Abstract
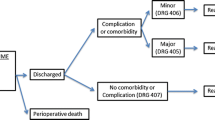
Recent studies have demonstrated the relationship between clinical outcomes of complex surgical procedures and provider volume. Hepatic resection is one such high-risk surgical procedure. The aim of this analysis was to determine whether mortality and cost of performing hepatic resection are related to surgical volume while also examining outcomes by extent of resection and diagnosis, variables seen with this procedure. Maryland discharge data were used to study surgical volume, length of stay, charges, and mortality for 606 liver resections performed at all acute-care hospitals between January 1990 and June 1996. One high-volume provider accounted for 43.6% of discharges, averaging 40.6 cases per year. In comparison, the remainder of resections were performed at 35 other hospitals, averaging 1.5 cases per year. Data were stratified into these high- and low-volume groups, and adjusted outcomes were compared. The mortality rate for all procedures in the low-volume group was 7.9% compared to 1.5% for the high-volume provider (P <0.01, relative risk = 5.2). No overall differences were observed between low- and high-volume providers in total hospital charges. When analyzing by procedure type and diagnosis, lower mortality was seen in the high-volume center for both minor and major resections, as well as resections for metastatic disease. It was concluded that hepatic resection can be performed more safely and at comparable cost at high-volume referral centers.
Similar content being viewed by others
References
Luft HS, BunkerJP, Enthoven AC. Should operations be re- gionalized: The empirical relation between surgical volume and mortality. N EnglJ Med 1979;301:1364–1369.
Luft H. The relation between surgical volume and mortality: An exploration of causal factors and altenative models. Med Care 1980;18:940–959.
Flood AB, Scott WR, Ewy W. Does practice make perfect? Part I: The relation between hospital volume and outcomes for selected diagnostic categories. Med Care 1984;22:98–114.
Flood AB, Scott WR, Ewy W. Does practice make perfect? Part II: The relation between volume and outcomes and other hospital characteristics. Med Care 1984;22:115–125.
Hannan EL, Racz M, Ryan TJ, et al. Coronary angioplasty volume-outcome relationships for hospitals and cardiologists. JAMA 1997;277:892–898.
Grumbach K, Anderson GM, Luft HS, Roos LL, Brook R. Regionalization of cardiac surgery in the United States and Canada. JAMA 1995;274:1282–1288.
Lieberman MD, Kilburn H, LLndsey M, Brerman ME. Relation of preoperative deaths to hospital volume among patients undergoing pancreatic resection for malignancy. Ann Surg 1995;222:638–645.
Glascow RE, Mulvhill SJ. Relation ofhosp/tal volume to out-come in patients undergoing Whipple resection for adenocar-cinoma ia Northern California hospitals in 1993. Presented at the Thirtieth Annual Meeting of Pancreas Club, Inc., San Francisco, Calif.,May 19, 1996.
Gordon TA, Burleyson GP, Tielsch JM, Cameron JL. The effects of regionaIization on cost and outcome for one general high-risk surgical procedure. Ann Surg 1995;221:43–49.
Gordon TA, Burleyson GP, Shahrokh S, Cameron JL. Cost and outcome for complex high-risk gastro-intestinat surgical procedures. Surg Forum 1996;47:618–620.
Hannah EL, O’Doimell JF, Kilbum H Jr, et al. Investigation of the relationship between volume and mortality for surgical procedures performed inNew York state hospitals. JAMA 1989;262:503 -510.
Hannan EL, Kilburn H Jr, O’Donnell JF, et al. A longitudinal analysis of the relationship between in-hospital mortality in New York state hopsitals and the volume of abdominal aortic aneurysm surgeries performed. Health Serv Res 1992;27:518–542.
Showstack JA, Rosenfeld KE, Gamick DW, et al. Association of volume with outcome of coronary artery bypass graft surgery: Scheduled vs. nonscheduled operations. JAMA 1987;257:785–789.
Choi TK, Lai Edward CS, Fan ST, et al. Results of surgical resection for hepatocellular carcinoma. Hepatogastroenterology 1990;37:172–175.
Haratake J, Takeda S, Kasai T, et al. Predictable factors for estimating prognosis of patients after resection of hepatocellular carcinoma. Cancer 1993;72:1178–1183.
Takenaka K, Kawahara N, Yamamoto K, et al. Results of 280 liver resections for hepatocellular carcinoma. Arch Surg 1996;131:71–76.
Fong Y, Blumgart LH, Cohen AM. Surgical treatment of colorectal metastases to the liver. CA Cancer J Clin 1995;45:50–62.
Medicode’s International Classification of Diseases, 9th revision, Clinical Modification, 4th ed, 1995.
Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40:373–383.
Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: Differing perspectives. J Clin Epidemiol 1993;46:1075–1079.
Sitzmann JV, Greene PS. Perioperative predictors of morbidity following hepatic resection for neoplasm. A multivariate analysis of a single surgeon experience with 105 patients. Ann Surg 1994;219:13–17.
Stimpson REJ, Pellegrini CA, Way LW. Factors affecting the morbidity of elective liver resection. AmJ Surg 1987;153:189–196.
Vauthey JN, Baer UB, Guastella T, Blumgart LH. Comparison of outcome between extended and nonextended liver resections for neoplasms. Surgery 1993; 114:968–973.
Schlag P, Hohenberger P, Herforth C. Resection of liver metastases in colorectal cancer: Competitive analysis of treatment results in synchronous versus metachronous metastases. EurJ Surg Oncol 1990;16:360–365.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choti, M.A., Bowman, H.M., Pitt, H.A. et al. Should hepatic resections be performed at high-volume referral centers?. J Gastrointest Surg 2, 11–20 (1998). https://doi.org/10.1016/S1091-255X(98)80098-X
Issue Date:
DOI: https://doi.org/10.1016/S1091-255X(98)80098-X