugimoto Y, Tanaka M, Nakanishi K, et al. Predicting intraoperative vertebral rotation in patients with scoliosis using posterior elements as anatomical landmarks. Spine (Phila Pa 1976) 2007;32:761–3.
Krawczyński A, Kotwicki T, Szulc A, et al. Clinical and radiological assessment of vertebral rotation in idiopathic scoliosis. Ortop Traumatol Rehabil 2006;8:602.
Stokes IAF, Bigalow LC, Moreland MS. Measurement of axial rotation of vertebrae in scoliosis. Spine (Phila Pa 1976) 1986;11:213–8.
Nash CL, Moe J. A study of vertebral rotation. J Bone Joint Surg Am 1969;51:223–9.
Perdriolle R, Vidal J. Thoracic idiopathic scoliosis curve evaluation and prognosis. Spine (Phila Pa 1976) 1985;10:785–91.
Herzenberg JE, Waanders NA, Closkey RF, et al. Cobb angle versus spinous process angle in adolescent idiopathic scoliosis the relationship of the anterior and posterior deformities. Spine (Phila Pa 1976) 1990;15:874–9.
Chen W, Le L, Lou E. Ultrasound imaging of spinal vertebrae to study scoliosis. Open J Acoust 2012;2:95–103.
Li M, Cheng J, Ying M, et al. Application of 3-D ultrasound in assisting the fitting procedure of spinal orthosis to patients with adolescent idiopathic scoliosis. Stud Health Technol Inform 2010;158:34–7.
Li M, Cheng J, Ying M, et al. Could clinical ultrasound improve the fitting of spinal orthosis for the patients with AIS? Eur Spine J 2012;21:1926–35.
Suzuki S, Yamamuro T, Shikata J, et al. Ultrasound measurement of vertebral rotation in idiopathic scoliosis. J Bone Joint Surg Br 1989;7:252–5.
Chen W, Lou EH, Zhang PQ, et al. Reliability of assessing the coronal curvature of children with scoliosis by using ultrasound images. J Pediatr Orthop 2013:1–9.
Portney LG, Watkins MP. Foundations of clinical research. New Jersey: Pearson/Prentice Hall; 1993.
Currier P. Elements of research in physical therapy. Baltimore: Williams & Wilkins; 1990.
Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res 1999;8:135–60.
Stratford PW, Goldsmith CH. Use of the standard error as a reliability index of interest: an applied example using elbow flexor strength data. Phys Ther 1997;77:745–50.
Pinheiro AP, Tanure MC, Oliveira AS. Validity and reliability of a computer method to estimate vertebral axial rotation from digital radiographs. Eur Spine J 2010;19:415–20.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: ACYC (none); DGM (none); DVN (none); DLH (none); EP (none); EHM L (none).
This work was supported by the Alberta Innovates Health Solutions, Women’s and Children’s Health Research Institute.
Rights and permissions
About this article
Cite this article
Chan, A.C.Y., Morrison, D.G., Nguyen, D.V. et al. Intra- and Interobserver Reliability of the Cobb AngleeVertebral Rotation Angle—Spinous Process Angle for Adolescent Idiopathic Scoliosis. Spine Deform 2, 168–175 (2014). https://doi.org/10.1016/j.jspd.2014.02.006
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2014.02.006