Abstract
Excess opioid prescribing among post-surgical patients plays a major contributory role in the ongoing opioid epidemic in the United States—an epidemic that has devastating economic and human life tolls. Artificial intelligence (AI) and machine learning (ML) can be useful clinically by helping providers personalize opioid prescriptions based on individual patient needs and risk factors, thereby closing the gap between prescribed and consumed amounts. In this article, we explore the rationale for implementing AI/ML tools for post-surgical opioid prescription and recent use cases that have accurately predicted post-discharge opioid consumption and allowed providers to identify patients with unique prescription needs. These use cases not only address the challenge of capturing accurate and clinically relevant post-discharge patient data but also demonstrate promising preliminary evidence in reducing the opioid prescription volume at an institutional level. We later propose recommendations for AI/ML to be broadly applied across the entirety of the opioid prescription life cycle, from improving the precision of prescription quantity, monitoring individual- and population-level patient outcomes, to enhancing care integration. Lastly, we discuss potential challenges for future applications and scaling opportunities, including existing infrastructural limitations, evolving regulatory requirements, and the necessity of relevant stakeholder involvement throughout the intervention development process. In addition to ensuring the accuracy of model predictions, AI/ML-generated, data-driven insights also need to be reinforced by behavioral change strategies to encourage providers to adhere to recommendations. In short, AI/ML technologies can promote responsible and personalized opioid prescribing practices among healthcare providers, while achieving adequate post-surgical pain control and curbing opioid overprescription.
Similar content being viewed by others
References
2022 NSDUH annual national report 2023. https://www.samhsa.gov/data/report/2022-nsduh-annual-national-report (accessed February 16, 2024).
Agniel D, Brat GA, Marwaha JS, Fox K, Knecht D, Paz HL, et al. Association of postsurgical opioid refills for patients with risk of opioid misuse and chronic opioid use among family members. JAMA Netw Open. 2022;5: e2221316.
Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg. 2017;152:1066–71.
Young JC, Dasgupta N, Chidgey BA, Jonsson FM. Postsurgical opioid prescriptions and risk of long-term use: an observational cohort study across the United States. Ann Surg. 2021;273:743–50.
Howard R, Fry B, Gunaseelan V, Lee J, Waljee J, Brummett C, et al. Association of opioid prescribing with opioid consumption after surgery in Michigan. JAMA Surg. 2019;154: e184234.
Jones T, Moore TM, Meske DS, Passik SD. Preliminary validation of the Diversion Risk Scale (DRS): using environmental and individual factors to predict opioid-related diversion events. J Opioid Manag. 2023;19:35–42.
Guy GP Jr, Zhang K. Opioid prescribing by specialty and volume in the U.S. Am J Prev Med. 2018;55:e153–5.
Callinan CE, Neuman MD, Lacy KE, Gabison C, Ashburn MA. The initiation of chronic opioids: a survey of chronic pain patients. J Pain. 2017;18:360–5.
Marwaha JS, Kennedy CJ, Brat GA. Surgical residency programs should leverage recent advances in national policy, real-world data, and public opinion to improve post-surgery opioid prescribing. J Grad Med Educ. 2022;14:25–9.
ACGME releases recommendations and resources on Preparing Residents and Fellows to Manage Pain and substance use disorder 2021. https://www.acgme.org/newsroom/2021/10/opioid-congress-recommendations/ (accessed February 16, 2024).
Price SM, O’Donoghue AC, Rizzo L, Sapru S, Aikin KJ. Opioid education and prescribing practices. J Am Board Fam Med. 2021;34:802–7.
Kim BJ, Newhook TE, Blumenthaler A, Chiang Y-J, Aloia TA, Roland CL, et al. Sustained reduction in discharge opioid volumes through provider education: results of 1168 cancer surgery patients over 2 years. J Surg Oncol. 2021;124:143–51.
Larach DB, Sahara MJ, As-Sanie S, Moser SE, Urquhart AG, Lin J, et al. Patient factors associated with opioid consumption in the month following major surgery. Ann Surg. 2021;273:507–15.
Overton HN, Hanna MN, Bruhn WE, Hutfless S, Bicket MC, Makary MA, et al. Opioid-prescribing guidelines for common surgical procedures: an expert panel consensus. J Am Coll Surg. 2018;227:411–8.
Kaafarani HMA, Eid AI, Antonelli DM, Chang DC, Elsharkawy AE, Elahad JA, et al. Description and impact of a comprehensive multispecialty multidisciplinary intervention to decrease opioid prescribing in surgery. Ann Surg. 2019;270:452–62.
Robinson KA, Thiels CA, Stokes S, Duncan S, Feranil M, Fleishman A, et al. Comparing clinician consensus recommendations to patient-reported opioid use across multiple hospital systems. Ann Surg. 2022;275:e361–5.
Dowell D. CDC clinical practice guideline for prescribing opioids for pain—United States, 2022. MMWR Recomm Rep 2022;71. https://doi.org/10.15585/mmwr.rr7103a1.
Imo CS, Macias DA, McIntire DD, McGuire J, Nelson DB, Duryea EL. A personalized protocol for prescribing opioids after cesarean delivery: leveraging the electronic medical record to reduce outpatient opioid prescriptions. Am J Obstet Gynecol. 2023. https://doi.org/10.1016/j.ajog.2023.09.092.
Zhang KK, Blum KM, Chu JJ, Zewdu A, Janse S, Skoracki R, et al. A personalized opioid prescription model for predicting postoperative discharge opioid needs. Plast Reconstr Surg. 2023;151:450–60.
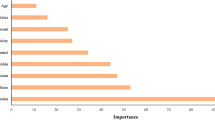
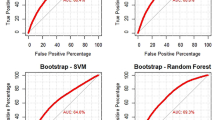
Yu JK, Marwaha JS, Kennedy CJ, Robinson KA, Fleishman A, Beaulieu-Jones BR, et al. Who doesn’t fit? A multi-institutional study using machine learning to uncover the limits of opioid prescribing guidelines. Surgery. 2022;172:655–62.
Beaulieu-Jones BR, Marwaha JS, Kennedy CJ, Le D, Berrigan MT, Nathanson LA, et al. Comparing rationale for opioid prescribing decisions after surgery with subsequent patient consumption: a survey of the highest quartile of prescribers. J Am Coll Surg. 2023;237:835–43.
Marwaha JS, Beaulieu-Jones BR, Kennedy CJ, Nathanson LA, Robinson K, Tandon M, et al. Design, implementation, and clinical impact of a machine learning-assisted intervention bundle to improve opioid prescribing. NEJM Catal Innov Care Deliv. 2022;3. https://doi.org/10.1056/cat.21.0477.
Sud A, Molska GR, Salamanca-Buentello F. Evaluations of continuing health provider education focused on opioid prescribing: a scoping review. Acad Med. 2022;97:286–99.
Marwaha JS, Beaulieu-Jones BR, Kennedy CJ, Bicket MC, Brat GA. Research priorities for the surgical care of patients taking opioids preoperatively. Reg Anesth Pain Med. 2022. https://doi.org/10.1136/rapm-2022-103584.
Marwaha JS, Raza MM, Kvedar JC. The digital transformation of surgery. NPJ Digit Med. 2023;6:103.
Kassam A-F, Kim Y, Cortez AR, Dhar VK, Wima K, Shah SA. The impact of opioid use on human and health care costs in surgical patients. Surg Open Sci. 2020;2:92–5.
Santosa KB, Lai Y-L, Oliver JD, Hu H-M, Brummett CM, Englesbe MJ, et al. Preoperative opioid use and mortality after minor outpatient surgery. JAMA Surg. 2020;155:1169–71.
Blevins Peratikos M, Weeks HL, Pisansky AJB, Yong RJ, Stringer EA. Effect of preoperative opioid use on adverse outcomes, medical spending, and persistent opioid use following elective total joint arthroplasty in the United States: a large retrospective cohort study of administrative claims data. Pain Med. 2020;21:521–31.
Cron DC, Hwang C, Hu HM, Lee JS, Dupree JM, Syrjamaki JD, et al. A statewide comparison of opioid prescribing in teaching versus nonteaching hospitals. Surgery. 2019;165:825–31.
Sceats LA, Ayakta N, Merrell SB, Kin C. Drivers, beliefs, and barriers surrounding surgical opioid prescribing: a qualitative study of surgeons’ opioid prescribing habits. J Surg Res. 2020;247:86–94.
Kennedy CJ, Marwaha JS, Beaulieu-Jones BR, Scalise PN, Robinson KA, Booth B, et al. Machine learning nonresponse adjustment of patient-reported opioid consumption data to enable consumption-informed postoperative opioid prescribing guidelines. Surg Pract Sci. 2022;10. https://doi.org/10.1016/j.sipas.2022.100098.
Author information
Authors and Affiliations
Contributions
Initial draft was written by JEH, and was edited and reviewed by BBJ, GAB, and JSM. All authors approved the final draft.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no competing interests to declare.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J.E., Beaulieu-Jones, B., Brat, G.A. et al. The role of artificial intelligence in helping providers manage pain and opioid use after surgery. Global Surg Educ 3, 57 (2024). https://doi.org/10.1007/s44186-024-00254-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44186-024-00254-5