Abstract
Objective
In emergency department patients with ureteral colic, the prognostic value of hydronephrosis is unclear. Our goal was to determine whether hydronephrosis can differentiate low-risk patients appropriate for trial of spontaneous passage from those with clinically important stones likely to experience passage failure.
Methods
We used administrative data and structured chart review to evaluate a consecutive cohort of patients with ureteral stones who had a CT at nine Canadian hospitals in two cities. We used CT, the gold standard for stone imaging, to assess hydronephrosis and stone size. We described classification accuracy of hydronephrosis severity for detecting large (≥ 5 mm) stones. In patients attempting spontaneous passage we used hierarchical Bayesian regression to determine the association of hydronephrosis with passage failure, defined by the need for rescue intervention within 60 days. To illustrate prognostic utility, we reported pre-test probability of passage failure among all eligible patients (without hydronephrosis guidance) to post-test probability of passage failure in each hydronephrosis group.
Results
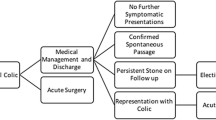
Of 3251 patients, 70% male and mean age 51, 38% had a large stone, including 23%, 29%, 53% and 72% with absent, mild, moderate and severe hydronephrosis. Passage failure rates were 15%, 20%, 28% and 43% in the respective hydronephrosis categories, and 23% overall. “Absent or mild” hydronephrosis identified a large subset of patients (64%) with low passage failure rates. Moderate hydronephrosis predicted slightly higher, and severe hydronephrosis substantially higher passage failure risk.
Conclusions
Absent and mild hydronephrosis identify low-risk patients unlikely to experience passage failure, who may be appropriate for trial of spontaneous passage without CT imaging. Moderate hydronephrosis is weakly associated with larger stones but not with significantly greater passage failure. Severe hydronephrosis is an important finding that warrants definitive imaging and referral. Differentiating “moderate-severe” from “absent-mild” hydronephrosis provides risk stratification value. More granular hydronephrosis grading is not prognostically helpful.
Résumé
Objectif
Chez les patients des services d’urgence (SU) atteints de colique urétérale, la valeur pronostique de l’hydronéphrose n’est pas claire. Notre objectif était de déterminer si l’hydronéphrose peut différencier les patients à faible risque appropriés pour l’essai de passage spontané de ceux qui ont des calculs cliniquement importants susceptibles de subir un échec de passage.
Méthodes
Nous avons utilisé des données administratives et un examen structuré des dossiers pour évaluer une cohorte consécutive de patients atteints de calculs urétéraux qui avaient subi une tomodensitométrie dans neuf hôpitaux canadiens de deux villes. Nous avons utilisé la tomodensitométrie, l’étalon-or pour l’imagerie des calculs, pour évaluer l’hydronéphrose et la taille des calculs. Nous avons décrit la précision de la classification de la gravité de l’hydronéphrose pour la détection de gros calculs (> 5 mm). Chez les patients tentant un passage spontané, nous avons utilisé la régression bayésienne hiérarchique pour déterminer l’association de l’hydronéphrose avec l’échec du passage, défini par le besoin d’intervention de sauvetage dans les 60 jours. Pour illustrer l’utilité pronostique, nous avons signalé la probabilité d’échec de passage avant le test chez tous les patients admissibles (sans directives sur l’hydronéphrose) à la probabilité d’échec de passage post-test dans chaque groupe d’hydronéphrose.
Résultats
Sur 3251 patients, 70% d’hommes et d’âge moyen 51 ans, 38% avaient un gros calcul, dont 23%, 29%, 53% et 72% avec une hydronéphrose absente, légère, modérée et sévère. Les taux d’échec au passage étaient de 15%, 20%, 28% et 43% dans les catégories d’hydronéphrose respectives et de 23% dans l’ensemble. L’hydronéphrose « absente ou légère » a permis d’identifier un sous-ensemble important de patients (64%) présentant de faibles taux d’échec au passage. Une hydronéphrose modérée prédisait un risque d’échec de passage légèrement plus élevé, et une hydronéphrose sévère un risque sensiblement plus élevé.
Conclusions
L’absence d’hydronéphrose et une hydronéphrose légère permettent d’identifier les patients à faible risque, peu susceptibles d’avoir un échec de passage, qui peuvent être appropriés pour un essai de passage spontané sans imagerie CT. Une hydronéphrose modérée est faiblement associée à des calculs plus gros mais pas à un échec de passage significativement plus important. L’hydronéphrose sévère est une constatation importante qui justifie une imagerie définitive et une référence. Différencier l’hydronéphrose « modérée-sévère » de l’« absence-légère » fournit une valeur de stratification du risque. Un classement plus granulaire de l’hydronéphrose n’est pas utile sur le plan pronostique.



Similar content being viewed by others
References
Daniels B, Gross CP, Molinaro A, et al. STONE PLUS: evaluation of emergency department patients with suspected renal colic using a clinical prediction tool combined with point-of-care limited ultrasonography. Ann Emerg Med. 2016;67:439–48.
Ray AA, Ghiculete D, Pace KT, Honey RJD. Limitations to ultrasound in the detection and measurement of urinary tract calculi. Urology. 2010;76:295–300.
Yilmaz S, Sindel T, Arslan G, et al. Renal colic: comparison of spiral CT, US and IVU in the detection of ureteral calculi. Eur Radiol. 1998;8:212–7.
Fowler KA, Locken JA, Duchesne JH, Williamson MR. Ultrasound for detecting renal calculi with nonenhanced CT as a reference standard. Radiology. 2002;222:109–13.
Wong C, Teitge B, Ross M, et al. The accuracy and prognostic value of point-of-care ultrasound for nephrolithiasis in the emergency department: a systematic review and meta-analysis. Acad Emerg Med. 2018;25:684–98.
Innes GD, Scheuermeyer FX, McRae AD, et al. Which patients should have early surgical intervention for acute ureteric colic. J Urol. 2021;205:152–8.
Hollingsworth JM, Canales BK, Rogers M, et al. Alpha blockers for treatment of ureteric stones: systematic review and meta-analysis. BMJ. 2016;355:i6112.
National Institute for Health and Care Excellence. Renal and ureteric stones: assessment and management. In: Imaging for diagnosis. Diagnostic evidence review. London: National Institute for Health and Care Excellence; 2019.
Schoenfeld EM, Pekow PS, Shieh MS, et al. The diagnosis and management of patients with renal colic across a sample of US hospitals: high CT utilization despite low rates of admission and inpatient urologic intervention. PLoS ONE. 2017;12:e0169160.
Moak JH, Lyons MS, Lindsell CJ. Bedside renal ultrasound in the evaluation of suspected ureterolithiasis. Am J Emerg Med. 2012;30:218–21.
Goertz JK, Lotterman S. Can the degree of hydronephrosis on ultrasound predict kidney stone size? Am J Emerg Med. 2010;28:813–6.
Taylor M, Woo MY, Pageau P, et al. Ultrasonography for the prediction of urological surgical intervention in patients with renal colic. Emerg Med J. 2016;33:118–23.
Fields J, Fischer J, Anderson K, et al. The ability of renal ultrasound and ureteral jet evaluation to predict 30-day outcomes in patients with suspected nephrolithiasis. Am J Emerg Med. 2015;33:1402–6.
Leo M, Langlois BK, Pare J, et al. Ultrasound vs computed tomography for severity of hydronephrosis and its Importance in renal colic. West J Emerg Med. 2017;18:559–68.
Daniels B, Schoenfeld E, Taylor A. Predictors of hospital admission and urologic intervention in adult emergency department patients with CT-confirmed ureteral stones. J Urol. 2017;198:1359–66.
Innes G, McRae A, Grafstein E, et al. Variability of renal colic management and outcomes in two Canadian cities. Can J Emerg Med. 2018;20:702–12.
Ordon M, Urbach D, Mamdani M, et al. The surgical management of kidney stone disease: a population based time series analysis. J Urol. 2014;192:1450–6.
McGlothlin AE, Viele K. Bayesian hierarchical models. JAMA. 2018;320:2365–6.
Riddell J, Case A, Wopat R, et al. Sensitivity of emergency department ultrasound to detect hydronephrosis in patients with CTR-proven stones. West J Emerg Med. 2014;15:96–100.
Herbst MK, Rosenberg G, Daniels B, et al. Effect of provider experience on clinician-performed ultrasonography for hydronephrosis in patients with suspected renal colic. Ann Emerg Med. 2014;64:269–76.
Pathan SA, Mitra B, Mirza S, et al. Emergency physician interpretation of point-of-care ultrasound for identifying and grading of hydronephrosis in renal colic compared with consensus interpretation by emergency radiologists. Acad Emerg Med. 2018;25:1129–37.
Watkins S, Bowra J, Sharma P, et al. Validation of emergency physician ultrasound in diagnosing hydronephrosis in ureteric colic. Emerg Med Australas. 2007;19(3):188–95.
Gaspari RJ, Horst K. Emergency ultrasound and urinalysis in the evaluation of flank pain. Acad Emerg Med. 2005;12:1180–4.
Schoenfeld EM, Shieh MS, Pekow P, et al. Association of patient and visit characteristics with rate and timing of urologic procedures for patients discharged from the emergency department with renal colic. JAMA Netw Open. 2019;2(12):e1916454.
Funding
This study was funded by the MSI Foundation (a registered charity and research funding agency under the arms-length oversight of the Alberta College of Physicians and Surgeons).
Author information
Authors and Affiliations
Contributions
GDI conceived and designed the study, acquired research funding, and drafted the manuscript. FXS performed the literature search, participated in study design, and assisted with manuscript revisions. ADM helped guide development of the design and analysis, and assisted with manuscript revision. JMHT was Vancouver Urology study site liaison and contributed to manuscript revisions. DJL designed and performed the statistical analyses, and helped revise the draft manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Teichman has received grants and personal fees from from Boston Scientific, grants from Cook Urologic, personal fees from Urigen and non-financial support from Innova Quartz, although none were related to this research. None of the other investigators have any potential conflicts to report.
Additional information
Meetings
This study has not been previously presented.
Rights and permissions
About this article
Cite this article
Innes, G.D., Scheuermeyer, F.X., McRae, A.D. et al. Hydronephrosis severity clarifies prognosis and guides management for emergency department patients with acute ureteral colic. Can J Emerg Med 23, 687–695 (2021). https://doi.org/10.1007/s43678-021-00168-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-021-00168-x