Abstract
Objectives
Pain and bleeding complicate 30% of pregnancies, raising concerns for viability. The objective is to evaluate the diagnostic characteristics of a single serum progesterone level in assessing pregnancy viability among symptomatic patients.
Methods
We conducted a predefined literature search in MEDLINE, Embase (OVID), CINAHL and Cochrane databases for studies that enrolled patients in first trimester with miscarriage symptoms, measured progesterone and reported pregnancy viability, from inception to July 2020. We extracted data for 2 × 2 tables, progesterone threshold levels and viability. We obtained summary estimates of sensitivity, specificity, Diagnostic Odds Ratio (DOR), and predictive values at given prevalence rates.
Results
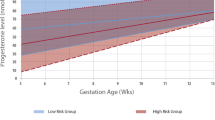
We identified 54 publications. There was a total of 15,878 patients enrolled, of whom 7864 patients (49.5%) were confirmed to have a viable pregnancy and 8014 patients (50.5%) were confirmed to have a non-viable pregnancy. The cut-off value of progesterone ranged from 3.2 to 25 ng/mL (20.034–79.5 nmol/L). We evaluated the performance of the following progesterone cut-off categories: < 6.3, 6.3–12.6, 12.7–19.9, and 20–25 ng/mL. To detect non-viable pregnancy, progesterone with cut-off < 6.3 ng/mL had sensitivity 73.1%, specificity 99.2% and DOR 322.0 (PPV 0.91, 0.97 and 0.99 at prevalences 0.1, 0.25, 0.5, respectively, indicating higher likelihood of non-viable pregnancy), and cut-off category 20–25 ng/mL had sensitivity 91.3%, specificity 75% and DOR 31.4 (NPV 0.99, 0.96 and 0.89 at the prevalences above indicating higher likelihood of viable pregnancy).
Conclusion
A single progesterone level provides a clinically useful prognostic information on pregnancy viability. More than nine out of ten patients with a level < 6.3 ng/mL (< 20.034 nmol/L) will be diagnosed with a non-viable pregnancy, and more than 90% of patients with a level ≥ 20–25 ng/mL (63.6–79.5 nmol/L) will have a viable pregnancy confirmed.
Résumé
Objectives
La douleur et les saignements compliquent 30% des grossesses, ce qui soulève des inquiétudes quant à la viabilité. L’objectif est d’évaluer les caractéristiques diagnostiques d’un seul taux sérique de progestérone dans l’évaluation de la viabilité de la grossesse chez les patientes symptomatiques.
Méthodes
Nous avons effectué une recherche littérature prédéfinie dans les bases de données MEDLINE, Embase (OVID), CINAHL et Cochrane pour des études qui ont recruté des patientes au cours du premier trimestre présentant des symptômes de fausse couche, mesuré la progestérone et signalé la viabilité de la grossesse, du début à juillet 2020. Nous avons extrait les données pour les tableaux 2 × 2, les niveaux de seuil de progestérone et la viabilité. Nous avons obtenu des estimations sommaires de la sensibilité, de la spécificité, du rapport de cotes diagnostiques (DOR) et des valeurs prédictives à des taux de prévalence donnés.
Résultats
On a identifié 54 publications. Il y avait un total de 15 878 patientes recrutées, dont 7864 patientes (49.5%) ont été confirmées comme ayant une grossesse viable et 8014 patientes (50,5%) ont été confirmées comme ayant une grossesse non viable. La valeur seuil de la progestérone variait de 3.2 – 25 ng/mL (20.034 – 79.5 nmol/L). Nous avons évalué les performances des catégories de seuil de progestérone suivantes: < 6.3, 6.3–12.6, 12.7–19.9 et 20–25 ng/mL. Pour détecter une grossesse non viable, la progestérone avec seuil < 6.3 ng/mL avait une sensibilité de 73.1%, une spécificité de 99.2% et une DOR 322.0 (PPV 0.91, 0.97 et 0.99 à des prévalences de 0.1, 0.25, 0.5 respectivement indiquant une probabilité plus élevée de grossesse non viable), et la catégorie de coupure 20–25 ng/mL avait une sensibilité de 91,3%, une spécificité de 75% et une DOR 31,4 (NPV 0.99, 0.96 et 0.89 aux prévalences ci-dessus indiquant une probabilité plus élevée de grossesse viable).
Conclusion
Un seul niveau de progestérone fournit une information pronostique cliniquement utile sur la viabilité de la grossesse. Plus de neuf patientes sur dix avec un niveau < 6.3 ng/mL (< 20.034 nmol/L) sera diagnostiqué de grossesse non viable, et plus de 90% des patientes ayant un niveau ≥ 20–25 ng/mL (63.6–79.5 nmol/L) auront une grossesse viable confirmée.



Similar content being viewed by others
References
Verhaegen J, Gallos ID, van Mello NM, et al. Accuracy of single progesterone test to predict early pregnancy outcome in women with pain or bleeding: meta-analysis of cohort studies. BMJ. 2012;345: e6077.
The Society of Obstetricians and Gynaecologists of Canada (SOGC). Miscarriage. Special Considerations Resources - Your pregnancy. https://www.pregnancyinfo.ca/your-pregnancy/special-consideration/miscarriage/. Accessed 21 Mar 2020.
Ontario Prenatal Education. Prenatal Education. Key Messages for Ontario. Pregnancy and Infant Loss. 2016; https://www.ontarioprenataleducation.ca/infant-loss/#:~:text=Even%20though%20most%20pregnancies%20are%20problem%2Dfree%2C%20it%20is%20estimated,to%20occur%20later%20in%20pregnancy. Accessed 28 July 2021.
Cunningham SD, Magriples U, Thomas JL, et al. Association Between Maternal Comorbidities and Emergency Department Use Among a National Sample of Commercially Insured Pregnant Women. Acad Emerg Med. 2017;24:940–7.
Magriples U, Kershaw TS, Rising SS, Massey Z, Ickovics JR. Prenatal health care beyond the obstetrics service: utilization and predictors of unscheduled care. Am J Obstet Gynecol. 2008;198:75 e71–77.
Varner CE, Park AL, Little D, Ray JG. Emergency department use by pregnant women in Ontario: a retrospective population-based cohort study. CMAJ Open. 2020;8:E304–12.
Varner C, Balaban D, McLeod S, Carver S, Borgundvaag B. Fetal outcomes following emergency department point-of-care ultrasound for vaginal bleeding in early pregnancy. Can Fam Physician. 2016;62:572–8.
Deng Y, Chen C, Chen S, et al. Baseline levels of serum progesterone and the first trimester pregnancy outcome in women with threatened abortion: a retrospective cohort study. Biomed Res Int. 2020;2020:8780253.
Peng S, Micks T, Braganza D, et al. Canadian national survey of family medicine residents on point-of-care ultrasound training. Can Fam Physician. 2019;65:e523–30.
Whittaker PG, Schreiber CA, Sammel MD. Gestational hormone trajectories and early pregnancy failure: a reassessment. Reprod Biol Endocrinol: RB&E. 2018;16:95.
Jurkovic D, Overton C, Bender-Atik R. Diagnosis and management of first trimester miscarriage. BMJ. 2013;346:f3676.
Kadam VK, Agrawal S, Saxena P, Laul P. Predictive value of single serum progesterone level for viability in threatened miscarriage. J Obstet Gynaecol India. 2019;69:431–5.
Phipps MG, Hogan JW, Peipert JF, Lambert-Messerlian GM, Canick JA, Seifer DB. Progesterone, inhibin, and hCG multiple marker strategy to differentiate viable from nonviable pregnancies. Obstet Gynecol. 2000;95:227–31.
Pillai RN, Konje JC, Richardson M, Tincello DG, Potdar N. Prediction of miscarriage in women with viable intrauterine pregnancy-A systematic review and diagnostic accuracy meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2018;220:122–31.
Pillai RN, Konje JC, Tincello DG, Potdar N. Role of serum biomarkers in the prediction of outcome in women with threatened miscarriage: a systematic review and diagnostic accuracy meta-analysis. Hum Reprod Update. 2016;22:228–39.
Li Y, Zhang J, Zhang K, Wang E, Shu J. Significance of dynamically monitoring serum estrogen and beta-human chorionic gonadotropin in early pregnancy assessment. J Clin Lab Anal. 2021;35:e23559.
Diagnosis and Management of Ectopic Pregnancy: Green-top Guideline No. 21. BJOG. 2016;123:e15–55.
Hendriks E, MacNaughton H, MacKenzie MC. First trimester bleeding: evaluation and management. Am Fam Physician. 2019;99:166–74.
Morin L, Cargill YM, Glanc P. Ultrasound evaluation of first trimester complications of pregnancy. J Obstet Gynaecol Can. 2016;38:982–8.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Deeks JJ, Bossuyt PM, Gatsonis CA. Cochrane handbook for systematic reviews of diagnostic test accuracyVersion 1.0. The Cochrane Collabortaion, 2010. Available from: http://srdta.cochrane.org/. Accessed 6 July 2020.
Lautmann K, Cordina M, Elson J, Johns J, Schramm-Gajraj K, Ross JA. Clinical use of a model to predict the viability of early intrauterine pregnancies when no embryo is visible on ultrasound. Hum Reprod. 2011;26:2957–63.
Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
Schunemann HJ, Oxman AD, Brozek J, et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ. 2008;336:1106–10.
GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime, 2021. Available from gradepro.org.
Rutter CM, Gatsonis CA. A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med. 2001;20:2865–84.
Takwoingi Y, Deeks JJ. MetaDAS: a SAS macro for meta-analysis of diagnostic accuracy studies. Version 1.3. 2010. Available from https://methods.cochrane.org/sites/methods.cochrane.org.sdt/files/uploads/MetaDAS%20Quick%20Reference%20v1.3%20May%202012.pdf.
Elewa A, Mansour A, El-Deen A, Bioumi A. The role of a single serum progesterone measurement in relation to early pregnancy failure and fetal viability. Med J Cairo Univ. 2016;84:169–75.
Matthews CP, Coulson PB, Wild RA. Serum progesterone levels as an aid in the diagnosis of ectopic pregnancy. Obstet Gynecol. 1986;68:390–4.
Sauer MV, Sinosich MJ, Yeko TR, Vermesh M, Buster JE, Simon JA. Predictive value of a single serum pregnancy associated plasma protein-A or progesterone in the diagnosis of abnormal pregnancy. Hum Reprod. 1989;4:331–4.
Riss PA, Radivojevic K, Bieglmayer C. Serum progesterone and human chorionic gonadotropin in very early pregnancy: implications for clinical management. Eur J Obstet Gynecol Reprod Biol. 1989;32:71–7.
Witt BR, Wolf GC, Wainwright CJ, Johnston PD, Thorneycroft IH. Relaxin, CA-125, progesterone, estradiol, Schwangerschaft protein, and human chorionic gonadotropin as predictors of outcome in threatened and nonthreatened pregnancies. Fertil Steril. 1990;53:1029–36.
Hahlin M, Sjöblom P, Lindblom B. Combined use of progesterone and human chorionic gonadotropin determinations for differential diagnosis of very early pregnancy. Fertil Steril. 1991;55:492–6.
Takahashi K, Yamane Y, Kitao M. Prognostic value of serum CA 125 and serum progesterone in threatened abortion. J Obstet Gynaecol. 1992;12:147–9.
Peterson CM, Kreger D, Delgado P, Hung TT. Laboratory and clinical comparison of a rapid versus a classic progesterone radioimmunoassay for use in determining abnormal and ectopic pregnancies. Am J Obstet Gynecol. 1992;166:562–6.
Ledger WL, Sweeting VM, Chatterjee S. Rapid diagnosis of early ectopic pregnancy in an emergency gynaecology service–are measurements of progesterone, intact and free beta human chorionic gonadotrophin helpful? Hum Reprod. 1994;9:157–60.
Valley VT, Mateer JR, Aiman EJ, Thoma ME, Phelan MB. Serum progesterone and endovaginal sonography by emergency physicians in the evaluation of ectopic pregnancy. Acad Emerg Med. 1998;5:309–13.
Dart R, Dart L, Segal M, Page C, Brancato J. The ability of a single serum progesterone value to identify abnormal pregnancies in patients with beta-human chorionic gonadotropin values less than 1,000 mIU/mL. Acad Emerg Med. 1998;5:304–9.
Banerjee S, Aslam N, Zosmer N, Woelfer B, Jurkovic D. The expectant management of women with early pregnancy of unknown location. Ultrasound Obstet Gynecol. 1999;14:231–6.
Buckley RG, King KJ, Disney JD, Riffenburgh RH, Gorman JD, Klausen JH. Serum progesterone testing to predict ectopic pregnancy in symptomatic first-trimester patients. Ann Emerg Med. 2000;36:95–100.
Dart R, Ramanujam P, Dart L. Progesterone as a predictor of ectopic pregnancy when the ultrasound is indeterminate. Am J Emerg Med. 2002;20:575–9.
Elson J, Salim R, Tailor A, Banerjee S, Zosmer N, Jurkovic D. Prediction of early pregnancy viability in the absence of an ultrasonically detectable embryo. Ultrasound Obstet Gynecol. 2003;21:57–61.
Camejo MI, Proverbio F, Febres F, Casart YC. Bioactive to immunoreactive ratio of circulating human chorionic gonadotropin as possible evaluation for the prognosis of threatened abortion. Eur J Obstet Gynecol Reprod Biol. 2003;109:181–4.
Florio P, Severi FM, Bocchi C, et al. Single serum activin a testing to predict ectopic pregnancy. J Clin Endocrinol Metab. 2007;92:1748–53.
Ugurlu EN, Ozaksit G, Karaer A, Zulfikaroglu E, Atalay A, Ugur M. The value of vascular endothelial growth factor, pregnancy-associated plasma protein-A, and progesterone for early differentiation of ectopic pregnancies, normal intrauterine pregnancies, and spontaneous miscarriages. Fertil Steril. 2009;91:1657–61.
Day A, Sawyer E, Mavrelos D, Tailor A, Helmy S, Jurkovic D. Use of serum progesterone measurements to reduce need for follow-up in women with pregnancies of unknown location. Ultrasound Obstet Gynecol. 2009;33:704–10.
Altay MM, Yaz H, Haberal A. The assessment of the gestational sac diameter, crown-rump length, progesterone and fetal heart rate measurements at the 10th gestational week to predict the spontaneous abortion risk. J Obstet Gynaecol Res. 2009;35:287–92.
Osmanağaoğlu MA, Erdoğan I, Eminağaoğlu S, et al. The diagnostic value of beta-human chorionic gonadotropin, progesterone, CA125 in the prediction of abortions. J Obstet Gynaecol. 2010;30:288–93.
Bignardi T, Condous G, Kirk E, et al. Viability of intrauterine pregnancy in women with pregnancy of unknown location: prediction using human chorionic gonadotropin ratio vs. progesterone. Ultrasound Obstet Gynecol. 2010;35:656–661.
Rausch ME, Sammel MD, Takacs P, Chung K, Shaunik A, Barnhart KT. Development of a multiple marker test for ectopic pregnancy. Obstet Gynecol. 2011;117:573–82.
Majeed H, Højgaard A, Johannesen P, Ladefoged ML, Forman A, Bor P. Predictive value of serum human chorionic gonadotropin ratio, progesterone and inhibin A for expectant management of early pregnancies of unknown location. Eur J Obstet Gynecol Reprod Biol. 2012;165:66–9.
Abdul-Hussein MM, Abdul-Rasheed OF, Al-Moayed HA. The Values of CA-125, Progesterone, ß-HCG and Estradiol in the Early Prediction of Ectopic Pregnancy. Oman Med J. 2012;27:124–8.
Abdelazim IA, Elezz AA, Elsherbiny M. Relation between single serum progesterone assay and viability of the first trimester pregnancy. Springerplus. 2012;1:80.
Maged A, W. AM. Biochemical and ultrasonographic predictors of outcome in threatened abortion. Middle East Fertil Soc J. 2013;18:177–181.
Butler SA, Abban TK, Borrelli PT, Luttoo JM, Kemp B, Iles RK. Single point biochemical measurement algorithm for early diagnosis of ectopic pregnancy. Clin Biochem. 2013;46:1257–63.
Kant R, Ara S, Lone A, Gupta S. Evaluation of outcome of pregnancy in threatened abortion by serum progesterone levels. Int J Reprod Contracept Obstet Gynecol. 2015;4:1313–8.
Lek SM, Ku CW, Allen JC, et al. Validation of serum progesterone <35nmol/L as a predictor of miscarriage among women with threatened miscarriage. BMC Pregnancy Childbirth. 2017;17:78.
Puget C, Joueidi Y, Bauville E, et al. Serial hCG and progesterone levels to predict early pregnancy outcomes in pregnancies of uncertain viability: A prospective study. Eur J Obstet Gynecol Reprod Biol. 2018;220:100–5.
Dave A, Patil R, Bansal P, Malhotra A. Role of serum progesterone in threatened miscarriage. Int J Reprod Contracept Obstet Gynecol. 2018;7:4272–8.
Bucuri CE, Ciortea R, Malutan AM, Berceanu C, Rada MP, Mihu D. Progesterone’s Serum Level and a New Ultrasonographic Parameter in the First Trimester Pregnancy - Prognostic Factors for Embryonic Demise. Rev Bras Ginecol Obstet. 2019;41:525–30.
Refaat B, Bahathiq AO. The performances of serum activins and follistatin in the diagnosis of ectopic pregnancy: A prospective case-control study. Clin Chim Acta. 2020;500:69–74.
Lautmann K, Cordina M, Elson J, Johns J, Schramm-Gajraj K, Ross JA. Clinical use of a model to predict the viability of early intrauterine pregnancies when no embryo is visible on ultrasound. Hum Reprod. 2011;26:2957–63.
Perkins SL, Al-Ramahi M, Claman P. Comparison of serum progesterone as an indicator of pregnancy nonviability in spontaneously pregnant emergency room and infertility clinic patient populations. Fertil Steril. 2000;73:499–504.
McCord ML, Muram D, Buster JE, Arheart KL, Stovall TG, Carson SA. Single serum progesterone as a screen for ectopic pregnancy: exchanging specificity and sensitivity to obtain optimal test performance. Fertil Steril. 1996;66:513–6.
O’Leary P, Nichols C, Feddema P, Lam T, Aitken M. Serum progesterone and human chorionic gonadotrophin measurements in the evaluation of ectopic pregnancy. Aust N Z J Obstet Gynaecol. 1996;36:319–23.
Isaacs JD, Whitworth NS, Cowan BD. Relative operating characteristic analysis in reproductive medicine: comparison of progesterone and human chorionic gonadotropin doubling time as predictors of early gestational normalcy. Fertil Steril. 1994;62:452–5.
Grosskinsky CM, Hage ML, Tyrey L, Christakos AC, Hughes CL. hCG, progesterone, alpha-fetoprotein, and estradiol in the identification of ectopic pregnancy. Obstet Gynecol. 1993;81:705–9.
Choe JK, Check JH, Nowroozi K, Benveniste R, Barnea ER. Serum progesterone and 17-hydroxyprogesterone in the diagnosis of ectopic pregnancies and the value of progesterone replacement in intrauterine pregnancies when serum progesterone levels are low. Gynecol Obstet Invest. 1992;34:133–8.
Williams RS, Gaines IL, Fossum GT. Progesterone in diagnosis of ectopic pregnancy. J Fla Med Assoc. 1992;79:237–9.
Gelder MS, Boots LR, Younger JB. Use of a single random serum progesterone value as a diagnostic aid for ectopic pregnancy. Fertil Steril. 1991;55:497–500.
Kratzer PG, Taylor RN. Corpus luteum function in early pregnancies is primarily determined by the rate of change of human chorionic gonadotropin levels. Am J Obstet Gynecol. 1990;163:1497–502.
Hubinont CJ, Thomas C, Schwers JF. Luteal function in ectopic pregnancy. Am J Obstet Gynecol. 1987;156:669–74.
Yeko TR, Gorrill MJ, Hughes LH, Rodi IA, Buster JE, Sauer MV. Timely diagnosis of early ectopic pregnancy using a single blood progesterone measurement. Fertil Steril. 1987;48:1048–50.
Al Mohamady M, Fattah GA, Elkattan E, Bayoumy R, Hamed DA. Correlation of serum CA-125 and progesterone levels with ultrasound markers in the prediction of pregnancy outcome in threatened miscarriage. Int J Fertil Steril. 2016;9:506–11.
Senapati S, Sammel MD, Butts SF, Takacs P, Chung K, Barnhart KT. Predicting first trimester pregnancy outcome: derivation of a multiple marker test. Fertil Steril. 2016;106:1725–32.
Yalcin I, Taskin S, Pabuccu EG, Soylemez F. The value of placental protein 13, beta-human chorionic gonadotropin and progesterone in the prediction of miscarriages in threatened miscarriage patients. J Obstet Gynaecol. 2015;35:283–6.
Hanita O, Hanisah AH. Potential use of single measurement of serum progesterone in detecting early pregnancy failure. Malays J Pathol. 2012;34:41–6.
Stovall TG, Kellerman AL, Ling FW, Buster JE. Emergency department diagnosis of ectopic pregnancy. Ann Emerg Med. 1990;19:1098–103.
Rojas-Luengas V, Seaton B, Dainty K, McLeod S, Varner C. The emergency department experience of patients with early pregnancy complications: A qualitative study. CJEM. 2019;21:798–802.
NICE. Ectopic pregnancy and miscarriage: diagnosis and initial management. 2019; https://www.nice.org.uk/guidance/ng126/chapter/Recommendations#diagnosis-of-viable-intrauterine-pregnancy-and-of-tubal-ectopic-pregnancy. Accessed 20 July 2020.
Hinshaw K, Fayyad D, Munjurluri P. The management of early pregnancy loss. Revised Guideline no. 25. Green-top Guideline no. 25, Guidelines and Audit Committee of the Royal College of Obstetricians and Gynaecologists. 2006;25:1–18.
Acknowledgements
We thank Mrs. Preeti Gupta for input with clinical guidelines.
Funding
None.
Author information
Authors and Affiliations
Contributions
BG and WC contributed equally to the systematic review and are joint first authors. VT, BG, and WC were the core team leading the systematic review. BG, SA, and KA identified and selected the studies. BG, WC, SA, KA, NC and AZ collected the data. VT and WC analyzed the data. BG, WC and VT drafted the manuscript. All authors approved the final version of the manuscript. VT is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Study registration
PROSPERO 2020 CRD42020186508.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ghaedi, B., Cheng, W., Ameri, S. et al. Performance of single serum progesterone in the evaluation of symptomatic first-trimester pregnant patients: a systematic review and meta-analysis. Can J Emerg Med 24, 611–621 (2022). https://doi.org/10.1007/s43678-022-00332-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00332-x