Abstract
Study Design
Retrospective case series.
Objectives
To report the complications and outcomes of pediatric revision spine surgery and review the surgical indications and treatment methods.
Background Summary
Recent reports have shown the necessity of revision spine surgery for pediatric deformities. Many reports have shown the result of revision surgery for pediatric spinal deformity.
Materials and Methods
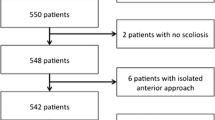
We conducted a retrospective review of 638 patients with pediatric spinal deformity who were treated with surgery from 1996 to 2007.We identified 50 patients who underwent revision spinal fusion surgery with a minimum of 3 years of follow-up.
Results
Mean follow-up was 4 years (range, 3–8.3 years). The diagnosis at index surgery was idiopathic scoliosis in 18 patients, congenital scoliosis in 13, neuromuscular scoliosis in 13, tumor and spinal arteriovenous malformation in 4, burst fracture in thoracic spine in 1, and Scheuermann kyphosis in 1. The primary surgeries were 1 hemi epiphysiodesis, 3 anterior spinal fusions, 4 posterior decompressions, 8 combined anterior and posterior spinal fusions, and 34 posterior spinal fusions. A total of 16 patients had pseudarthrosis, 12 decompensation, 11 progressive kyphosis, 8 crankshaft phenomenon, 2 infections, and 1 junctional degeneration. All 50 reoperations included spinal instrumentation and fusion. The revision surgeries were 2 anterior spinal fusions, 14 posterior fusions, and 34 combined anterior and posterior spinal fusions. Spine arthrodesis was obtained in 98% of patients (49 of 50) and complications occurred in 14% of patients (7 of 50). The Scoliosis Research Society Patient Questionnaire outcomes at the latest follow-up were as follows: total 3.95, function 3.88, pain 3.83, self-image 3.98, and mental health 4.04.
Conclusion
Pseudarthrosis was the most common indication for revision surgery, and bony union was achieved in 98% with revision surgery. Despite the complications, pediatric revision spine surgery can achieve successful outcomes.
Similar content being viewed by others
References
Benli IT, Duman E, Akalin S, et al. [An evaluation of the types and the results of surgical treatment for congenital scoliosis]. Acta Orthop Traumatol Turc 2003;37:284–98.
Bernard Jr TN, Burke SW, Johnston III CE, et al. Congenital spine deformities: A review of 47 cases. Orthopedics 1985;8:777–83.
Bowen RE, Scaduto AA, Banuelos S. Does early thoracic fusion exacerbate preexisting restrictive lung disease in congenital scoliosis patients? J Pediatr Orthop 2008;28:506–11.
Coran DL, Rodgers WB, Keane JF, et al. Spinal fusion in patients with congenital heart disease: Predictors of outcome. Clin Orthop Relat Res 1999;364:99–107.
Garrido E, Tome-Bermejo F, Tucker SK, et al. Short anterior instrumented fusion and posterior convex non-instrumented fusion of hemivertebra for congenital scoliosis in very young children. Eur Spine J 2008;17:1507–14.
Griss P, Huberti H. The operative treatment of congenital scoliosis: A review of 26 cases. Arch Orthop Trauma Surg 1981;98:241–6.
Holte DC, Winter RB, Lonstein JE, et al. Excision of hemivertebrae and wedge resection in the treatment of congenital scoliosis. J Bone Joint Surg Am 1995;77:159–71.
Keller PM, Lindseth RE, DeRosa GP. Progressive congenital scoliosis treatment using a transpedicular anterior and posterior convex hemiepiphysiodesis and hemiarthrodesis: A preliminary report. Spine (Phila Pa 1976) 1994;19:1933–9.
McMaster MJ, Singh H. The surgical management of congenital kyphosis and kyphoscoliosis. Spine (Phila Pa 1976) 2001;26:2146–54; discussion 55.
Noordeen MH, Garrido E, Tucker SK, et al. The surgical treatment of congenital kyphosis. Spine (Phila Pa 1976) 2009;34:1808–14.
Shahcheraghi GH, Hobbi MH. Patterns and progression in congenital scoliosis. J Pediatr Orthop 1999;19:766–75.
Smith JT, Gollogly S, Dunn HK. Simultaneous anterior-posterior approach through a costotransversectomy for the treatment of congenital kyphosis and acquired kyphoscoliotic deformities. J Bone Joint Surg Am 2005;87:2281–9.
Uzumcugil A, Cil A, Yazici M, et al. Convex growth arrest in the treatment of congenital spinal deformities, revisited. J Pediatr Orthop 2004;24:658–66.
Winter RB, Lonstein JE. Congenital thoracic scoliosis with unilateral unsegmented bar and concave fused ribs: Rib osteotomy and posterior fusion at 1 year old, anterior and posterior fusion at 5 years old with a 36-year follow-up. Spine (Phila Pa 1976) 2007;32:E841–4.
Gillingham BL, Fan RA, Akbarnia BA. Early onset idiopathic scoliosis. J Am Acad Orthop Surg 2006;14:101–12.
Thacker M, Hui JH, Wong HK, et al. Spinal fusion and instrumentation for paediatric neuromuscular scoliosis: Retrospective review. J Orthop Surg (Hong Kong) 2002;10:144–51.
Vitale MG, Matsumoto H, Bye MR, et al. A retrospective cohort study of pulmonary function, radiographic measures, and quality of life in children with congenital scoliosis: An evaluation of patient outcomes after early spinal fusion. Spine (Phila Pa 1976) 2008;33:1242–9.
Agabegi SS, Antekeier DP, Crawford AH, Crone KR. Postlaminectomy kyphosis in an achondroplastic adolescent treated for spinal stenosis. Orthopedics 2008;31:168.
Kesling KL, Lonstein JE, Denis F, et al. The crankshaft phenomenon after posterior spinal arthrodesis for congenital scoliosis: A review of 54 patients. Spine (Phila Pa 1976) 2003;28:267–71.
Hedequist DJ, Hall JE, Emans JB. The safety and efficacy of spinal instrumentation in children with congenital spine deformities. Spine (Phila Pa 1976) 2004;29:2081–6; discussion 7.
Marks DS, Sayampanathan SR, Thompson AG, et al. Long-term results of convex epiphysiodesis for congenital scoliosis. Eur Spine J 1995;4:296–301.
Thompson AG, Marks DS, Sayampanathan SR, et al. Long-term results of combined anterior and posterior convex epiphysiodesis for congenital scoliosis due to hemivertebrae. Spine (Phila Pa 1976) 1995;20:1380–5.
Asher M, Min Lai S, Burton D, Manna B. The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine 2003;28:63–9.
Bago J, Ramirez M, Pellise F, Villanueva C. Survivorship analysis of Cotrel-Dubousset instrumentation in idiopathic scoliosis. Eur Spine J 2003;12:435–9.
Cook S, Asher M, Lai SM, Shobe J. Reoperation after primary posterior instrumentation and fusion for idiopathic scoliosis: Toward defining late operative site pain of unknown cause. Spine (Phila Pa 1976) 2000;25:463–8.
Luhmann SJ, Lenke LG, Bridwell KH, Schootman M. Revision surgery after primary spine fusion for idiopathic scoliosis. Spine (Phila Pa 1976) 2009;34:2191–7.
Dias RC, Miller F, Dabney K, Lipton GE. Revision spine surgery in children with cerebral palsy. J Spinal Disord 1997;10:132–44.
Hell AK, Campbell RM, Hefti F. [New treatment concept for children with thoracic insufficiency syndrome due to congenital spine deformity]. Klin Padiatr 2005;217:268–73.
Thompson GH, Akbarnia BA, Campbell Jr RM. Growing rod techniques in early-onset scoliosis. J Pediatr Orthop 2007;27:354–61.
Suk SI, Kim JH, Cho KJ, et al. Is anterior release necessary in severe scoliosis treated by posterior segmental pedicle screw fixation? Eur Spine J 2007;16:1359–65.
Sarlak AY, Atmaca H, Buluć L, et al. Juvenile idiopathic scoliosis treated with posterior arthrodesis and segmental pedicle screw instrumentation before the age of 9 years: A 5-year follow-up. Scoliosis 2009;4:1.
Eccher M. Intraoperative neurophysiologic monitoring: are we really that bad? J Clin Neurophysiol 2012;29:157–9.
Gavaret M, Tréebuchon A, Aubert S, Jacopin S, Blondel B. Intraoperative monitoring in pediatric orthopedic spinal surgery: three hundred consecutive monitoring cases of which 10% of patients were younger than 4 years of age. Spine 2011;36:1855–63.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures:MY(none); ABK (none); HJK (none); MEC (none); OB (royalties from DePuy and K2M, Inc.; development of presentations for DePuy and K2M Inc; other support from Osteotech, K2M Inc, and DePuy).
Rights and permissions
About this article
Cite this article
Yagi, M., King, A.B., Kim, H.J. et al. Outcome of Revision Surgery in Pediatric Spine Deformity Patients. Spine Deform 1, 59–67 (2013). https://doi.org/10.1016/j.jspd.2012.10.002
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2012.10.002