Abstract
Study Design
Retrospective sequential patient series.
Objectives
To establish the relationship between the magnitude of the deformity in scoliosis and patients’ perception of their condition, as measured with Scoliosis Research Society-22 scores.
Methodology
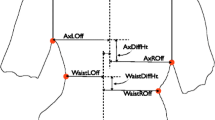
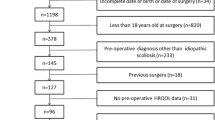
A total of 93 untreated patients with adolescent idiopathic scoliosis were included retrospectively. The Cobb angle was measured from a plain radiograph, and volumetric asymmetry was measured by ISIS2 surface topography. The association between Scoliosis Research Society scores for function, pain, self-image, and mental health against Cobb angle and volumetric asymmetry was investigated using the Pearson correlation coefficient.
Results
Correlation of both Cobb angle and volumetric asymmetry with function and pain was weak (all <.23); these correlation values were not statistically significant. Correlation of Cobb angle and volumetric asymmetry with self-image, was higher, although still moderate (-.37 for Cobb angle and -.44 for volumetric asymmetry). Both were statistically significant (Cobb angle, p =.0002; volumetric asymmetry; p =.00001). Cobb angle contributed 13.8% to the linear relationship with self-image, whereas volumetric asymmetry contributed 19.3%. For mental health, correlation was statistically significant with Cobb angle (p =.011) and volumetric asymmetry (p =.0005), but the correlation was low to moderate (-.26 and -.35, respectively). Cobb angle contributed 6.9% to the linear relationship with mental health, whereas volumetric asymmetry contributed 12.4%.
Conclusions
Volumetric asymmetry correlates better with both mental health and self-image compared with Cobb angle, but the correlation was only moderate. This study suggests that a patient’s own perception of self-image and mental health is multifactorial and not completely explained through present objective measurements of the size of the deformity. This helps to explain the difficulties in any objective analysis of a problem with multifactorial perception issues. Further study is required to investigate other physical aspects of the deformity that may have a role in how patients view themselves.
Similar content being viewed by others
References
Cobb J. Outline for the study of scoliosis. AAOS Instr Course Lect 1948;5:261–75.
Aaro S, Dahlborn M. The longitudinal axis rotation of the apical vertebra, the vertebral, spinal, and rib cage deformity in idiopathic scoliosis studied by computer tomography. Spine 1981;6:567–72.
Burwell R, James N, Johnson F, et al. Standardised trunk asymmetry scores: a study of back contour in healthy school children. J Bone Joint Surg Br 1983;65:452–63.
Erkula G, Sponseller PD, Kiter AE. Rib deformity in scoliosis. Eur Spine J 2003;12:281–7.
Geissele AE, Ogilvie JW, Cohen M, et al. Thoracoplasty for the treatment of rib prominence in thoracic scoliosis. Spine 1994;19: 1636–42.
Thulbourne T, Gillespie R. The rib hump in idiopathic scoliosis: measurement, analysis and response to treatment. J Bone Joint Surg Br 1976;58:64–71.
Oxborrow N. Assessing the child with scoliosis: the role of surface topography. Arch Dis Child 2000;83:453–5.
Doody M, Lonstein JE, Stovall M, et al. Breast cancer mortality after diagnostic radiography: findings from the US Scoliosis Cohort Study. Spine 2000;25:2052–63.
Preston DL, Mattsson A, Holmberg E, et al. Radiation effects on breast cancer risk: a pooled analysis of eight cohorts. Radiat Res 2002;158:220–35.
Ronckers CM, Doody MM, Lonstein JE, et al. Multiple diagnostic X- rays for spine deformities and risk of breast cancer. Breast Cancer Res 2005;17:605–13.
Berryman F, Pynsent P, Fairbank J, et al. A new system for measuring three-dimensional back shape in scoliosis. Eur Spine J 2008;17: 663–72.
Frobin W, Hierholzer E. Video rasterstereography: a method for online measurement of body surfaces. Photogramm Eng Remote Sensing 1991;57:1341–5.
Goldberg CJ, Kaliszer M, Moore DP, et al. Surface topography, Cobb angles, and cosmetic change in scoliosis. Spine 2001;26:E55–63.
Theologis TN, Fairbank JCT, Turner-Smith AR, et al. Early detection of progression in adolescent idiopathic scoliosis by measurement of changes in back shape with the integrated shape imaging system scanner. Spine 1997;22:1223–7.
Turner-Smith AR, Harris J, Houghton G, et al. A method for analysis of back shape in scoliosis. J Biomech 1988;21:497–509.
Labelle H, Aubin CE, Jackson R, et al. Seeing the spine in 3D: how will it change what we do? J Pediatr Orthoped 2011;31:S37–45.
Sangole AP, Aubin CE, Labelle H, et al. Three-dimensional classification of thoracic scoliotic curves. Spine 2009;34:91–9.
Smith F, Latchford G, Hall R, et al. Indications of disordered eating behaviour in adolescent patients with idiopathic scoliosis. J Bone Joint Surg Br 2002;84:392–4.
Payne III WK, Ogilvie JW, Resnick MD, et al. Does scoliosis have a psychological impact and does gender make a difference? Spine 1997;22:1380–4.
Haher TR, Gorup JM, Shin TM, et al. Results of the Scoliosis Research Society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis: a multicenter study of 244 patients. Spine 1999;24:1435–40.
Asher M, Min Lai S, Burton D, et al. The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine 2003;28:63–9.
Asher M, Min Lai S, Burton D, et al. Discrimination validity of the scoliosis research society-22 patient questionnaire: relationship to idiopathic scoliosis curve pattern and curve size. Spine 2003;28:74–7.
Asher M, Min Lai S, Burton D, et al. Scoliosis Research Society-22 patient questionnaire: responsiveness to change associated with surgical treatment. Spine 2003;28:70–3.
Asher MA, Min Lai S, Burton DC. Further development and validation of the Scoliosis Research Society (SRS) outcomes instrument. Spine 2000;25:2381–6.
Asher M, Min Lai S, Burton DC, et al. The influence of spine and trunk deformity on preoperative idiopathic scoliosis patients’ health-related quality of life questionnaire responses. Spine 2004;29:861–8.
Parent EC, Hill D, Mahood J, et al. Discriminative and predictive validity of the Scoliosis Research Society-22 Questionnaire in management and curve-severity subgroups of adolescents with idiopathic scoliosis. Spine 2009;34:2450–7.
Inami K, Suzuki N, Ono T, et al. Analysis of posterior trunk symmetry index (POTSI) in scoliosis: part 2. In: Stokes IAF, editor. Research into spinal deformities 2. Amsterdam: IOS Press; 1999. p. 85—8.
Suzuki N, Inami K, Ono T, et al. Analysis of posterior trunk symmetry index (POTSI) in scoliosis: part 1. In: Stokes IAF, editor. Research into spinal deformities 2. Amsterdam: IOS Press; 1999. p. 81—4.
Suzuki N, Ono T, Tezuka M, et al. Moire topography and back shape analysis: clinical application. In: Dansereau J, editor. International symposium on 3-D scoliotic deformity. Montreal: Fisher Verlag; 1992. p. 124–30.
Berryman F, Pynsent P, Fairbank J. Variability in transverse volumetric asymmetry measurements in ISIS2. J Bone Joint Surg Br 2009;91(SUPP III):484.
Jackson SL. Research methods and statistics: a critical thinking approach. 4th ed. Belmont, CA: Wadsworth; 2011. p69.
R Development Core Team. R: A language and environment for statistical computing. R Foundation or statistical computing. Available: http://www.R-project.org; 2009.
D’Andrea LP, Betz RR, Lenke LG, et al. Do radiographic parameters correlate with clinical outcomes in adolescent idiopathic scoliosis? Spine 2000;25:1795–802.
Helenius I, Remes V, Yrjonen T, et al. Comparison of long-term functional and radiologic outcomes after Harrington instrumentation and spondylodesis in adolescent idiopathic scoliosis: a review of 78 patients. Spine 2002;27:176–80.
Rinella A, Lenke L, Peelle M, et al. Comparison of SRS questionnaire results submitted by both parents and patients in the operative treatment of idiopathic scoliosis. Spine 2004;29:303–10.
White SF, Asher MA, Lai SM, et al. Patients’ perceptions of overall function, pain, and appearance after primary posterior instrumentation and fusion for idiopathic scoliosis. Spine 1999;24: 1693–700.
Tones M, Moss N, Polly Jr DW. A review of quality of life and psychosocial issues in scoliosis. Spine 2006;31:3027–38.
Watanabe K, Hasegawa K, Hirano T, et al. Use of the Scoliosis Research Society outcomes instrument to evaluate patient outcome in untreated idiopathic scoliosis patients in Japan. Part II: relation between spinal deformity and patient outcomes. Spine 2005;30: 1202–5.
Clayson D, Mahon B, Levine DB. Preoperative personality characteristics as predictors of postoperative physical and psychological patterns in scoliosis. Spine 1981;6:9–12.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: PB (none); FB (salary paid from a grant from Smith & Nephew on hip joints); DB (none); PP (grant from Smith & Nephew; royalties from Books Editor); AG (consultancy for Medtronic; expert testimony for medicolegal practice—AC Gardner Ltd; payment for lectures including service on speakers bureaus from Medtronic, DePuy Synthes Spine; payment for development of educational presentations from Medtronic; travel/accommodations/meeting expenses from Medtronic).
Rights and permissions
About this article
Cite this article
Brewer, P., Berryman, F., Baker, D. et al. Influence of Cobb Angle and ISIS2 Surface Topography Volumetric Asymmetry on Scoliosis Research Society-22 Outcome Scores in Scoliosis. Spine Deform 1, 452–457 (2013). https://doi.org/10.1016/j.jspd.2013.07.012
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2013.07.012