Abstract
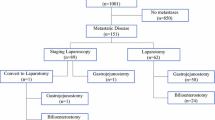
Laparoscopy and laparoscopic ultrasound are used widely in cancer staging and are perceived to prevent unnecessary open exploration in many patients. The aim of this study was to analyze the impact of staging laparoscopy in improving resectability in patients with primary and secondary hepatobiliary malignancies. Over a 10-month period (November 1, 1997 to August 31, 1998), 186 patients with primary and secondary hepatobiliary cancers were submitted to operation for potentially curative resection. One hundred four patients staged laparoscopically (LAP) before laparotomy were compared prospectively to 82 patients undergoing exploration without laparoscopy (NO LAP). Assignment to each group was not random but was based on surgeon practice. Demographic data, diagnoses, the extent of preoperative evaluation, and the percentage of patients resected were similar in the two groups. Laparoscopy identified 26 (67%) of 39 patients with unresectable disease. In the NO LAP group, 28 patients (34%) had unresectable disease discovered at laparotomy. In patients with unresectable disease and submitted to biopsy only, the operating times were similar in the two groups (LAP 83 ±22 minutes vs. NO LAP 91 ±33 minutes; P = 0.4). However, laparoscopic staging significantly reduced the length of hospital stay (LAP 2.2 ±2 days vs. NO LAP 8.5 ±8.6 days; P = 0.006). Likewise, total hospital charges, normalized to 100 in the NO LAP patients, were significantly lower in the LAP group (LAP 54 ±42 vs. NO LAP 100 ±84; P = 0.02). Staging laparoscopy identified the majority of patients with unresectable hepatobiliary malignancies, significantly improved resectability, and reduced the number of days in the hospital and the total charges. The yield of laparoscopy was greatest for detecting peritoneal metastases (9 of 10), additional hepatic tumors (10 of 12), and unsuspected advanced cirrhosis (5 of 5) but often failed to identify nonresectability because of lymph node metastases, vascular involvement, or extensive biliary involvement. Eighty-three percent of patients subjected to laparotomy after laparoscopy underwent a potentially curative resection compared to 66% of those who were not staged laparoscopically.
Similar content being viewed by others
References
Bartlett DL, Fong Y, Fortuer JG, et al.. Long-term results af- ter resection for gallbladder cancer. Implications for staging and management [Review]. Ann Surg 1996;224:639–646.
Burke EC, Jamagin WR, Hochwald SN, et al.. Hilar cholan- giocarcinoma: Patterns of spread, the importance of hepatic resection for curative operation, and a presurgical clinical stag- ing system. Ann Surg 1998;228:385–394.
D’Angelica M, Brennan MF, Fortuer J, et al.. Ninety-six five- year survivors after liver resection for metastatic colorectal cancer. J Am Coll Surg 1997;185:554–559.
Fong Y, Sun RL, Jarnagin WR, Blumgart LH. Hepatocellular carcinoma: An analysis of 412 cases at a Western center. Ann Surg 1999;229:790–799.
Harrison LE, Brennan MF, Newman E, et al.. Hepatic resec- tion for noncolorectal, nonneuroendocrine metastases: A fif- teen-year experience with ninety-six patients. Surgery 1997; 121:625–632.
Harrison LE, Fong Y, Klimstra DS, et al.. Surgical treatment of 32 patients with peripheral intrahepatic cholangiocarci- noma. BrJ Surg 1998;85:1068–1070.
Fortuer J, Silva JS, Golbey RB, et al.. Multivariate analysis of a personal series of 247 consecutive patients with liver metas- tases from Colorectal cancer: I. Treatment by hepatic resec- tion. Ann Surg 1984;199:306–316.
Steele G, Bleday R, Mayer RJ, et al.. A prospective evaluation of hepatic resection for colorectal carcinoma metastases to the liver: Gastrointestinal tumor study group protocol 6584. J Clin Oncol 1991;9:1105–1112.
Gibbs JF, Weber TK, Rodriguez-Bigas MA, et al.. Intraopera- five determinants of unresectability for patients with colorec- tal hepatic metastases. Cancer 1998;82:1244–1249.
Jarnagin WR, Fong Y, Ky A, et al.. Liver resection for metasta- tic colorectal cancer: Assessing the risk of occult irresectable disease. J Am Coil Surg 1999;188:33–42.
Lo CM, Lai EC, Liu CL, et al.. Laparoscopy and laparoscopic ultrasonography avoid exploratory laparotomy in patients with hepatocellular carcinoma. Ann Surg 1998;227:527–532.
Babineau T, Lewis D, Jenkins R, et al.. Role of staging lapa- roscopy in the treatment of hepatic malignancy. Am J Surg 1994;167:151–155.
Callery MP, Strasberg SM, Doherty GM, et al.. Staging lapa- roscopy with laparoscopic ultrasonography: Optimizing re- sectability in hepatobiliary and pancreatic malignancy. J Am Coil Surg 1997;185:33–39.
John TG, Greig JD, Crosbie JL, et al.. Superior staging of liver tumors with laparoscopy and laparoscopic ultrasound. Ann Surg 1994;220:711–719.
Conlon KC, Ting A, Dougherty E, Brennan ME. The eco- nomic effect of the introduction of laparoscopic staging for patients with adenocarcinoma of the pancreas: A prospective analysis of hospital charges. Ann Surg Oncol (in press).
Savader SJ, Lillemoe KD, Prescott CA, et al.. Laparoscopic cholecystectomy-related bile duct injuries: A health and fi- nancial disaster. Ann Surg 1997;225:268–273.
Traverso LW. The laparoscopic surgical value package and how surgeons can influence costs. Surg Clin North Am 1996; 76:631–639.
Blumgart LH, Benjamin IS. Cancer of the bile ducts. In Blumgart LH, ed. Surgery of the Liver and Biliary Tract. Ed- inburgh: Churchill Livingstone, 1994, pp 967–995.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported in part by grants R01 CA76416 (Dr. Fong) and R01CA/DK80982 (Dr. Fong) from the National Institutes of Health.
Rights and permissions
About this article
Cite this article
Jarnagin, W.R., Bodniewicz, J., Dougherty, E. et al. A prospective analysis of staging laparoscopy in patients with primary and secondary hepatobiliary malignancies. J Gastrointest Surg 4, 34–43 (2000). https://doi.org/10.1016/S1091-255X(00)80030-X
Issue Date:
DOI: https://doi.org/10.1016/S1091-255X(00)80030-X