Abstract
Study Design
Biomechanical pullout study using calcium triglyceride (CTG) and polymethylmethacrylate (PMMA) for screw augmentation.
Objective
Compare the biomechanical performance of CTG augmentation versus the gold standard, PMMA, in primary and revision models, using a pedicle screw pullout model.
Background Summary
CTG is a novel form of bone augmentation with several reported biocompatible properties compared with PMMA. PMMA is the standard of care for pedicle screw augmentation in osteoporotic spine.
Methods
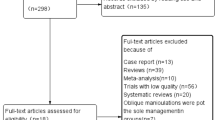
Blocks of closed-cell rigid polyurethane foam of uniform density, representing subcortical layer in osteoporotic pedicle, were prepared according to ASTM standards. After the components of PMMA (n 5 11) and CTG (n 5 11) were individually mixed in a standardized fashion, 0.2 ml was injected from deep to superficial along a predrilled pilot hole followed by immediate insertion of the pedicle screw. An unaugmented group (n 5 10) was also prepared. Blocks cured for 24 hrs, and screws were pulled out at a rate of 5 mm/ min on materials testing equipment. For the revision model, the unaugmented group, after screw pullout, was augmented with 0.8 ml of PMMA (n 5 5) or CTG (n 5 5) as detailed above and screw pullout performed similarly.
Results
The mean pullout strengths (SD) for the intact models were as follows: unaugmented, 976.6 N (94.2 N); PMMA, 1,218.1 N (66.8 N); and CTG, 1,841.6 N (57.4 N). A one-way analysis of variance indicated a significant difference among the primary models (p <.0001). For the revision models, the pullout strength for PMMA was 1,939.2 N (108.9 N) and for CTG, 2,513.0 N (149.1 N), which were statistically different from each other (p <.0003). Stiffness of the constructs was increased with both PMMA and CTG augmentation over no augmentation (p <.0001) although no significant difference in stiffness was detected between the 2 forms of augmentation.
Conclusion
We conclude that CTG augmentation of pedicle screws resulted in significantly higher axial pullout strength in primary (p <.0001) and revision (p <.0003) models compared with PMMA.
Similar content being viewed by others
References
Hirano T, Hasegawa K, Takahashi HE, et al. Structural characteristics of the pedicle and its role in screw stability. Spine 1997;22:2504–9. discussion 2510.
Cho W, Cho SK, Wu C. The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg Br 2010;92:1061–5. Review.
Wittenberg RH, Shea M, Swartz DE, et al. Importance of bone mineral density in instrumented spine fusions. Spine 1991;16:647–52.
Renner SM, Lim TH, Kim WJ, et al. Augmentation of pedicle screw fixation strength using an injectable calcium phosphate cement as a function of injection timing and method. Spine 2004;29:E212–6.
Jaeblon T. Polymethylmethacrylate: Properties and contemporary uses in orthopaedics. J Am Acad Orthop Surg 2010;18:297–305. Review.
Chang MC, Liu CL, Chen TH. Polymethylmethacrylate augmentation of pedicle screw for osteoporotic spinal surgery: a novel technique. Spine 2008;33:E317–24.
Abu-Amer Y, Clohisy JC. The biologic response to orthopaedic implants. In: Einhorn TA, O’Keefe RJ, Buckwalter JA, editors. Orthopaedic Basic Science: Foundations of Clinical Practice 3rd Ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2007. p. 365–75.
Jannetty J, Kolb E, Boxberger J, et al. Guiding Bone Formation in a Critical-Sized Defect and Assessments. J Craniofac Surg 2010;21:1848–54.
Fedak PW, Kolb E, Borsato G, et al. Kryptonite Bone Cement Prevents Pathological Sternal Displacement. Ann Thorac Surg 2010;90:979–85.
Adams DJ, Barrero M, Jiang X. Persistent osteoconductivity of calcium triglyceride bone cement in osteoporotic bone. Transactions of the 54th Annual Meeting of the Orthopaedic Research Society; 2008:1718.
ASTM F1839-08, “Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments”. West Conshohocken, PA: ASTM International; 2008.
ASTM F543-07, “Standard specification and Test Methods for Metallic Medical Bone Screws”. West Conshohocken, PA: ASTM international; 2007.
di Nuzzo G, Luongo M, Parlato C, et al. Cranial reconstruction using bioabsorbable calcified triglyceride bone cement. J Craniofac Surg 2010;21:1170–4.
Chapman JR, Harrington RM, Lee KM, et al. Factors affecting the pullout strength of cancellous bone screws. J Biomech En 1996;118:391–8.
Patel PS, Shepherd DE, Hukins DW. The effect of screw insertion angle and thread type on the pullout strength of bone screws in normal and osteoporotic cancellous bone models. Med Eng Phy 2010;32:822–8.
Nakashima H, Yukawa Y, Imagama S, et al. Complications of cervical pedicle screw fixation for nontraumatic lesions: a multicenter study of 84 patients. J Neurosurg Spine 2012;16:238–47.
Adams DJ, Diaz-Doran V. Mechanical efficacy of calcium triglyceride bone cement for pedicle screw augmentation. Transactions of the 55th Annual Meeting of the Orthopaedic Research Society 2009;34:1759.
McLachlin SD, Al Saleh K, Gurr KR, et al. Comparative assessment of sacral screw loosening augmented with PMMA versus a calcium triglyceride bone cement. Spine 2011;36:E699–704.
Author information
Authors and Affiliations
Corresponding author
Additional information
FDA drug/device status: Calcium triglyceride bone cement is FDA approved for cranioplasty applications.
Author disclosures: LEH (none); JRO (none); JSW (grants to institution from Ascension Orthopedics and EB Ortho; travel accommodations from ORS); HRT (royalties from and consulting for Amedica; board membership; consulting for and stock ownership in Doctor’s Research Group; and patents with US Spine).
Rights and permissions
About this article
Cite this article
Hickerson, L.E., Owen, J.R., Wayne, J.S. et al. Calcium Triglyceride Versus Polymethylmethacrylate Augmentation: A Biomechanical Analysis of Pullout Strength. Spine Deform 1, 10–15 (2013). https://doi.org/10.1016/j.jspd.2012.07.004
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2012.07.004