Abstract
Objectives
Bystander-applied Automated External Defibrillators (AED) improve outcomes for out-of-hospital cardiac arrest. AED placement is often driven by private enterprise or non-for-profit agencies, which may result in inequitable access. We sought to compare AED availability between four regions in British Columbia (BC).
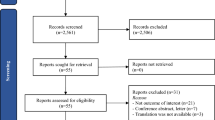
Methods
We identified AEDs (confirmed to be operational) and emergency medical system (EMS)-treated out-of-hospital cardiac arrests (OHCA) from provincial registries. We compared AED availability between BC’s four most populous regions. The primary outcome was the total regional weekly accessible AED-hours per 100,000 population. We also examined: AEDs per 100,000 population and per km2, the ratio of AEDs to OHCA, and the distance from each OHCA to the closest AED.
Results
From provincial registries, we included 879 AEDs from BC’s four most populous regions, where 9333 EMS-treated OHCA occurred over a 5-year period. The most common AED location types were stores, public community centres, and office buildings. Ten percent of AEDs were accessible for all hours. Weekly accessible AED-hours/100,000 population in the four regions were: 3845, 1734, 1594, and 1299. AEDs/100,000 population ranged from 22 to 48, and AEDs/km2 ranged from 0.0048 to 0.20. The number of OHCAs per AED per year ranged from 1.1 to 2.8. The median OHCA-to-closest AED distance ranged from 503 (IQR 244, 947) to 925 (IQR 455, 1501) metres. The regional mean accessibility of individual AEDs ranged between 59 and 79 h per week.
Conclusion
BC’s four most populous regions demonstrate substantial variability in AED accessibility. Further benefit could be derived from AEDs if placed in locations accessible all hours. Our data may encourage community planning efforts to use data-based strategies to systematically place AEDs in optimal locations with strategies to maximize accessibility.
Abstrait
Objectifs
Les défibrillateurs externes automatisés (DEA) appliqués par les témoins améliorent les résultats en cas d’arrêt cardiaque hors hôpital. Le placement des DEA est souvent dirigé par une entreprise privée ou des organismes sans but lucratif, ce qui peut entraîner un accès inéquitable. Nous avons cherché à comparer la disponibilité des DEA entre quatre régions de la Colombie-Britannique.
Méthodes
Nous avons identifié les DEA (dont la mise en service a été confirmée) et les SMU (système médical d’urgence) traités par arrêt cardiaque hors hôpital (AHC) dans les registres provinciaux. Nous avons comparé la disponibilité des DEA entre les quatre régions les plus peuplées de la Colombie-Britannique. Le résultat principal était le nombre total d’heures de DEA accessibles hebdomadaires par région pour 100000 habitants. Nous avons également examiné : les DEA par 100000 habitants et par km2, le rapport entre les DEA et l’AHCA, et la distance entre chaque AHCA et le DEA le plus proche.
Résultats
À partir des registres provinciaux, nous avons inclus 879 DEA des quatre régions les plus peuplées de la Colombie-Britannique, où 9333 OHCA traités par les SMU se sont produits sur une période de 5 ans. Les types de DEA les plus courants étaient les magasins, les centres communautaires publics et les immeubles de bureaux. Dix pour cent des DEA étaient accessibles toutes les heures. La population hebdomadaire accessible en heures AED/100000 habitants dans les quatre régions était de 3845, 1734, 1594 et 1299. Le nombre de DEA/100 000 habitants variait de 22 à 48, et le nombre de DEA/km2 variait de 0,018 à 0,018. Le nombre de CASO par DEA par année variait de 1,1 à 2,8. La distance médiane entre le DEA OHCA et le DEA le plus proche variait de 503 mètres (IQR 244, 947) à 925 mètres (IQR 455, 1501). L’accessibilité moyenne régionale des DEA individuels variait entre 59 et 79 heures par semaine.
Conclusion
Les quatre régions les plus populeuses de la Colombie-Britannique présentent une variabilité importante de l’accessibilité aux DEA. D’autres avantages pourraient découler des DEA s’ils sont placés dans des endroits accessibles toutes les heures. Nos données peuvent encourager les efforts de planification communautaire à utiliser des stratégies fondées sur les données pour placer systématiquement les DEA dans des endroits optimaux avec des stratégies pour maximiser l’accessibilité.
Similar content being viewed by others
References
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics’2017 update: a report from the American Heart Association. vol. 135, Circulation. 2017. p. 146–603.
Chan PS, McNally B, Tang F, Kellermann A, CARES Surveillance Group. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation [Internet]. 2014;130(21):1876–82.
Daya MR, Schmicker RH, Zive DM, Rea TD, Nichol G, Buick JE, et al. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation [Internet]. 2015;91:108–15.
Hallstrom AP, Ornato J, Weisfeldt M. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):637–46.
Grunau B, Kawano T, Dick W, Straight R, Connolly H, Schlamp R, et al. Trends in care processes and survival following prehospital resuscitation improvement initiatives for out-of-hospital cardiac arrest in British Columbia, 2006–2016. Resuscitation [Internet]. 2018;125:118–25.
Weisfeldt ML, Sitlani CM, Ornato JP, Rea T, Aufderheide TP, Davis D, et al. Survival after application of automatic external defibrillators before arrival of the emergency medical system: evaluation in the resuscitation outcomes consortium population of 21 million. J Am Coll Cardiol [Internet]. 2010;55(16):1713–20.
Nagase A, Kaneko H, Hatanaka T, Marukawa S, Sakamoto T. A mismatch of spatial distribution between AED installation and out-of-hospital cardiac arrest. Resuscitation. 2019;142:e50.
Tsukigase K, Tanaka H, Takyu H, Tsukigase K, Tanaka H, Takyu H. Mismatch between sites of incidence of out-of-hospital cardiac arrest and locations of installed automated external defibrillator in the Tokyo Metropolitan area. World J Cardiovasc Dis. 2017;07(06):185–94.
Statistics Canada. Census Profile, 2016 Census British Columbia [Province] and Canada [Country] [Internet]. [cited 2020 Jul 17]. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=PR&Code1=59&Geo2=PR&Code2=01&SearchText=Canada&SearchType=Begins&SearchPR=01&B1=All&type=0. Accessed 17 July 2020.
Government of BC. Municipalities in B.C. [Internet]. 2020 [cited 2020 Jul 17]. https://www2.gov.bc.ca/gov/content/governments/local-governments/facts-framework/systems/municipalities. Accessed 17 July 2020.
Heart and Stroke Foundation. BC and Yukon Advocacy Achievements [Internet]. [cited 2023 Jun 5]. Available from: https://www.heartandstroke.ca/how-you-can-help/advocate/bc-and-yukon-advocacy-achievements. Accessed 17 July 2020.
Heart and Stroke Foundation. Public Access to Defibrillation Program [Internet]. [cited 2023 Jan 20]. https://www.heartandstroke.ca/-/media/pdf-files/yukon/advocacy/bc20pad20program20overview2013.pdf?rev=2c5e833cf6984ad4b03d7f263b64a911. Accessed 17 July 2020.
BC Emergency Health Services. BCEHS: PulsePoint CPR App.
Statistics Canada. Population Centre and Rural Area Classification 2016 [Internet]. Statistics Canada Catalogue. 2016 [cited 2020 Jul 17]. https://www.statcan.gc.ca/en/subjects/standard/pcrac/2016/introduction#. Accessed 17 July 2020.
Ni Y-M, Rusinaru C, Reinier K, Uy-Evanado A, Chugh H, Stecker EC, et al. Unexpected shift in circadian and septadian variation of sudden cardiac arrest: the Oregon Sudden Unexpected Death Study. Hear Rhythm. 2019;16(3):411–5.
Hansen CM, Wissenberg M, Weeke P, Ruwald MH, Lamberts M, Lippert FK, et al. Automated external defibrillators inaccessible to more than half of nearby cardiac arrests in public locations during evening, nighttime, and weekends. Circulation. 2013;128(20):2224–31.
Srinivasan S, Salerno J, Hajari H, Weiss LS, Salcido DD. Modeling a novel hypothetical use of postal collection boxes as automated external defibrillator access points. Resuscitation. 2017;120:26.
Tsai YS, Ko PCI, Huang CY, Wen TH. Optimizing locations for the installation of automated external defibrillators (AEDs) in urban public streets through the use of spatial and temporal weighting schemes. Appl Geogr. 2012;35(1–2):394.
Karam N, Narayanan K, Bougouin W, Benameur N, Beganton F, Jost D, et al. Major regional differences in Automated External Defibrillator placement and Basic Life Support training in France: Further needs for coordinated implementation. Resuscitation [Internet]. 2017;118:49–54.
Kjølbye J, Karlsson L, Lippert F, Hansen C, Andelius L, Møller S, et al. 66 Regional variations in aed deployment, accessibility and early defibrillation: a nationwide study. In: Abstracts [Internet]. British Medical Journal Publishing Group; 2018. p. A25.1–A25. https://doi.org/10.1136/bmjopen-2018-EMS.66
Blom MT, Beesems SG, Homma PCM, Zijlstra JA, Hulleman M, Van Hoeijen DA, et al. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130(21):1868–75.
Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, et al. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):637–46.
Blackwood J, Mancera M, Bavery S, Carbon C, Daya M, VanKeulen B, et al. Improving response to out-of-hospital cardiac arrest: the verified responder program pilot. Resuscitation [Internet]. 2020;154:1.
Andelius L, Malta Hansen C, Jonsson M, Gerds TA, Rajan S, Torp-Pedersen C, et al. Smartphone-activated volunteer responders and bystander defibrillation for out-of-hospital cardiac arrest in private homes and public locations. Eur Hear Journal Acute Cardiovasc Care [Internet]. 2023;12(2):87–95. https://academic.oup.com/ehjacc/article/12/2/87/6961720. Accessed 17 July 2020.
Smith CM, Lall R, Fothergill RT, Spaight R, Perkins GD. The effect of the GoodSAM volunteer first-responder app on survival to hospital discharge following out-of-hospital cardiac arrest. Eur Hear Journal Acute Cardiovasc Care [Internet]. 2022;11(1):20–31. https://academic.oup.com/ehjacc/article/11/1/20/6431742. Accessed 17 July 2020.
Grunau B, Bal J, Scheuermeyer F, Guh D, Dainty KN, Helmer J, et al. Bystanders are less willing to resuscitate out-of-hospital cardiac arrest victims during the COVID-19 pandemic. Resusc Plus. 2020;4: 100034.
Oh JH, Cho GC, Ryoo SM, Han SH, Woo SH, Jang YS, et al. Mismatches between the number of installed automated external defibrillators and the annual rate of automated external defibrillator use among places. Prehosp Disaster Med [Internet]. 2021;36(2):183–8. https://www.cambridge.org/core/product/identifier/S1049023X20001508/type/journal_article. Accessed 17 July 2020.
Moon S, Vadeboncoeur TF, Kortuem W, Kisakye M, Karamooz M, White B, et al. Analysis of out-of-hospital cardiac arrest location and public access defibrillator placement in Metropolitan Phoenix, Arizona. Resuscitation. 2015;89:43–9.
Sun CLF, Karlsson L, Morrison LJ, Brooks SC, Folke F, Chan TCY. Effect of optimized versus guidelines-based automated external defibrillator placement on out-of-hospital cardiac arrest coverage: an in silico trial. J Am Heart Assoc [Internet]. 2020. https://doi.org/10.1161/JAHA.120.016701.
Sun CLF, Karlsson L, Torp-Pedersen C, Morrison LJ, Folke F, Chan TCY. Spatiotemporal AED optimization is generalizable. Resuscitation [Internet]. 2018;131:101–7.
Acknowledgements
The BC Cardiac Arrest Registry is funded by the Heart and Stroke Foundation of Canada, and benefits from in-kind support from Province Health Care, BC Emergency Health Services, and Provincial Health Services Authority
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, Z.H., Heidet, M., Bal, J. et al. Regional variation in accessibility of automated external defibrillators in British Columbia. Can J Emerg Med 26, 23–30 (2024). https://doi.org/10.1007/s43678-023-00610-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-023-00610-2