Abstract
Background
Both hemodynamic abnormalities and thrombophilia predispose to pregnancy-associated vascular complications such as fetal growth restriction, stillbirth, preeclampsia, and placental abruption. Antithrombotic treatment may reduce the risk for these events. In this study we tested the hypothesis that in normotensive thrombophilic formerly preeclamptic women certain alterations in hemodynamic function as measured under nonpregnant conditions predict the development of hypertensive disorders and / or fetal growth restriction in the subsequent pregnancy.
Methods
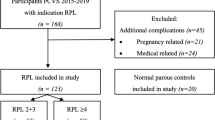
In 350 nondiabetic formerly preeclamptic women, we measured in the follicular phase of the menstrual cycle at least 5 months postpartum central hemodynamic, metabolic, and hemostatic variables. In the subsequent ongoing pregnancy we determined fetal outcome variables and the incidence of maternal vascular complications. In addition to a normotensive thrombophilic profile, inclusion for final analysis required a subsequent singleton pregnancy, established within 1 year following the pre-pregnant evaluation and ongoing beyond 16 weeks’ gestation. As a consequence, 47 normotensive thrombophilic formerly preeclamptic women could be included for final analysis. All formerly preeclamptic participants received aspirin throughout pregnancy. Additionally, those with thrombophilia or hyperhomocysteinemia were treated with low molecular weight heparin and with pyridoxine and folic acid supplementation, respectively.
Results
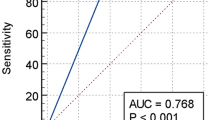
Among 350 formerly preeclamptic women, 266 (76%) were normotensive and 84 (24%) hypertensive. About half (140/2 66) of normotensive formerly preeclamptic participants were thrombophilic. One hundred eighteen formerly preeclamptic participants succeeded in establishing an ongoing pregnancy within 1 year. From this subset of formerly preeclamptic women, 47 were normotensive thrombophilic; 23 remained normotensive (THROMB), whereas 24 developed at least gestational hypertension (COMPLITHROMB). Participants in the latter subgroup were more obese than those remaining normotensive. In addition, this former subset of women had a higher vascular resistance index, and a lower plasma volume and cardiac index. With respect to fetal outcome, COMPLITHROMB gave birth to an infant with a lower birth weight relative to THROMB. Preeclampsia with or without the hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome recurred in 26% of the participants in the whole thrombophilic group, in which a low pre-pregnant plasma volume and a raised vascular resistance predisposed for recurrent hypertensive disorders.
Conclusion
Pre-pregnant hemodynamic, metabolic, and clotting variables in formerly preeclamptic women can predict hypertension in the subsequent pregnancy.
Similar content being viewed by others
References
Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol 2000;183:S1–22.
Schuitemaker NEW, van Roosmalen J, Dekker GA, van Dongen PWJ, van Geijn HP, Bennebroek Gravenhorst J. Confidential inquiry into maternal deaths in The Netherlands 1983–1992. Eur J Obstet Gynecol Reprod Biol 1998;79:57–62.
Dekker GA, de Vries JIP, Doelitzsch PM, et al. Underlying disorders associated with severe early-onset preeclampsia. Am J Obstet Gynecol 1995;173:1042–8.
van Pampus MG, Dekker GA, Wolf H, et al. High prevalence of hemostatic abnormalities in women with a history of severe preeclampsia. Am J Obstet Gynecol 1999;180:1146–50.
Kupferminc MJ, Eldor A, Steinman N, et al. Increased frequency of genetic thrombophilia in women with complications of pregnancy. N Engl J Med 1999;340:9–13.
Spaanderman MEA, Ekhart THA, van Eyck J, Cheriex EC, de Leeuw PW, Peeters LLH. Asymptomatic ex-preeclamptic women have latent hemodynamic abnormalities. Am J Obstet Gynecol 2000;182:101–7.
van Beek E, Ekhart THA, Schiffers PMH, van Eyck J, Peeters LLH, de Leeuw PW. Persistent abnormalities in volume homeostasis and renal hemodynamics in patients with a history of preeclampsia. Am J Obstet Gynecol 1998;179:690–6.
Aardenburg R, Spaanderman MEA, Ekhart THA, van Eijndhoven HW, van der Heijden OWH, Peeters LLH. Low plasma volume following pregnancy complicated by pre-eclampsia predisposes for hypertensive disease in a-next pregnancy. BJOG 2003;110:1001–6.
Roberts JM. Endothelial dysfunction in preeclampsia. Semin Reprod Endocrinol 1998;16:5–15.
Walker FM, Ferguson SE, Allen VM. Heparin for pregnant women with acquired or inherited thrombophilias (Cochrane Review). The Cochrane Library, Vol 2. Chichester, UK: Wiley, 2004.
Brenner B, Kupferminc MJ. Inherited thrombophilia and poor pregnancy outcome. Best Pract Res Clin Obstet Gynaecol 2003;17:427–39.
Eskenazi B, Fenster L, Sidney S. A multivariate analysis of risk factors for preeclampsia. JAMA 1991;266:237–41.
Sibai BM, el-Nazer A, Gonzalez-Ruiz A. Severe preeclampsia-eclampsia in young primigravid women: Subsequent pregnancy outcome and remote prognosis. Am J Obstet Gynecol 1986;155:1011–6.
Sibai BM, Mercer B, Sarinoglu C. Severe preeclampsia in the second trimester: Recurrence risk and long-term prognosis. Am J Obstet Gynecol 1991;165:1408–12.
Zhang J, Troendle J, Levine R. Risks of hypertensive disorders in the second pregnancy. Paediatr Perinat Epidemiol 2001;15:226–231.
Sullivan CA, Magnann EF, Perry K, Jr, Roberts WE, Blake PG, Martin J, Jr. The recurrence risk of the syndrome of hemolysis, elevated liver enzymes, and low platelets (HELLP) in subsequent gestations. Am J Obstet Gynecol 1994;171:940–3.
Sibai BM, Ramadan MK, Chari RS, Friedman SA. Pregnancies complicated by HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets): Subsequent pregnancy outcome and long-term prognosis. Am J Obstet Gynecol 1995;172:125–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spaanderman, M.E.A., Aardenburg, R., Ekhart, T.H.A. et al. Pre-pregnant Prediction of Recurrent Preeclampsia in Normotensive Thrombophilic Formerly Preeclamptic Women Receiving Prophylactic Antithrombotic Medication. Reprod. Sci. 12, 112–117 (2005). https://doi.org/10.1016/j.jsgi.2004.10.009
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jsgi.2004.10.009