Abstract
Purpose
Sickle cell disease (SCD) is an inherited blood disorder with a natural course punctuated by acute complications including painful vaso-occlusive episodes. The objectives were: (1) to determine what proportion of patients with SCD receive opioids within 30 min of triage as recommended by the current clinical recommendations and quality standard; and (2) to identify facilitators to timely opioid administration for patients with SCD.
Methods
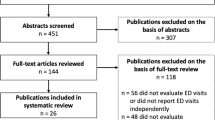
This was a retrospective observational study. The primary outcome was the proportion of visits in which patients received opioid analgesia within 30 min of triage. Secondary outcomes were time in minutes from triage to any analgesic administration and time from triage to first opioid administration. Patient demographics and ED encounter characteristics were included as potential associated variables.
Results
There were 236 patient visits (by 103 patients) that met inclusion criteria. Patients received opioid analgesia within 30 min of triage in only 5.2% of visits. The median time from triage to opioid analgesia was 80 (IQR = 49.0, 125.5) minutes. Using an order set and receiving opioid analgesia prior to physician assessment were both associated with shorter times to opioid analgesia.
Conclusion
Existing recommendations are that opioid analgesia be provided within 30 min of triage for patients with SCD and VOEs. Our data show this target is rarely met, even in a department in which SCD VOEs are a common presenting concern. The association of earlier opioid analgesia with order set use and administration prior to physician assessment highlights potential avenues for improving time to analgesia.
Résumé
Objectif
La drépanocytose (ou l'anémie falciforme) est une maladie héréditaire du sang dont l'évolution naturelle est ponctuée de complications aiguës, notamment des épisodes vaso-occlusifs douloureux. Les objectifs étaient : (1) de déterminer quelle proportion de patients atteints de drépanocytose reçoivent des opioïdes dans les 30 minutes suivant le triage, comme le recommandent les recommandations cliniques et la norme de qualité actuelles ; et (2) d'identifier les facteurs facilitant l'administration rapide d'opioïdes aux patients atteints de drépanocytose.
Méthodes
Il s'agissait d'une étude observationnelle rétrospective. Le critère de jugement principal était la proportion de visites au cours desquelles les patients ont reçu une analgésie opioïde dans les 30 minutes suivant le triage. Les critères de jugement secondaires étaient le temps en minutes écoulé entre le triage et l'administration de tout analgésique et le temps écoulé entre le triage et la première administration d'opioïdes. Les caractéristiques démographiques des patients et les caractéristiques des rencontres aux urgences ont été incluses comme variables potentiellement associées.
Résultats
Il y a eu 236 visites de patients (par 103 patients) qui répondaient aux critères d'inclusion. Les patients ont reçu une analgésie opioïde dans les 30 minutes suivant le triage dans seulement 5,2 % des visites. Le temps médian écoulé entre le triage et l'analgésie opioïde était de 80 (IQR = 49,0, 125,5) minutes. L'utilisation d'un ensemble de commandes et la réception d'une analgésie opioïde avant l'évaluation du médecin étaient toutes deux associées à des temps plus courts d'analgésie opioïde.
Conclusions
Les recommandations existantes sont que l'analgésie opioïde soit fournie dans les 30 minutes suivant le triage pour les patients atteints de drépanocytose et d'EVO. Nos données montrent que cet objectif est rarement atteint, même dans un service où les EVO de la drépanocytose sont une préoccupation courante. L'association d'une analgésie opioïde plus précoce avec l'utilisation d'un ensemble de commandes et l'administration avant l'évaluation du médecin met en évidence des pistes potentielles pour améliorer le temps d'analgésie.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, JB within the limits of the project’s research ethics board waiver.
References
Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, et al. Mortality in sickle cell disease Life expectancy and risk factors for early death. N Engl J Med. 1994;330(23):1639–44.
Benjamin LJ, Swinson GI, Nagel RL. Sickle cell anemia day hospital: an approach for the management of uncomplicated painful crises. Blood. 2000;95(4):1130–6.
Mager A, Pelot K, Koch K, Miller L, Hubler C, Ndifor A, et al. Opioid management strategy decreases admissions in high-utilizing adults with sickle cell disease. J Opioid Manag. 2017;13(3):143–56.
Chan D, Kouyoumdjian F, Athale U, Pendergrast J, Verhovsek M. Emergency department quality of care for sickle cell disease in Ontario, Canada: a population-based matched cohort study. Blood. 2020;136(1):38–9.
Glassberg JA, Tanabe P, Chow A, Harper K, Haywood C Jr, DeBaun MR, et al. Emergency provider analgesic practices and attitudes toward patients with sickle cell disease. Ann Emerg Med. 2013;62(4):293–302.
Lazio MP, Costello HH, Courtney DM, Martinovich Z, Myers R, Zosel A, et al. A comparison of analgesic management for emergency department patients with sickle cell disease and renal colic. Clin J Pain. 2010;26(3):199–205.
Tunji-Ajayi, L., Jemitola, S.,Darkwa,M.,Verhovsek, M., Kirby-Allen, M., Williams, S.Bryan, J. Identifying hospitals in need of education to provide optimal care for patients living with Sickle Cell Disease in Ontario - Sickle Cell Awareness Group of Ontario [Internet]. 2020 [cited 2022 Nov 18]. Available from: https://sicklecellanemia.ca/identifying-hospitals-in-need-of-education-to-provide-optimal-care-for-patients-living-with-scd-in-ontario
Cacciotti C, Vaiselbuh S, Romanos-Sirakis E. Pain management for sickle cell disease in the pediatric emergency department: medications and hospitalization trends. Clin Pediatr (Phila). 2017;56(12):1109–14.
Health Quality Ontario. Sickle Cell Disease: Care for people of all ages [Internet]. [cited 2023 Mar 20]. Available from: https://hqontario.ca/Evidence-to-Improve-Care/Quality-Standards/View-all-Quality-Standards/Sickle-Cell-Disease
Clinical Handbook for Sickle Cell Disease Vaso-occlusive Crisis [Internet]. Ministry of Health and Long-Term Care; 2017. Available from: http://www.health.gov.on.ca/en/pro/programs/ecfa/docs/hb_sickle.pdf
Gillis VL, Senthinathan A, Dzingina M, Chamberlain K, Banks E, Baker MR, et al. Management of an acute painful sickle cell episode in hospital: summary of NICE guidance. BMJ. 2012;27(344):e4063.
Brandow AM, Carroll CP, Creary S, Edwards-Elliott R, Glassberg J, Hurley RW, et al. American Society of Hematology 2020 guidelines for sickle cell disease: management of acute and chronic pain. Blood Adv. 2020;4(12):2656–701.
Scotch RK. Nothing about us without us: disability rights in America. OAH Mag Hist. 2009;23(3):17–22.
Kelly GS, Stewart RW, Strouse JJ, Anders JF. Intranasal fentanyl improves time to analgesic delivery in sickle cell pain crises. Am J Emerg Med. 2018;36(7):1305–7.
Arnold T, Jr RLC, Rosenberg L, Jacob SA, Thompson S, Saavedra H, et al. A Quality Improvement Initiative to Decrease Time to Analgesia in Patients With Sickle Cell and Vaso-Occlusive Crisis: A Population With Disparities in Treatment. Cureus [Internet]. 2022 Sep 25 [cited 2022 Dec 23];14(9). Available from: https://www.cureus.com/articles/108554-a-quality-improvement-initiative-to-decrease-time-to-analgesia-in-patients-with-sickle-cell-and-vaso-occlusive-crisis-a-population-with-disparities-in-treatment
Seaser J, Thomson J, Brunsman A, Patel N. Evaluation of guideline-recommended pain management in acute sickle cell crisis and its effect on patient outcomes. J Pain Palliat Care Pharmacother. 2022;36(3):152–8.
Tanabe P, Myers R, Zosel A, Brice J, Ansari AH, Evans J, et al. Emergency department management of acute pain episodes in sickle cell disease. Acad Emerg Med. 2007;14(5):419–25.
Ostrom C, Bair E, Maixner W, Dubner R, Fillingim RB, Ohrbach R, et al. Demographic predictors of pain sensitivity: results from the OPPERA study. J Pain Off J Am Pain Soc. 2017;18(3):295–307.
Saastamoinen P, Leino-Arjas P, Laaksonen M, Lahelma E. Socio-economic differences in the prevalence of acute, chronic and disabling chronic pain among ageing employees. Pain. 2005;114(3):364–71.
Mitchell R, Kelly AM, Kerr D. Does emergency department workload adversely influence timely analgesia? Emerg Med Australas. 2009;21(1):52–8.
Tozer AP, Belanger P, Moore K, Caudle J. Socioeconomic status of emergency department users in Ontario, 2003 to 2009. CJEM. 2014;16(03):220–5.
https://ctas-phctas.ca/ [Internet]. [cited 2021 Dec 28]. Available from: https://ctas-phctas.ca/
McHugh M. Interrater reliability: the kappa statistic. Biochem Med Časopis Hrvat Druš Med Biokem HDMB. 2012;3(22):276–82.
SAS. SAS [Internet]. SAS. [cited 2023 Mar 20]. Available from: https://www.sas.com/en_ca/curiosity.html
Arendts G, Fry M. Factors associated with delay to opiate analgesia in emergency departments. J Pain. 2006;7(9):682–6.
Wachnik AA, Welch-Coltrane JL, Adams MC, Blumstein HA, Pariyadath M, Robinson SG, et al. A Standardized emergency department order set decreases admission rates and in-patient length of stay for adults patients with sickle cell disease. Pain Med. 2022;23(12):2050–60.
Balsamo L, Shabanova V, Carbonella J, Szondy MV, Kalbfeld K, Thomas DA, et al. Improving care for sickle cell pain crisis using a multidisciplinary approach. Pediatrics. 2019. https://doi.org/10.1542/peds.2018-2218.
Co JPT, Johnson KB, Duggan AK, Casella JF, Wilson M. Does a clinical pathway improve the quality of care for sickle cell anemia? Jt Comm J Qual Saf. 2003;29(4):181–90.
Andemariam B, Odesina V, Owarish-Gross J, Grady J, Gorenbeyn A, Powell A, et al. (254) A fast-track emergency department acute sickle cell pain management algorithm results in fewer hospital admissions, decreased length of stay and increased hospital revenue. J Pain. 2014;15(4):S39.
Matthie N, Jenerette C. Sickle cell disease in adults: developing an appropriate care plan. Clin J Oncol Nurs. 2015;19(5):562.
Morse BL, Carmichael AE, Bradford VA, Pollard AL. Sickle Cell Disease Care Planning for School Nurses. NASN Sch Nurse. 2022;37(1):48–54.
Tanabe P, Spratling R, Smith D, Grissom P, Hulihan M. Understanding the complications of sickle cell disease. Am J Nurs. 2019;119(6):26.
Odesina V, Bellini S, Leger R, Bona R, Delaney C, Andemariam B, et al. Evidence-based sickle cell pain management in the emergency department. Adv Emerg Nurs J. 2010;32(2):102–11.
O’Connor S, Hanes D, Lindsey A, Weiss M, Petty L, Overcash J. Attitudes among healthcare providers and patients diagnosed with sickle cell disease. Clin J Oncol Nurs. 2014;18(6):675.
Atkinson P, McGeorge K, Innes G. Saving emergency medicine: is less more? Can J Emerg Med. 2022;24(1):9–11.
Bryan JM, Alavian S, Giffin D, LeBlanc C, Liu J, Phalpher P, et al. CAEP 2021 academic symposium: recommendations for addressing racism and colonialism in emergency medicine. Can J Emerg Med. 2022;1:1–7.
Acknowledgements
We thank the Sickle Cell Awareness Group of Ontario, the Sickle Cell Association of Ontario, the University Health Network Emergency Department Quality Improvement Committee (especially Dr. Joseph Choi), the University Health Network Emergency Department Sickle Cell Working Group and the University Health Network Red Blood Cell Disorders Clinic for their advice and expertise in completing this work, and Dr. Alex Kiss for his biostatistical expertise. The authors would also like to acknowledge the Black Physicians Association of Ontario for their role in connecting physicians, patients, and community members for the advancement of care for those living with sickle cell disease.
University Health Network Emergency Department Sickle Cell Working Group: Lame Tunji-Ajayi, Serena Thompson, Ruth Appiah-Boateng, Jennifer Bryan, Kaitlin Azubuike, Ulysse Guerrier, Markus Gulilat, Jennifer Hulme, Lance Armstrong, Marie-Pascale Poku, Karen Fleming, Nia Navarro, Hasan Sheikh, Tricia Williams, Betty Lulseged.
Funding
This work was funded by the University Health Network Physician Council on Quality and Safety and the University Health Network Summer Training and Research in Emergency Medicine (STAR-EM) program. This manuscript is the work of the authors and not their institutions.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
MG declares that he has no conflict of interest. LTA has received research grants/funding/honoraria from the Public Health Agency of Canada/is a consultant with Novartis Inc and Roche Inc. ST has received research grants/funding/honoraria from/is a member of Healthcare Excellence Canada. MPP declares that she has no conflict of interest, RAB declares that she has no conflict of interest. NN declares that she has no conflict of interest, HS declares no conflict of interest. JH is the director of the University of Toronto Global Health Emergency Medicine and receives a stipend from the UHN Emergency Department as an Equity co-lead, JB is the chair of the Canadian Association of Emergency Physicians Committee on Antiracism and Anticolonialism and is a Canadian Association of Emergency Physicians equity, diversity, and inclusion advisor.
Additional information
Communicated by Catherine Varner.
The members of the instutional author group “the University Health Network Emergency Department Sickle Cell Working Group” was processed under acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gulilat, M., Tunji-Ajayi, L., Thompson, S. et al. Pain management in adult patients with sickle cell disease in the emergency department: how does current practice compare with existing standards of care?. Can J Emerg Med 25, 836–844 (2023). https://doi.org/10.1007/s43678-023-00579-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-023-00579-y