Abstract
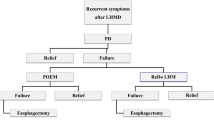
Two case reports demonstrate the paradoxical occurrence of achalasia many years after the successful surgical treatment of gastroesophageal reflux disease (GERD). These patients had remedial surgery laparoscopically. The three types of achalasia syndromes that can follow antireflux surgery are discussed. In type 1, primary achalasia is misdiagnosed as GERD and inappropriate antireflux surgeD, causes worsenhag dysphagia immediately after surgery without any symptom-free interval. In type 2, secondary iatrogenic achalasia is seen early after antireflux surgery and is characterized by the presence of stenosis and scar formation at the site of the fundic wrap. Although the motility studies resemble achalasia, the repair needs only to be taken down and refashioned when there is no response to balloon dilatation. In type 3, illustrated by the case reports, primary achalasia follows antireflux surgery after a significant symptom-free interval. There is complete absence of any stenosis or fibrosis of the esophagus and periesophageal tissues at remedial surgery. Moreover, surgical treatment of this condition needs to include esophageal myotomy.
Similar content being viewed by others
References
McCallum RW. Esophageal achalasia secondary to gastric car- cinoma. Pun J Gastroenterol 1979;71:24–29.
Kline MM. Successful treatment of vigorous achalasia associ- ated with gastric lymphoma. Dig Dis Sci 1980;25:311–313.
Goldin NR, Burns TW, Ferrante WVA. Secondary achalasia: Association with adenocarcinoma of the lung and reversal with radiation therapy. Am J Gastroenterol 1983;78:203–205.
Davis JA, Kantrowitz PA, Chandler HL, Schatzki SC. Re- versible achalasia due to reticulum-cell sarcoma. N Engl J NIed 1976;293:130–132.
Roark G, Shabot M, Patterson M. Achalasia secondary to he- patocellular carcinoma. J Clin Gastroentero1 1983;5:255–258.
Eaves R, Lambert J, Rees J, King RWF. Achalasia secondary to carcinoma of prostate. Dig Dis Sci 1983;28:278–284.
Feldman M. Esophageal achalasia syndromes. Am J Med Sci 1988;295:60–81.
Reynolds JC, Parkman HP. Achalasia. Gastroenterol Clin North Am 1989;18:223–255.
Woods CA, Foutch PG, Waring JP, Sanowski RA. Pancreatic pseudocyst as a cause for secondary achalasia. Gastroenterol- ogy 1989;96:235–239.
Aguayo JL, Martinez de Haro L, Ortiz A, Martinez DA, Morales G. Reversible achalasia-like motor pattern of esoph- ageal body secondary to postoperative stricture of gastro- esophageal junction. Dig Dis Sci 1992;37:1781–1784.
Ellingson TL, Kozarek RA, Gelfand MD, Botoman AV, Pat-terson DJ. latrogenic achalasia. J Clin Gastroenterol 1995; 20:96–99.
Toffolon EP, Devers TJ. Achalasia following esophageal sur- gery. Corm Med 1982;46:249–250.
Ellis FH, Kiser FC, Schlegel JF, Earlam RJ, McveyJL, Olsen AM. Esophagomyotomy for esophageal acbalasia: Experi- mental, clinical and manometric aspects. Ann Surg 1967; 166:640–656.
Stuart RC, Hennessy TPJ. Primary disorders of esophageal motility. Review. BrJ Surg 1989;76:1111–1120.
Smart HL, MayberryJF, Atldnson M. Achalasia following gastro-esopbageal reflux. J RSocMed 1986;79:71–73.
Shoenut JP, Mickflikier AB, Yaffe CS, Den Boer B, Teskey JM. Reflux in untreated achalasia patients. J Clin Gastroenterol 1995;20:6–11.
Spechler SJ, Souza RF, Rosenberg SJ, Ruben RA, Goyal RK. Heartburn in patients with achalasia. Gut 1995;37:305–308.
Mattox HE III, Albertson DA, Castell DO, Richter JE. Dys- phagia following fundoplication: “Slipped” fundoplication versus achalasis complicated by fundoplication. Pun J Gas- troenterol 1990;85:1468–1472.
O’Brien CJ, Collins JSA, Collins BJ, McGuigan J. Aperistaltic oesophageal disorders unmasked by severe post-fundoplica- tion dysphagia. Postgrad Med J 1990;66:1047–1049.
Wo JM, Trus TL, Richardson WS, Hunter JG, Branum GD, Mauren SJ, Waring JP. Evaluation and management of postfun- doplication dysphagia. Am J Gastroenterol 1996;90:2318–2322.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Poulin, E.C., Diamant, N.E., Kortan, P. et al. Achalasia developing years after surgery for reflux disease: Case reports, laparoscopic treatment, and review of achalasia syndromes following antireflux surgery. J Gastrointest Surg 4, 626–631 (2000). https://doi.org/10.1016/S1091-255X(00)80113-4
Issue Date:
DOI: https://doi.org/10.1016/S1091-255X(00)80113-4