Abstract
Introduction
Current guidelines suggest adjuvant antibiotics after incision and drainage (I&D) of small, uncomplicated abscesses may improve patient outcomes, minimize pain, and prevent recurrence. The objective was to explore antibiotic prescribing at ED discharge and describe patient outcomes.
Methods
This was a health records review of adult patients (≥ 18 years) discharged from an academic hospital ED (annual census 65,000) over a 2-year period with diagnosis of an uncomplicated skin abscess. Outcomes included any unplanned return ED visits within 30 days, repeat I&D, and escalation to intravenous (IV) antibiotics.
Results
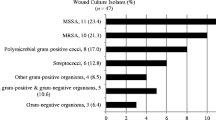
Of 389 ED visits, 85.6% patients underwent I&D, of which 62.2% were prescribed antibiotics at discharge. Of these patients, 36.7% received guideline recommended antibiotics (TMP-SMX or clindamycin). Of all patients who underwent I&D, 13.2% had an unplanned return ED visit within 30 days, 6.9% required repeat I&D, and 0.6% patients were escalated to IV antibiotics. Patients treated with cefalexin were more likely to have an unplanned return ED visit within 30 days (20.0 vs 5.3%; Δ14.7, 95% CI 4.6–24.4), and were more likely to have a repeat I&D within 30 days (13.7 vs 0%; Δ13.7, 95% CI 6.4–22.0), compared to patients prescribed guideline recommended antibiotics. Treatment with guideline recommended antibiotics reduced treatment failure significantly in MRSA positive patients (0.0 vs 44.4%; Δ44.4, 95% CI 13.4–73.3).
Conclusions
Antibiotics were prescribed for most abscesses that underwent I&D. Less than half of the patients received antibiotics that were guideline recommended. Compared to those who received cefalexin, patients prescribed TMP-SMX or clindamycin had fewer return ED visits and were less likely to have a repeat I&D within 30 days. However, adjuvant antibiotic use did not significantly improve outcomes overall, with most patients not requiring a change in management irrespective of antibiotic use.
Résumé
Objectifs
Les lignes directrices actuelles suggèrent que les adjuvants aux antibiotiques après l’incision et le drainage (I&D) des petits abcès simples peuvent améliorer les résultats pour les patients, réduire la douleur et prévenir la récidive. L'objectif était d'explorer la prescription d'antibiotiques à la sortie des urgences et de décrire les résultats pour les patients.
Méthodes
Il s'agissait d'une étude des dossiers médicaux des patients adultes (≥ 18 ans) sortis des urgences d'un hôpital universitaire (recensement annuel 65 000) sur une période de deux ans avec un diagnostic d'abcès cutané non compliqué. Les résultats comprenaient toutes les visites de retour non planifiées aux urgences dans les 30 jours, la répétition de l'I&D et l'escalade vers des antibiotiques intraveineux (IV).
Résultats
Sur 389 visites aux urgences, 85,6 % des patients ont subi une I&D, dont 62,2 % se sont vu prescrire des antibiotiques à la sortie. Parmi ces patients, 36,7 % ont reçu les antibiotiques recommandés par les directives (TMP-SMX ou clindamycine). Sur l'ensemble des patients ayant subi une I&D, 13,2 % ont eu une visite non planifiée aux urgences dans les 30 jours, 6,9 % ont dû subir une nouvelle I&D et 0,6 % des patients ont eu recours à une antibiothérapie IV. Les patients traités par la céfalexine étaient plus susceptibles d'avoir une visite de retour imprévue à l'urgence dans les 30 jours 20,0 % vs 5,3 % ; Δ14,7, IC 95 % : 4,6 à 24,4), et étaient plus susceptibles d’avoir une I&D répétée dans les 30 jours (13,7 % vs 0 % ; Δ13,7, IC 95 % : 6,4 à 22,0), par rapport aux patients auxquels on a prescrit des antibiotiques recommandés par les lignes directrices. Le traitement avec les antibiotiques recommandés par les lignes directrices a réduit de manière significative l'échec thérapeutique chez les patients positifs au SARM (0,0 % vs 44,4 % ; Δ44,4, IC 95 % : 13,4 à 73,3).
Conclusions
Des antibiotiques ont été prescrits pour la plupart des abcès ayant fait l'objet d'une I&D. Moins de la moitié des patients ont reçu des antibiotiques recommandés par les lignes directrices. Par rapport à ceux qui ont reçu de la céfalexine, les patients à qui l'on a prescrit du TMP-SMX ou de la clindamycine ont eu moins de visites de retour aux urgences et étaient moins susceptibles de subir une nouvelle I&D dans les 30 jours. Toutefois, l’utilisation des adjuvants aux antibiotiques n’a pas amélioré de façon significative les résultats dans l’ensemble, la plupart des patients n’ayant pas besoin d’un changement de prise en charge, quelle que soit l’utilisation d’antibiotiques.
Similar content being viewed by others
References
Prusakowski MK, Kuehl DR. Trends in emergency department management of skin abscesses. Am J Infect Control. 2015;43(4):336–40.
Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18–55.
Borgundvaag B, Ng W, Rowe B, et al. Prevalence of methicillin-resistant Staphylococcus aureus in skin and soft tissue infections in patients presenting to Canadian emergency departments. Can J Emerg Med. 2013;15(3):141–60.
Adam HJ, Allen VG, Currie A, et al. Community-associated methicillin-resistant Staphylococcus aureus: prevalence in skin and soft tissue infections at emergency departments in the Greater Toronto Area and associated risk factors. Can J Emerg Med. 2009;11(5):439–46.
Talan DA, Mower WR, Krishnadasan A, et al. Trimethoprim-sulfamethoxazole versus placebo for uncomplicated skin abscess. N Engl J Med. 2016;374(9):823–32.
Daum RS, Miller LG, Immergluck L, et al. A placebo-controlled trial of antibiotics for smaller skin abscesses. N Engl J Med. 2017;376(26):2545–55.
Vermandere M, Aertgeerts B, Agoritsas T, et al. Antibiotics after incision and drainage for uncomplicated skin abscesses: a clinical practice guideline. BMJ. 2018;6(360): k243.
Wang W, Chen W, Liu Y, et al. Antibiotics for uncomplicated skin abscesses: systematic review and network meta-analysis. BMJ Open. 2018;8(2): e020991.
Talan DA, Moran GJ, Krishnadasan A, et al. Subgroup analysis of antibiotic treatment for skin abscesses. Ann Emerg Med. 2018;71(1):21–30.
Gottlieb M, DeMott JM, Hallock M, et al. Systemic antibiotics for the treatment of skin and soft tissue abscesses: a systematic review and meta-analysis. Ann Emerg Med. 2019;73(1):8–16.
Gilbert EH, Lowenstein SR, Kozoil-McLain J, et al. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;27:305–8.
Worster A, Bledsoe RD, Cleve P, Fernandes CM, Upadhye S, Eva K. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448–51.
Cheng AHY, Campbell S, Chartier LB, Dowling S, Goddard T, Gosselin S, et al. Choosing Wisely Canada’s emergency medicine recommendations: time for a revision. CJEM. 2019;21(6):717–20.
Author information
Authors and Affiliations
Contributions
TI, SLM and BB conceived the study and designed the protocol. TI and CT extracted the data. SLM and BB supervised the conduct of the study and data collection. BB provided clinical advice on study interpretation. TI drafted the manuscript, and all authors contributed substantially to its revision. SLM takes responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Conflict of interest
The authors state no conflict of interest and have received no payment in preparation of this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ibrahim, T., Thompson, C., Borgundvaag, B. et al. Antibiotic prescribing and outcomes for patients with uncomplicated purulent skin and soft tissue infections in the emergency department. Can J Emerg Med 24, 719–724 (2022). https://doi.org/10.1007/s43678-022-00366-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00366-1