Abstract
Background
While electrolyte maintenance solution is recommended and commonly used in pediatric gastroenteritis, it can be more costly and less palatable than preferred fluids such as apple juice.
Objective
To assess the incremental cost-effectiveness of apple juice/preferred fluids versus electrolyte maintenance solution in reducing treatment failures in children in an emergency department from societal and health care perspectives.
Methods
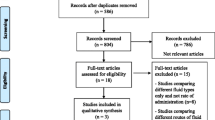
A probabilistic cost-effectiveness analysis was performed using clinical trial and chart data. All intervention, and direct and indirect costs were included, with a 14-day time horizon. Cost-effectiveness was examined by calculating the difference in mean number of treatment failures and mean cost/patient between treatment groups. The probabilistic point estimate and 95% confidence intervals for incremental costs and incremental effectiveness were determined.
Results
The apple juice strategy was less costly than electrolytes with average per child savings of CAD $171 (95% CI $22 to $1097) from a societal perspective, and $147 (95% CI $23 to $1056) from a health care perspective. There were 0.08 fewer treatment failures per child (95% CI − 0.15 to − 0.02). The higher electrolyte maintenance solution cost was due to more frequent hospitalizations, ongoing care, and greater lost parental productivity due to additional medical visits.
Conclusion
Apple juice/preferred fluids strategy was dominant over electrolytes in the treatment of children with minimal dehydration secondary to acute gastroenteritis as this option yielded fewer treatment failures and a lower societal cost. Given the high prevalence of acute gastroenteritis, this approach may result in significant cost savings while leading to improved clinical outcomes.
Résumé
Contexte
Bien que la solution de maintien des électrolytes soit recommandée et couramment utilisée dans les gastro-entérites pédiatriques, elle peut être plus coûteuse et moins agréable au goût que les liquides préférés tels que le jus de pomme.
Objectif
Évaluer le rapport coût-efficacité supplémentaire du jus de pomme/des liquides préférés par rapport à des électrolytes pour réduire les échecs de traitement chez les enfants dans un service d'urgence, du point de vue de la société et des soins de santé.
Les méthodes
Une analyse probabiliste de la rentabilité a été réalisée en utilisant les données des essais cliniques et des dossiers. Tous les coûts d'intervention, directs et indirects, ont été inclus, avec un horizon temporel de 14 jours. La rentabilité a été examinée en calculant la différence du nombre moyen d'échecs de traitement et du coût/patient moyen entre les groupes de traitement. L'estimation ponctuelle probabiliste et les intervalles de confiance à 95% pour les coûts différentiels et l'efficacité différentielle ont été déterminés.
Résultats
La stratégie du jus de pomme était moins coûteuse que les électrolytes, avec des économies moyennes par enfant de 171 $ CAD (IC à 95 % : 22 $ à 1097 $) du point de vue sociétal et de 147 $ (IC à 95 % : 23 $ à 1056 $) du point de vue des soins de santé. Il y a eu 0,08 échec de traitement en moins par enfant (IC 95 % : -0,15 à -0,02). Le coût plus élevé des électrolytes est dû à des hospitalisations plus fréquentes, à des soins continus et à une plus grande perte de productivité des parents en raison de visites médicales supplémentaires.
Conclusion
La stratégie du jus de pomme/des liquides préférés a été dominante sur les électrolytes dans le traitement des enfants présentant une déshydratation minimale secondaire à une gastro-entérite aiguë, car cette option a permis de réduire les échecs du traitement et le coût pour la société. Compte tenu de la prévalence élevée de la gastro-entérite aiguë, cette approche peut entraîner des économies de coûts significatives tout en améliorant les résultats cliniques.

Similar content being viewed by others
References
Hartman S, Brown E, Loomis E, Russell HA. Gastroenteritis in children. Am Fam Phys. 2019;99(3):159–65.
King CK, Glass R, Bresee JS, Duggan C, Prevention. CfDCa. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR Recomm Rep. 2003;52(RR-16):1–16.
Lucado J, Mohamoud S, Zhao L, Elixhauser A. Infectious enteritis and foodborne illness in the United States, 2010. HCUP Statistical Brief #150. Rockville, MD: Agency for Healthcare Research and Quality; 2013.
Freedman SB, Cho D, Boutis K, Stephens D, Schuh S. Assessing the palatability of oral rehydration solutions in school-aged children: a randomized crossover trial. Arch Pediatr Adolesc Med. 2010;164(8):696–702.
Reis EC, Goepp JG, Katz S, Santosham M. Barriers to use of oral rehydration therapy. Pediatrics. 1994;93(5):708–11.
Karpas A, Finkelstein M, Reid S. Parental preference for rehydration method for children in the emergency department. Pediatr Emerg Care. 2009;25(5):301–6.
Freedman SB, Willan AR, Boutis K, Schuh S. Effect of dilute apple juice and preferred fluids vs electrolyte maintenance solution on treatment failure among children with mild gastroenteritis: a randomized clinical trial. JAMA. 2016;315(18):1966–74.
Cohen MB, Hardin J. Medicaid coverage of oral rehydration solutions. N Engl J Med. 1993;329(3):211.
Canadian Agency for Drugs and Technologies in Health. Guidelines for the economic evaluation of health technologies, 4th edn. Ottawa: Canadian Agency for Drugs and Technologies in Health=Agence canadienne des médicaments et des technologies de la santé; 2017.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. 4th ed. Oxford: Oxford University Press; 2015.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in Health and Medicine. JAMA. 2016;316(10):1093–103.
Ungar WJ. Economic evaluation in child health. Oxford: Oxford University Press; 2010. p. 2010.
Friedman JN, Goldman RD, Srivastava R, Parkin PC. Development of a clinical dehydration scale for use in children between 1 and 36 months of age. J Pediatr. 2004;145(2):201–7.
Freedman SB, Thakkar VA. Easing the strain on a pediatric tertiary care center: use of a redistribution system. Arch Pediatr Adolesc Med. 2007;161(9):870–6.
Ontario Case Costing Initiative. 2019. https://hsimi.ca/occp/occpreports/. Accessed Jun 2019.
Ontario Ministry of Health and Long-Term Care. Schedule of Benefits-Physician Services Under the Health Insurance Act. 2016.
Statistics Canada. Table: 14-10-0065-01 Employee wages by job permanency and union coverage, monthly, unadjusted for seasonality. 2019. https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=1410006501. Accessed Jun 2019.
Majowicz SE, McNab WB, Sockett P, Henson TS, Dore K, Edge VL, et al. Burden and cost of gastroenteritis in a Canadian community. J Food Prot. 2006;69(3):651–9.
Freedman SB, Hall M, Shah SS, Kharbanda AB, Aronson PL, Florin TA, et al. Impact of increasing ondansetron use on clinical outcomes in children with gastroenteritis. JAMA Pediatr. 2014;168(4):321–9.
Guarino A, Ashkenazi S, Gendrel D, Lo Vecchio A, Shamir R, Szajewska H, et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: update 2014. J Pediatr Gastroenterol Nutr. 2014;59(1):132–52.
Rao SS, Summers RW, Rao GR, Ramana S, Devi U, Zimmerman B, et al. Oral rehydration for viral gastroenteritis in adults: a randomized, controlled trial of 3 solutions. JPEN J Parenter Enteral Nutr. 2006;30(5):433–9.
Valois S, Costa-Ribeiro H Jr, Mattos A, Ribeiro TC, Mendes CM, Lifshitz F. Controlled, double-blind, randomized clinical trial to evaluate the impact of fruit juice consumption on the evolution of infants with acute diarrhea. Nutr J. 2005;4:23.
Baker JM, Dahl RM, Cubilo J, Parashar UD, Lopman BA. Effects of the rotavirus vaccine program across age groups in the United States: analysis of national claims data, 2001–2016. BMC Infect Dis. 2019;19(1):186.
Cummings EA, Reid GJ, Finley GA, McGrath PJ, Ritchie JA. Prevalence and source of pain in pediatric inpatients. Pain. 1996;68(1):25–31.
Skippen P, Adderley R, Bennett M, Cogswell A, Froese N, Seear M, et al. Iatrogenic hyponatremia in hospitalized children: can it be avoided? Paediatr Child Health. 2008;13(6):502–6.
Freedman SB, Steiner MJ, Chan KJ. Oral ondansetron administration in emergency departments to children with gastroenteritis: an economic analysis. PLoS Med. 2010;7(10):1000350.
Levinson W, Huynh T. Engaging physicians and patients in conversations about unnecessary tests and procedures: choosing Wisely Canada. CMAJ. 2014;186(5):325–6.
Ontario Ministry of Health. Ontario drug benefit formulary/comparative drug index—edition 43. Ministry of Health and Long-Term Care; 2019.
Funding
Dr. Moretti is supported in part by the Canadian Institute for Health Research, Support for Patient Oriented Research, and the Ontario Child Health Support Unit, an Ontario SPOR Support Unit. Dr. Ungar holds the Canada Research Chair in Economic Evaluation and Technology Assessment in Child Health. Dr. Freedman is supported in part by Alberta Children’s Hospital Foundation Professorship in Child Health and Wellness. The original clinical trial was supported by a grant from Physicians Services Incorporated Foundation (grant 10q1011). The authors have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Moretti, M.E., Ungar, W.J., Freedman, S.B. et al. Cost-effectiveness of preferred fluids versus electrolytes in pediatric gastroenteritis. Can J Emerg Med 23, 646–654 (2021). https://doi.org/10.1007/s43678-021-00108-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-021-00108-9