Abstract
Objectives
With the launch of competence by design (CBD) in emergency medicine (EM) in Canada, there are growing recommendations on the use of simulation for the training and assessment of residents. Many of these recommendations have been suggested by educational leaders and often exclude the resident stakeholder. This study sought to explore their experiences and perceptions of simulation in CBD.
Methods
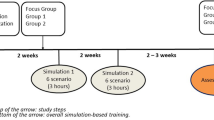
Qualitative data were collected from November 2020 to May 2021 at McMaster University and the University of Toronto after receiving ethics approval from both sites. Eligible participants included EM residents who were interviewed by a trained interviewer using a semi-structured interview guide. All interviews were recorded, transcribed, coded, and collapsed into themes. Data analysis was guided by constructivist grounded theory.
Results
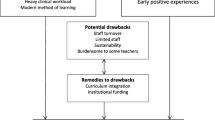
A total of seventeen residents participated. Thematic analysis revealed three major themes: 1) impact of CBD on resident views of simulation; 2) simulation’s role in obtaining entrustable professional activities (EPAs) and filling educational gaps; and 3) conflicting feelings on the use of high-stakes simulation-based assessment in CBD.
Conclusions
EM residents strongly support using simulation in CBD and acknowledge its ability to bridge educational gaps and fulfill specific EPAs. However, this study suggests some unintended consequences of CBD and conflicting views around simulation-based assessment that challenge resident perceptions of simulation as a safe learning space. As CBD evolves, educational leaders should consider these impacts when making future curricular changes or recommendations.
Résumé
Objectifs
Avec le lancement de la compétence par conception (CPC) en médecine d'urgence (MU) au Canada, il existe des recommandations croissantes sur l'utilisation de la simulation pour la formation et l'évaluation des résidents. Beaucoup de ces recommandations ont été suggérées par des leaders éducatifs et excluent souvent la partie prenante résidente. Cette étude visait à explorer leurs expériences et leurs perceptions de la simulation dans la CPC.
Méthodes
Des données qualitatives ont été collectées de novembre 2020 à mai 2021 à l'Université McMaster et à l'Université de Toronto après avoir reçu l'approbation éthique des deux sites. Les participants éligibles étaient des résidents en MU qui ont été interviewés par un interviewer formé à l'aide d'un guide d'entretien semi-structuré. Toutes les interviews ont été enregistrées, transcrites, codées et regroupées en thèmes. L'analyse des données a été guidée par la théorie ancrée constructiviste.
Résultats
Au total, dix-sept résidents ont participé. L'analyse thématique a révélé trois thèmes majeurs : (1) l'impact de la CPC sur les opinions des résidents sur la simulation ; (2) le rôle de la simulation dans l'obtention des activités professionnelles confiables (APC) et le comblement des lacunes éducatives ; et (3) des sentiments contradictoires sur l'utilisation de l'évaluation basée sur la simulation à hauts enjeux dans la CPC.
Conclusions
Les résidents en MU soutiennent fortement l'utilisation de la simulation dans la CPC et reconnaissent sa capacité à combler les lacunes éducatives et à remplir des APC spécifiques. Cependant, cette étude suggère quelques conséquences imprévues de la CPC et des opinions divergentes sur l'évaluation basée sur la simulation qui remettent en question les perceptions des résidents de la simulation comme un espace d'apprentissage sécuritaire. À mesure que la CPC évolue, les leaders éducatifs devraient tenir compte de ces impacts lorsqu'ils apportent des changements ou des recommandations curriculaires futurs.
Similar content being viewed by others
References
Royal College of Physicians and Surgeons (RCPSC). Entrustable professional activities for emergency medicine. Ottawa (ON); 2018
Dagnone JD, Hall AK, Sebok-Syer S, Klinger D, Woolfrey K, Davison C, Ross J, McNeil G, Moore S. Competency-based simulation assessment of resuscitation skills in emergency medicine postgraduate trainees–a Canadian multi-centred study. Can Med Educ J. 2016;7(1): e57.
Kester-Greene N, Hall AK, Walsh CM. Simulation curricular content in postgraduate emergency medicine: a multicentre Delphi study. Can J Emerg Med. 2019;21:667.
Chaplin T, Thoma B, Petrosoniak A, Caners K, McColl T, Forristal C, et al. Simulation-based research in emergency medicine in Canada: priorities and perspectives. Can J Emerg Med. 2019;22:103.
Russell E, Hall AK, Hagel C, Petrosoniak A, Dagnone JD, Howes D. Simulation in Canadian postgraduate emergency medicine training—a national survey. Can J Emerg Med. 2018;20:132.
Cheng A, Bhanji F. A call to action: the future of simulation-based research in emergency medicine in Canada. Can J Emerg Med. 2019;22:8.
Walsh CM, Garg A, Ng SL, Goyal F, Grover SC. Residents’ perceptions of simulation as a clinical learning approach. Can Med Educ J. 2017;8:e76.
Boet S, Sharma S, Goldman J, Reeves S. Review article: medical education research: an overview of methods. Can J Anesth. 2012;59(2):159–70.
Fritz PZ, Gray T, Flanagan B. Review of mannequin-based high-fidelity simulation in emergency medicine. EMA Emerg Med Australas. 2008;20:1.
Huynh C, Wong-Chong N, Vourtzoumis P, Lim S, Marini W, Johal G, et al. The future of general surgery training: a Canadian resident nationwide Delphi consensus statement. Surg US. 2019. https://doi.org/10.1016/j.surg.2019.04.025.
Ross S, Poth CA, Donoff MG, Papile C, Humphries P, Stasiuk S, et al. Involving users in the refinement of the competency-based achievement system: An innovative approach to competency-based assessment. Med Teach. 2012. https://doi.org/10.3109/0142159X.2012.644828.
Hall AK, Chaplin T, Mccoll T, Petrosoniak A, Caners K, Rocca N, et al. Harnessing the power of simulation for assessment: Consensus recommendations for the use of simulation-based assessment in emergency medicine. Can J Emerg Med. 2020. https://doi.org/10.1017/cem.2019.488.
Boursicot K, Etheridge L, Setna Z, Sturrock A, Ker J, Smee S, et al. Performance in assessment: consensus statement and recommendations from the Ottawa conference. Med Teacher. 2011;33:370.
Watling CJ, Ginsburg S. Assessment, feedback and the alchemy of learning. Med Educ. 2019. https://doi.org/10.1111/medu.13645.
Mills J, Bonner A, Francis K. The development of constructivist grounded theory. Int J Qual Methods. 2006. https://doi.org/10.1177/160940690600500103.
Charmaz K. Constructionism and the grounded theory method. In: Holstein J-A, Gubrium J-F, editors. Handbook of constructionist research. New York: Guilford; 2008. p. 397–412.
Charmaz K. Constructing grounded theory: a practical guide through qualitative research. London: Sage Publications Ltd; 2006.
Rudolph JW, Raemer DB, Simon R. Establishing a safe container for learning in simulation: the role of the presimulation briefing. Simul Healthcare. 2014;9(6):339–49.
Kolbe M, Eppich W, Rudolph J, Meguerdichian M, Catena H, Cripps A, Grant V, Cheng A. Managing psychological safety in debriefings: a dynamic balancing act. BMJ Simul Technol Enhanced Learn. 2020;6(3):164.
Turner S, Harder N. Psychological safe environment: a concept analysis. Clin Simul Nurs. 2018;1(18):47–55.
Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio C, Swing SR, Harris P, Glasgow NJ, Campbell C, Dath D, Harden RM. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638–45.
LeBlanc VR, Bould MD, McNaughton N, Brydges R, Piquette D, Sharma B. 2011 Simulation in postgraduate medical education. Members of the FMEC PG consortium
Thoma B, Hall AK, Clark K, Meshkat N, Cheung WJ, Desaulniers P, Ffrench C, Meiwald A, Meyers C, Patocka C, Beatty L. Evaluation of a national competency-based assessment system in emergency medicine: a CanDREAM study. J Grad Med Educ. 2020;12(4):425–34.
Costello L, Argintaru N, Wong A, Simard R, Chacko M, Meshkat N. MP18: Addressing unrealistic expectations: a novel transition to discipline curriculum in emergency medicine. Can J Emerg Med. 2019;21(S1):S48.
Pandya A, Patocka C, Huffman J. Simulation for assessment of entrustable professional activities in an emergency medicine residency program. Can J Emerg Med. 2022;1:1–4.
Upadhyaya S, Rashid M, Davila Cervantes A, Oswald A. Exploring resident perceptions of initial competency based medical education implementation. Can Med Educ Journal/Revue canadienne de l’éducation médicale. 2021;12(2):e42-56.
Ott MC, Pack R, Cristancho S, Chin M, Van Koughnett JA, Ott M. “The most crushing thing”: understanding resident assessment burden in a competency-based curriculum. J Grad Med Educ. 2022;14(5):583–92.
Royal College Staff. Commitment to Action|Statement on enhanced flexibility for CBD program implementation [Internet]. Ottawa, Canada: Royal College of Physicians and Surgeons; 2023 May 17. Available from: https://newsroom.royalcollege.ca/commitment-to-action-statement-on-enhanced-flexibility-for-cbd-program-implementation. Accessed 26 May 2023
Funding
This study was funded by a Canadian Association of Emergency Physicians and Schwartz/Reisman Emergency Medicine Institute (CAEP-SREMI) 2020 Junior Investigator Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The study authors declare no competing interests.
Additional information
Communicated by Catherine Patocka.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Costello, L.L., Cho, D.D., Daniel, R.C. et al. Emergency medicine resident perceptions of simulation-based training and assessment in competence by design. Can J Emerg Med 25, 828–835 (2023). https://doi.org/10.1007/s43678-023-00577-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-023-00577-0