Abstract
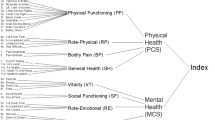
Secondary peptic ulcer surgery is uncommon given the success of a wide variety of medical therapies, plus the good outcome expected after primary peptic ulcer surgery. Early reports of secondary peptic ulcer surgery in the 1950s and 1960s suggested good long-term outcome in most patients; however, recent data suggest that patients operated in the Helicobacter pylori era have a worse outcome. We have attempted to quantify the poor outcome in these patients and measure the effect of sex, a previously unrecognized risk factor for poor outcome after peptic ulcer surgery. We reviewed the outcomes of 35 patients who underwent secondary peptic ulcer surgery for symptoms of persistent or recurrent peptic ulcer symptoms or complications of the condition. These patients were compared to a "control" group of patients to determine long-term quality of life as measured by the SF-36 and Visick scores (average follow-up 60 months). Visick and SF-36 scores were obtained through telephone interviews. The two groups of patients were age matched to eliminate age as a variable in the SF-36 results. There were more females than males in the secondary peptic ulcer surgery group (4.5/1 female-to-male ratio). Although perioperative mortality was zero for both groups, patients undergoing secondary peptic ulcer surgery had a high number of complications (57% of patients had complications). Patients undergoing secondary peptic ulcer surgery scored lower in seven of the eight subclasses of the SF-36 questionnaire compared to their age-matched cohorts. In contrast, average Visick scores showed slight improvement for three out of four symptoms reported. Immediate postoperative complications were not related to long-term quality of life issues. Secondary peptic ulcer surgery is more prevalent in females than in males. Although secondary peptic ulcer surgery is partially effective in alleviating symptoms, quality of life is poor.
Similar content being viewed by others
References
Heppell J, Bess MA, McIlrath DC, Dozois RR. Surgical treatment of recurrent peptic ulcer disease. Ann Surg 1983; 198:1–4.
Ware JE. SF-36 Health Survey: Manual and Interpretation Guide. Boston: The Medical Outcomes Trust, 1993.
Browder W, Thompson J, Youngberg G, Walters D. Delayed ulcer recurrence after gastric resection: A new post-gastrectomy syndrome? Am Surg 1997;63:1091–1096.
Hirchowitz BI, Lanas A. Intractable upper gastrointestinal ulceration due to aspirin in patients who have undergone surgery for peptic ulcer disease. Gastroenterology 1998;114: 883–892.
Muscroft TJ, Taylor EW, Deane SA, Alexander-Williams J. Reoperation for recurrent peptic ulceration. BrJ Surg 1981; 68:75–76.
Pietri P, Gabrielli F, Pellis G. Reoperation for recurrent peptic ulcer. Int Surg 1983;68:301–305.
Hoffman J, Shokouh-Amiri MH, Klarskov P, et al. Gastrectomy for recurrent ulcer after vagotomy: Five-to nineteen-year follow-up. Surgery 1986;99:517–522.
Jaffe BM, Newton WT, Judd DR, Ballinger WF. Surgical management of recurrent peptic ulcers. Am J Surg 1969; 117:214–221.
Gustavsson S, Kelly KA. Total gastrectomy for benign disease. Surg Clin North Am 1987;67:539–551.
Eckhauser FE, Knol JA, Raper SA, Guice KS. Completion gastrectomy for postsurgical gastroparesis syndrome. Ann Surg 1988;208:345–353.
Forstner-Barthell AW, Murr MM, Nitecki S, et al. Neartotal completion gastrectomy for severe postvagotomy gastric stasis: Analysis of early and long-term results in 62 patients. J Gastrointest Surg 1999;3:15–21.
Sawyer JL. In discussion: Completion gastrectomy for post-surgical gastroparesis syndrome. Ann Surg 1988;208:352–353.
Farahmand M, Sheppard BC, Deveney CW, et al. Longterm outcome of completion gastrectomy for nonmalignant disease. J gastrointest Surg1997;1:182–187.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gonzàlez-Stawinski, G.V., Rovak, J.M., Seigler, H.F. et al. Poor outcome and quality of life in female patients undergoing secondary surgery for recurrent peptic ulcer disease. J Gastrointest Surg 6, 396–402 (2002). https://doi.org/10.1016/S1091-255X(01)00029-4
Issue Date:
DOI: https://doi.org/10.1016/S1091-255X(01)00029-4