Abstract
Study Design
Retrospective case series.
Objective
To assess the perioperative morbidity of pedicle subtraction osteotomy (PSO) based on the presence of 1 versus 2 attending surgeons.
Background Summary
Pedicle subtraction osteotomies are challenging cases with high complication rates and substantial physiological burden on patients. The literature supports the benefits of 2-surgeon strategies in complex cases in other specialties.
Methods
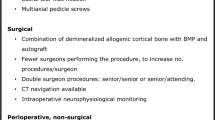
We reviewed a single institution database of all pedicle subtraction osteotomies (78 cases) from 2005–2010 and divided the cohort into single versus 2-surgeon groups (42 vs. 36 cases, respectively). We performed subset analysis after excluding cases before 2007 and excluding patients with staged anterior and posterior procedures.We analyzed cases for estimated blood loss, length of surgery, length of stay, radiographic analysis, rate of return to the operating room within 30 days, and medical and neurological complications.
Results
The groups were similar when comparing mean number of posterior levels fused, levels decompressed and revision rates, however, the average age of the single surgeon and 2 surgeon groups was 57.6 and 64.3 years, respectively (p =.02). The 2 groups had comparable correction of radiographic parameters. Mean percent estimated blood loss for single versus 2 surgeons was 109% versus 35% (p!.001) and estimated blood loss was 5,278 versus 2,003 mL (p <.001). Average surgical time for single versus 2 surgeons was 7.6 versus 5.0 hours (p <.001). A total of 45% of single-surgeon patients compared with 25% of 2-surgeon patients experienced at least 1 major complication within 30 days. In the single-surgeon group, 19% had unplanned surgery within 30 days, versus 8% in the 2-surgeon group.
Conclusions
The use of 2 surgeons at an experienced spine deformity center decreases the operative time and estimated blood loss, and may be a key factor in witnessed decreased major complication prevalence. This approach also may decrease the rate of premature case termination and return to operating room in 30 days.
Similar content being viewed by others
References
Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024–9.
Schwab F, Lafage V, Farcy JP, et al. Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis: Application of the new adult deformity classification. Spine (Phila Pa 1976) 2007;32:2723–30.
Buchowski JM, Bridwell KH, Lenke LG, et al. Neurologic complications of lumbar pedicle subtraction osteotomy: A 10-year assessment. Spine (Phila Pa 1976) 2007;32:2245–52.
Dorward IG, Lenke LG. Osteotomies in the posterior-only treatment of complex adult spinal deformity: A comparative review. Neurosurg Focus. Mar;28(3):E4.
Ikenaga M, Shikata J, Takemoto M, et al. Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine 2007;6:330–6.
Kim KT, Suk KS, Cho YJ, et al. Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine (Phila Pa 1976) 2002;27:612–8.
Kim YJ, Bridwell KH, Lenke LG, et al. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: A minimum 5-year follow-up study. Spine (Phila Pa 1976) 2007;32:2189–97.
Murrey DB, Brigham CD, Kiebzak GM, et al. Transpedicular decompression and pedicle subtraction osteotomy (eggshell procedure): A retrospective review of 59 patients. Spine (Phila Pa 1976) 2002;27:2338–45.
Yang BP, Ondra SL, Chen LA, et al. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine 2006;5:9–17.
Bridwell KH, Lewis SJ, Edwards C, et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine (Phila Pa 1976) 2003;28:2093–101.
Bridwell KH, Lewis SJ, Lenke LG, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am 2003;85:454–63.
Chen IH, Chien JT, Yu TC. Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis: Experience with 78 patients. Spine (Phila Pa 1976) 2001;26: E354–60.
Cho KJ, Bridwell KH, Lenke LG, et al. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine (Phila Pa 1976) 2005;30:2030–7; discussion 8.
Kiaer T, Gehrchen M. Transpedicular closed wedge osteotomy in ankylosing spondylitis: Results of surgical treatment and prospective outcome analysis. Eur Spine J 2010;19:57–64.
Lazennec JY, Neves N, Rousseau MA, et al. Wedge osteotomy for treating post-traumatic kyphosis at thoracolumbar and lumbar levels. J Spinal Disord Tech 2006;19:487–94.
van Loon PJ, van Stralen G, van Loon CJ, et al. A pedicle subtraction osteotomy as an adjunctive tool in the surgical treatment of a rigid thoracolumbar hyperkyphosis: A preliminary report. Spine J 2006;6:195–200.
Gurtner GC, Robertson CS, Chung SC, et al. Two-team synchronous oesophagectomy. Br J Surg 1994;81:1620–2.
Saithna A, Arbuthnot J, Carey-Smith R, et al. Simultaneous bilateral anterior cruciate ligament reconstruction: A safe option. Knee Surg Sports Traumatol Arthrosc 2010;18:1071–4.
Skinner A, Maoate K, Beasley S. Retroperitoneal laparoscopic nephrectomy: The effect of the learning curve, and concentrating expertise, on operating times. J Laparoendosc Adv Surg Tech A 2010;20:383–5.
Glassman SD, Hamill CL, Bridwell KH, et al. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 2007;32:2764–70.
Berven SH, Deviren V, Smith JA, et al. Management of fixed sagittal plane deformity: Results of the transpedicular wedge resection osteotomy. Spine (Phila Pa 1976) 2001;26:2036–43.
Lehmer SM, Keppler L, Biscup RS, et al. Posterior transvertebral osteotomy for adult thoracolumbar kyphosis. Spine (Phila Pa 1976) 1994;19:2060–7.
Mummaneni PV, Dhall SS, Ondra SL, et al. Pedicle subtraction osteotomy. Neurosurgery 2008;63(suppl):171–6.
Danisa OA, Turner D, Richardson WJ. Surgical correction of lumbar kyphotic deformity: Posterior reduction “eggshell” osteotomy. J Neurosurg 2000;92(suppl):50–6.
Blam OG, Vaccaro AR, Vanichkachorn JS, et al. Risk factors for surgical site infection in the patient with spinal injury. Spine (Phila Pa 1976) 2003;28:1475–80.
Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: Preliminary clinical results. J Neurosurg 2002;97(suppl):7–12.
Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. Clin Neurosurg 2002;49:499–517.
Guiot BH, Khoo LT, Fessler RG. A minimally invasive technique for decompression of the lumbar spine. Spine (Phila Pa 1976) 2002;27:432–8.
Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2003;28(suppl):S26–35.
German JW, Foley KT. Minimal access surgical techniques in the management of the painful lumbar motion segment. Spine (Phila Pa 1976) 2005;30(suppl):S52–9.
Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine (Phila Pa 1976) 2007;32:537–43.
Peng CW, Yue WM, Poh SY, et al. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2009;34:1385–9.
Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): Technical feasibility and initial results. J Spinal Disord Tech 2005;18(suppl): S1–6.
Shunwu F, Xing Z, Fengdong Z, et al. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976) 2010;35:1615–20.
Fang A, Hu SS, Endres N, et al. Risk factors for infection after spinal surgery. Spine (Phila Pa 1976) 2005;30:1460–5.
Simchen E, Stein H, Sacks TG, et al. Multivariate analysis of determinants of postoperative wound infection in orthopaedic patients. J Hosp Infect 1984;5:137–46.
Wimmer C, Gluch H, Franzreb M, et al. Predisposing factors for infection in spine surgery: A survey of 850 spinal procedures. J Spinal Disord 1998;11:124–8.
Watanabe M, Sakai D, Matsuyama D, et al. Risk factors for surgical site infection following spine surgery: Efficacy of intraoperative saline irrigation. J Neurosurg Spine 2010;12:540–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: CPA (consulting for DePuy, Medtronic, Stryker; employment by University of California—San Francisco; grant from Trans1; patents from Fish & Richardson, PC; royalties from AESCULAP, LAWX; stock options: Trans1, Doctors Research Group, Visulase all less than 1%); JJB (none); SK (none); OD (none); MHW (none); VD (honorarium and consulting for Stryker, NuVasive, Guidepoint, and Medtronic).
Rights and permissions
About this article
Cite this article
Ames, C.P., Barry, J.J., Keshavarzi, S. et al. Perioperative Outcomes and Complications of Pedicle Subtraction Osteotomy in Cases With Single Versus Two Attending Surgeons. Spine Deform 1, 51–58 (2013). https://doi.org/10.1016/j.jspd.2012.10.004
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2012.10.004