Abstract
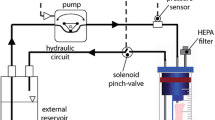
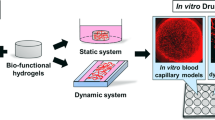
The mechanical stimulation applied on engineered vascular constructs in perfusion bioreactors has been shown to be beneficial for their maturation. The level of mechanical stimulation applied on these constructs depends on the flow parameters of the circuit (e.g., fluid viscosity, flow rate, frequency, and pressure). As a group, these parameters are often overlooked in the literature, and they rarely meet the physiological values of the blood flow. For this reason, the level of circumferential stretching and shear stress that blood vessels experience in the human body are rarely reproduced. In this work, we reported the development of a physiologically relevant platform for (1) the in situ fabrication of vascular wall models based on collagen gel, and (2) their maturation under physiological levels of mechanical stimulation in a perfusion bioreactor (pulsatile flow rate of 100 mL/min, frequency of 1 Hz, pressure of 80–120 mmHg, and viscosity of 4 cP). One week of dynamic maturation oriented the seeded cells into the circumferential direction, increased the deposition of collagen and key elastin fiber-related proteins, and improved the mechanical properties in terms of tensile equilibrium elastic modulus (by 110%) and strength at break (by 63%) when compared to the static condition. In addition to the maturation study under selected physiologically relevant mechanical stimulation (such as adult, fetal, child, and hypertension conditions), the platform might also be used as a relevant in vitro testing system for new drugs or pro-active coating to medical devices (such as stents, endografts, and vascular prostheses) expected to trigger specific mechanisms or activities in vascular cells composing the arterial wall.








Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Loy C, Meghezi S, Levesque L, et al. A planar model of the vessel wall from cellularized-collagen scaffolds: focus on cell-matrix interactions in mono-, bi- and tri-culture models. Biomaterials Science. 2017;5:153–62.
Ishibashi K, Matsuda T. Reconstruction of a hybrid vascular graft hierarchically layered with three cell types. ASAIO journal (American Society for Artificial Internal Organs: 1992). 1994;40:M284-290.
Boland ED, Matthews JA, Pawlowski KJ, et al. Electrospinning collagen and elastin: preliminary vascular tissue engineering. Front Biosci. 2004;9:e32.
González-Pérez M, Camasão DB, Mantovani D, et al. Biocasting of an elastin-like recombinamer and collagen bi-layered model of the tunica adventitia and external elastic lamina of the vascular wall. Biomaterials Science. 2021;9:3860–74.
Tuttolomondo MV, Foglia ML and Manuel J. Approaches for improving the mechanical properties of collagen biomaterials. Advances in Physicochemical Properties of Biopolymers (Part 2) 2017: 354.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS medicine. 2006;3:e442.
Hoskins PR, Lawford PV, Doyle BJ. Cardiovascular biomechanics. Switzerland: Springer; 2017.
Fung Y-c. Biomechanics: mechanical properties of living tissues. 2nd ed. New York: Springer Science & Business Media; 2013.
Boselli F, Freund JB, Vermot J. Blood flow mechanics in cardiovascular development. Cell Mol Life Sci. 2015;72:2545–59.
Cheng JK, Wagenseil JE. Extracellular matrix and the mechanics of large artery development. Biomech Model Mechanobiol. 2012;11:1169–86.
Seliktar D, Black RA, Vito RP, et al. Dynamic mechanical conditioning of collagen-gel blood vessel constructs induces remodeling in vitro. Ann Biomed Eng. 2000;28:351–62.
Bono N, Pezzoli D, Levesque L, et al. Unraveling the role of mechanical stimulation on smooth muscle cells: a comparative study between 2D and 3D models. Biotechnol Bioeng. 2016;113:2254–63.
Lu D, Kassab GS. Role of shear stress and stretch in vascular mechanobiology. J R Soc Interface. 2011;8:1379–85.
Narita Y, Hata K-I, Kagami H, et al. Novel pulse duplicating bioreactor system for tissue-engineered vascular construct. Tissue Eng. 2004;10:1224–33.
Song L, Zhou Q, Duan P, et al. Successful development of small diameter tissue-engineering vascular vessels by our novel integrally designed pulsatile perfusion-based bioreactor. PloS one 2012; 7.
Visconti R, Mironov V, Kasyanov VA, et al. Cardiovascular tissue engineering I. Perfusion bioreactors: a review. Journal of long-term effects of medical implants 2006; 16.
Bono N, Meghezi S, Soncini M, et al. A dual-mode bioreactor system for tissue engineered vascular models. Ann Biomed Eng. 2017;45:1496–510.
Loy C, Pezzoli D, Candiani G, et al. A cost-effective culture system for the in vitro assembly, maturation, and stimulation of advanced multilayered multiculture tubular tissue models. Biotechnol J. 2018;13:1700359.
Rajan N, Habermehl J, Cote M-F, et al. Preparation of ready-to-use, storable and reconstituted type I collagen from rat tail tendon for tissue engineering applications. Nat Protocols. 2007;1:2753–8. https://doi.org/10.1038/nprot.2006.430.
Zhu S, Yuan Q, Yin T, et al. Self-assembly of collagen-based biomaterials: preparation, characterizations and biomedical applications. Journal of Materials Chemistry B. 2018;6:2650–76.
Achilli M, Mantovani D. Tailoring mechanical properties of collagen-based scaffolds for vascular tissue engineering: the effects of pH, temperature and ionic strength on gelation. Polymers. 2010;2:664–80.
Tiedemann K, Bätge B, Müller PK, et al. Interactions of fibrillin-1 with heparin/heparan sulfate, implications for microfibrillar assembly. J Biol Chem. 2001;276:36035–42.
Kumra H, Nelea V, Hakami H, et al. Fibulin-4 exerts a dual role in LTBP-4L–mediated matrix assembly and function. Proc Natl Acad Sci. 2019;116:20428–37.
El-Hallous E, Sasaki T, Hubmacher D, et al. Fibrillin-1 interactions with fibulins depend on the first hybrid domain and provide an adaptor function to tropoelastin. J Biol Chem. 2007;282:8935–46.
Rueden CT, Schindelin J, Hiner MC, et al. Image J2: ImageJ for the next generation of scientific image data. BMC Bioinformatics. 2017;18:1–26.
Chen Y, Yu Q, Xu C-B. A convenient method for quantifying collagen fibers in atherosclerotic lesions by ImageJ software. Int J Clin Exp Med. 2017;10:14904–10.
Camasão D, Mantovani D. The mechanical characterization of blood vessels and their substitutes in the continuous quest for physiological-relevant performances. A critical review Materials Today Bio. 2021;10:100106.
Meghezi S, Couet F, Chevallier P, et al. Effects of a pseudophysiological environment on the elastic and viscoelastic properties of collagen gels. International Journal of Biomaterials 2012; 2012: Article ID 319290.
Camasão DB, Pérez MG, Palladino S, et al. Elastin-like recombinamers in collagen-based tubular gels improve cell-mediated remodeling and viscoelastic properties. Biomaterials Science 2020.
Camasão DB, Pezzoli D, Loy C, et al. Increasing cell seeding density improves elastin expression and mechanical properties in collagen gel-based scaffolds cellularized with smooth muscle cells. Biotechnol J. 2018;14:1700768.
Papaioannou TG, Stefanadis C. Vascular wall shear stress: basic principles and methods. Hellenic J Cardiol. 2005;46:9–15.
Blackman BR, Garcı´ a-Carden˜ a G, Gimbrone MA Jr. A new in vitro model to evaluate differential responses of endothelial cells to simulated arterial shear stress waveforms. J Biomech Eng. 2002;124:397–407.
Dancu MB, Berardi DE, Heuvel JPV, et al. Atherogenic endothelial cell eNOS and ET-1 responses to asynchronous hemodynamics are mitigated by conjugated linoleic acid. Ann Biomed Eng. 2007;35:1111–9.
Qiu Y, Tarbell JM. Interaction between wall shear stress and circumferential strain affects endothelial cell biochemical production. J Vasc Res. 2000;37:147–57.
Tardy Y, Resnick N, Nagel T, et al. Shear stress gradients remodel endothelial monolayers in vitro via a cell proliferation-migration-loss cycle. Arterioscler Thromb Vasc Biol. 1997;17:3102–6.
Rouleau L, Rossi J, Leask RL. Concentration and time effects of dextran exposure on endothelial cell viability, attachment, and inflammatory marker expression in vitro. Ann Biomed Eng. 2010;38:1451–62.
Trudel J, Massia S. Assessment of the cytotoxicity of photocrosslinked dextran and hyaluronan-based hydrogels to vascular smooth muscle cells. Biomaterials. 2002;23:3299–307.
de Jonge E, Levi M. Effects of different plasma substitutes on blood coagulation: a comparative review. Crit Care Med. 2001;29:1261–7.
Wade CE, Grady J, Kramer GC. Efficacy of hypertonic saline dextran fluid resuscitation for patients with hypotension from penetrating trauma. J Trauma Acute Care Surg. 2003;54:S144–8.
Letcher RL, Chien S, Pickering TG, et al. Direct relationship between blood pressure and blood viscosity in normal and hypertensive subjects: role of fibrinogen and concentration. Am J Med. 1981;70:1195–202.
Massai D, Cerino G, Gallo D, et al. Bioreactors as engineering support to treat cardiac muscle and vascular disease. Journal of healthcare engineering. 2013;4:329–70.
Song L, Zhou Q, Duan P, et al. Successful development of small diameter tissue-engineering vascular vessels by our novel integrally designed pulsatile perfusion-based bioreactor. PLoS One. 2012;7:e42569.
Buttafoco L, Engbers-Buijtenhuijs P, Poot AA, et al. Physical characterization of vascular grafts cultured in a bioreactor. Biomaterials. 2006;27:2380–9.
Schulte J, Friedrich A, Hollweck T, et al. A novel seeding and conditioning bioreactor for vascular tissue engineering. Processes. 2014;2:526–47.
Arrigoni C, Chittò A, Mantero S, et al. Rotating versus perfusion bioreactor for the culture of engineered vascular constructs based on hyaluronic acid. Biotechnol Bioeng. 2008;100:988–97.
Syedain ZH, Meier LA, Bjork JW, et al. Implantable arterial grafts from human fibroblasts and fibrin using a multi-graft pulsed flow-stretch bioreactor with noninvasive strength monitoring. Biomaterials. 2011;32:714–22.
Stock UA, Vacanti JP. Cardiovascular physiology during fetal development and implications for tissue engineering. Tissue Eng. 2001;7:1–7.
Cheema U, Rong Z, Kirresh O, et al. Oxygen diffusion through collagen scaffolds at defined densities: implications for cell survival in tissue models. J Tissue Eng Regen Med. 2012;6:77–84.
Loy C, Lainé A, Mantovani D. Rotation-based technique for the rapid densification of tubular collagen gel scaffolds. Biotechnol J. 2016;11:1673–9.
Li Y-SJ, Haga JH, Chien S. Molecular basis of the effects of shear stress on vascular endothelial cells. J biomech. 2005;38:1949–71.
Urbich C, Walter DH, Zeiher AM, et al. Laminar shear stress upregulates integrin expression: role in endothelial cell adhesion and apoptosis. Circ Res. 2000;87:683–9.
Huang AH and Niklason LE. Engineering biological-based vascular grafts using a pulsatile bioreactor. JoVE (Journal of Visualized Experiments) 2011: e2646.
Durante W, Liao L, Reyna SV, et al. Physiological cyclic stretch directs L-arginine transport and metabolism to collagen synthesis in vascular smooth muscle. FASEB J. 2000;14:1775–83.
Kim B-S, Nikolovski J, Bonadio J, et al. Cyclic mechanical strain regulates the development of engineered smooth muscle tissue. Nat Biotechnol. 1999;17:979–83.
Garanich JS, Pahakis M, Tarbell JM. Shear stress inhibits smooth muscle cell migration via nitric oxide-mediated downregulation of matrix metalloproteinase-2 activity. American Journal of Physiology-Heart and Circulatory Physiology. 2005;288:H2244–52.
Schad JF, Meltzer KR, Hicks MR, et al. Cyclic strain upregulates VEGF and attenuates proliferation of vascular smooth muscle cells. Vascular cell. 2011;3:1–10.
Morrow D, Sweeney C, Birney YA, et al. Cyclic strain inhibits Notch receptor signaling in vascular smooth muscle cells in vitro. Circ Res. 2005;96:567–75.
Fernandez P, Bausch AR. The compaction of gels by cells: a case of collective mechanical activity. Integr Biol. 2009;1:252–9.
Jeong SI, Kim SY, Cho SK, et al. Tissue-engineered vascular grafts composed of marine collagen and PLGA fibers using pulsatile perfusion bioreactors. Biomaterials. 2007;28:1115–22.
Wagenseil JE, Mecham RP. New insights into elastic fiber assembly. Birth Defects Res C Embryo Today. 2007;81:229–40.
Thurmond F, Trotter J. Morphology and biomechanics of the microfibrillar network of sea cucumber dermis. J Exp Biol. 1996;199:1817–28.
Sherratt MJ, Baldock C, Haston JL, et al. Fibrillin microfibrils are stiff reinforcing fibres in compliant tissues. J Mol Biol. 2003;332:183–93.
Patel A, Fine B, Sandig M, et al. Elastin biosynthesis: the missing link in tissue-engineered blood vessels. Cardiovasc Res. 2006;71:40–9.
Noda K, Dabovic B, Takagi K, et al. Latent TGF-β binding protein 4 promotes elastic fiber assembly by interacting with fibulin-5. Proc Natl Acad Sci. 2013;110:2852–7.
Schutte SC, Chen Z, Brockbank KG, et al. Cyclic strain improves strength and function of a collagen-based tissue-engineered vascular media. Tissue Eng Part A. 2010;16:3149–57.
van Haaften EE, Wissing TB, Rutten MC, et al. Decoupling the effect of shear stress and stretch on tissue growth and remodeling in a vascular graft. Tissue Eng Part C Methods. 2018;24:418–29.
Stekelenburg M, Rutten MC, Snoeckx LH, et al. Dynamic straining combined with fibrin gel cell seeding improves strength of tissue-engineered small-diameter vascular grafts. Tissue Eng Part A. 2009;15:1081–9.
Pezzoli D, Di Paolo J, Kumra H, et al. Fibronectin promotes elastin deposition, elasticity and mechanical strength in cellularised collagen-based scaffolds. Biomaterials. 2018;180:130–42.
Acknowledgements
The authors would like to thank Francesco Copes, PhD, for his precious help and guidance all along this research. This work was partially supported by the Natural Sciences and Engineering Research Council of Canada (NSERC to DM and DPR), the NSERC Create Program in Regenerative Medicine, the Canadian Foundation for the Innovation, and the Fonds de Recherche du Québec (Nature et Technologies, and Santé to DM and DPR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Camasão, D.B., Li, L., Drouin, B. et al. Physiologically relevant platform for an advanced in vitro model of the vascular wall: focus on in situ fabrication and mechanical maturation. In vitro models 1, 179–195 (2022). https://doi.org/10.1007/s44164-022-00012-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44164-022-00012-1