Abstract
Objective
At present it is unclear whether endothelial activation is systematically present in preeclampsia or restricted to specialized vascular beds. Therefore, this study aimed to investigate the presence of generalized proinflammatory endothelial activation in severe, early-onset preeclampsia in vivo.
Methods
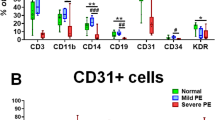
During caesarean section, biopsies were obtained from abdominal subcutaneous fat, abdominal fascia, and myometrium from 11 severe, early-onset preeclamptic and 19 healthy pregnant women. Prior to caesarean, section plasma levels of von Willebrand Factor (vWF), sVCAM-1, and C-reactive protein (CRP) were measured by ELISA. Consecutive cryostat sections were stained immunohistochemically for CD31, E-selectin, VCAM-1, and ICAM-1. For subcutaneous fat tissue, endothelial gene expression levels of E-selectin, VCAM-1, ICAM-1, endothelin-1 (ET-1), and endothelial nitric oxide synthase (eNOS) were quantified by real-time RT-PCR, using normalization to the endothelium-specific housekeeping genes CD31 and VE-cadherin.
Results
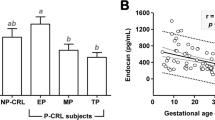
Plasma levels of vWF, sVCAM-1, and CRP were elevated in the preeclampsia group compared to the control group, indicating enhanced endothelial activation and inflammatory response in the severely diseased preeclamptic women. By immunohistochemical analysis, no E-selectin and VCAM-1 expression could be detected in, and no differences in endothelial ICAM-1 staining could be observed between the preeclampsia and the control group for all tissues studied. Endothelial gene expression levels of E-selectin, VCAM-1, ICAM-1, ET-1, and eNOS were comparable between the preeclampsia and control group.
Conclusion
Protein and gene expression analysis of E-selectin, VCAM-1, ICAM-1, ET-1, and eNOS, key mediators involved in pro-inflammatory endothelial activation, could not identify endothelial activation in severe, early-onset preeclampsia in the tissues studied. However, elevated plasma levels of markers of endothelial activation and inflammation were observed. These results may suggest that in severe, early-onset preeclampsia pro-inflammatory endothelial cell activation is not a generalized phenomenon, but is likely restricted to (possibly organ-specific) specialized vascular beds.
Similar content being viewed by others
References
Roberts JM. Pregnancy related hypertension. In: Creasy RK, Reyes A, eds. Maternal fetal medicine. Philadelphia: Saunders; 1998;833–872.
Odegard RA, Vatten LJ, Nilsen ST, Salvesen KA, Austgulen R. Preeclampsia and fetal growth. Obstet Gynecol 2000;96:950–955.
Roberts JM, Lain KY. Recent Insights into the pathogenesis of pre-eclampsia. Placenta 2002;23:359–372.
Aardema MW, Saro MC, Lander M, De Wolf BT, Oosterhof H, Aarnoudse JG. Second trimester Doppler ultrasound screening of the uterine atteries differentiates between subsequent normal and poor outcomes of hypertensive pregnancy: Two different pathophysiological entities? Clin Sci (Lond) 2004;106:377–382.
Redman CW, Sargent IL. Pre-eclampsia, the placenta and the maternal systemic inflammatory response-A review. Placenta 2003;24 Suppl A:S21–S27.
Teran E, Escudero C, Moya W, Flores M, Vallance P, Lopez-Jaramillo P. Elevated C-reative protein and pro-inflammatory cytokines in Andean women with pre-eclampsia. Int J Gynaecol Obstet 2001;75:243–249.
Qiu C, Luthy DA, Zhang C, Walsh SW, Leisenring WM, Williams MA. A prospective study of maternal serum C-reactive protein concentrations and risk of preeclampsia. Am J Hypertens 2004;17:154–160.
Madazli R, Aydin S, Uludag S, Vildan O, Tolun N. Maternal plasma levels of cytokines in normal and preeclamptic pregnancies and their relationship with diastolic blood pressure and fibronectin levels. Acta Obstet Gynecol Scand 2003;82:797–802.
Kauma S, Takacs P, Scordalakes C, Walsh S, Green K, Peng T. Increased endothelial monocyte chemoattractant protein-1 and interleukin-8 in preeclampsia. Obstet Gynecol 2002;100:706–714.
Sacks GP, Studena K, Sargent K, Redman CW. Normal pregnancy and preeclampsia both produce inflammatory changes in peripheral blood leukocytes akin to those of sepsis. Am J Obstet Gynecol 1998;179:80–86.
Chaiworapongsa T, Romero R, Yoshimatsu J, et al. Soluble adhesion molecule profile in normal pregnancy and pre-eclampsia. J Matern Fetal Neonat Med 2002;12:19–27.
Austgulen R, Lien E, Vince G, Redman CW. Increased maternal plasma levels of soluble adhesion molecules (ICAM-1, VCAM-1, E-selectin) in preeclampsia. Eur J Obstet Gynecol Reprod Biol 1997;71:53–58.
Leik CE, Walsh SW. Neutrophils infiltrate resistance-sized vessels of subcutaneous fat in women with preeclampsia. Hypertension 2004;44:72–77.
Kuldo JM, Ogawara KI, Werner N, et al. Molecular pathways of endothelial cell activation for (targeted) pharmacological intervention of chronic inflammatory diseases. Curr Vasc Pharmacol 2005;3:11–39.
Aydin S, Benian A, Madazli R, Uludag S, Uzun H, Kaya S. Plasma malondialdehyde, superoxide dismutase, sE-selectin, fibronectin, endothelin-1 and nitric oxide levels in women with preeclampsia. Eur J Obstet Gynecol Reprod Biol 2004;113:21–25.
Alonso D, Radomski MW. The nitrix oxide-endothelin-1 connection. Heart Fail Rev 2003;8:107–115.
Haynes WG, Webb DJ. Endothelin as a regulator of cardiovascular function in health and disease. J Hypertens 1998;16:1081–1098.
Albercht EW, Stegeman CA, Heeringa P, Henning RH, van Goor H. Protective role of endothelial nitric oxide synthase. J Pathol 2003;199:8–17.
Govers R, Rabelink TJ. Cellular regulation of endothelial nitric oxide synthase. Am J Physiol Renal Physiol 2001;280:F193–F206.
Wang Y, Gu Y, Zhang Y, Lewis DF. Evidence of endothelial dysfunction in preeclampsia: Decreased endothelial nitric oxide synthase expression is associated with increased cell permeability in endothelial cells from preeclampsia. Am J Obstet Gypnecol 2004;190:817–824.
Strevens H, Wide-Swensson D, Hansen A, et al. Glomerular endotheliosis in normal pregnancy and pre-eclampsia. BJOG 2003;110:831–836.
Campbell DM, Campbell AJ. Evans Blue disappearance rate in normal and pre-eclamptic pregnancy. Clin Exp Hypertens B 1983;2:163–169.
Deng L, Bremme K, Hansson LO, Blomback M. Plasma levels of von Willebrand factor and fibronectin as markers of persisting endothelial damage in preeclampsia. Obstet Gynecol 1994;84:3941–3945.
Perry KG Jr, Martin JN Jr. Abnormal hemostasis and coagulopathy in preeclampsia and eclampsia. Clin Obstet Gynecol 1992;35:338–350.
Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy 2001;20:IX–XIV.
von Dadelszen P, Magee LA, Roberts JM. Subclassification of preeclampsia. Hypertens Pregnancy 2003;22:143–148.
Audibert F, Friedman SA, Frangieh AY, Sibai BM. Clinical utility of strict diagnostic criteria for the HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome. Am J Obstet Gynecol 1996;175:460–464.
Janssen S, Limburg PC, Bijzet J, et al. SAA versus CRP in chronic inflammatory disease. In: Peeters H, ed. Protides of the biological fluids. Oxford, UK: Pergamon Press; 1986:347–350.
Radonic A, Thulke S, Mackay IM, Landt O, Siegert W, Nitsche A. Guideline to reference gene selection for quantiative realtime PCR. Biochem Biophys Res Commun 2004;313:856–862.
Mutin M, Dignat-George F, Sampol J. Immunologic phenotype of cultured endothelial cells: Quantitative analysis of cell surface molecules. Tissue Antigens 1997;50:449–458.
Murakami S, Morioka T, Nakagawa Y, Suzuki Y, Arakawa M, Oite T. Expression of adhesion molecules by cultured human glomerular endothelial cells in response to cytokines: Comparison to human umbilical vein and dermal microvascular endothelial cells. Microvasc Res 2001;62:383–391.
Van der Laan N, de Leij L, Ten Duis HJ. Local cellular inflammation as a result of elective standardized vascular surgery. Acta Histochem 2001;103:139–149.
Donker RB, Asgeirsdottir SA, Gerbens F, et al. Plasma factors in severe early-onset preeclampsia do not substantially alter endothelial gene expression in vitro. J Soc Gynecol Investig 2005;12:98–106.
Coata G, Pennacchi L, Bini V, Liotta L, Di Renzo GC. Soluble adhesion molecules: Marker of pre-eclampsia and intrauterine growth restriction. J Matern Fetal Neonat Med 2002;12:28–34.
Higgins JR, Papayianni A, Brady HR, Darling MR, Walshe JJ. Circulating vascular cell adhesion molecule-1 in pre-eclampsia, gestational hypertension, and normal pregnancy: Evidence of selective dysregulation of vascular cell adhesion molecule-1 homeostasis in pre-eclampsia. Am J Obstet Gynecol 1998;179:464–469.
Lyall F, Hayman RG, Ashworth IR, Duffie E, Baker PN. Relationship of cell adhesion molecule expression to endothelium-dependent relaxation in normal pregnancy and pregnancies complicated with preeclampsia or fetal growth restriction. J Soc Gynecol Investig 1999;6:196–201.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Groningen University Institute for Drug Exploration (GUIDE) and the Jan Kornelis de Cock Foundation, Project No. 04-06.
The authors thank Henk E. Moorlag, Department of Pathology and Laboratory Medicine, and Johan Bijzet, Department of Clinical Immunology, for expert technical assistance, and Sarah Buddeke and Patrick Vischjager for assistance in clinic and laboratory.
Rights and permissions
About this article
Cite this article
Donker, R.B., Molema, G., Faas, M.M. et al. Absence of In Vivo Generalized Pro-Inflammatory Endothelial Activation in Severe, Early-Onset Preeclampsia. Reprod. Sci. 12, 518–528 (2005). https://doi.org/10.1016/j.jsgi.2005.06.007
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jsgi.2005.06.007
Key words
- Preeclampsia
- severe early-onset preeclampsia
- endothelial activation
- endothelial cell activation
- pro-inflammatory endothelial activation
- in vivo
- protein expression
- gene expression
- vascular cell adhesion molecule-1 (VCAM-1)
- intercellular adhesion molecule-1 (ICAM-1)
- E-selectin
- endothelial nitric oxide synthase (eNOS)
- endothelin-1