Abstract
Background
Posterolateral fusion (PLF) surgery is frequently performed for a range of spinal disorders. However, spontaneous lumbar interbody fusion (SLIF) following PLF surgery is yet to be reported. Thus, we evaluated the incidence and characteristics of SLIF among patients that underwent PLF surgery.
Methods
This retrospective study involved review of electronic medical records of 121 adult patients who underwent primary lumbar decompression with instrumented PLF between 2006 and 2011. The available radiographs of L2–S1 region were assessed for SLIF and PLF. At 1 year, modified Lee’s and Lenke’s criteria were used to assess SLIF and PLF, respectively. Differences between the patients in the fusion and non-fusion groups were evaluated.
Results
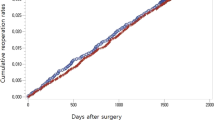
At 1-year follow-up, 28.93 and 87.61% patients had SLIF and PLF, respectively. Moreover, 27.27% patients had both SLIF and PLF. L4–L5 (n = 13) was the most common segment involved in SLIF. SLIF rate was significantly greater among young adults (p value = 0.001), and those with no pre-operative instability (p value = 0.003) as well as who underwent pedicular fixation instrumented PLF surgery (p value < 0.0001). While, PLF was significantly greater in patients who did not undergo discectomy (p value = 0.049). SLIF was not significantly associated with sex, age groups, discectomy status, and level of PLF surgery (all p values > 0.05). PLF was not significantly associated with sex, age groups, pre-operative instability, type of instrumentation, and level of PLF surgery (all p values > 0.05). There was no significant association between patients with SLIF and PLF (p value = 0.155).
Conclusions
More than a quarter of patients developed SLIF and majority of them had PLF. SLIF was significantly associated with younger age at surgery and use of pedicular fixation instruments.
Level of Evidence III; retrospective cohort study.

Similar content being viewed by others
Data availability
Data cannot be shared openly but are available on reasonable request from the corresponding author.
References
Raizman, N. M., O’Brien, J. R., Poehling-Monaghan, K. L., & Yu, W. D. (2009). Pseudarthrosis of the spine. Journal of American Academy of Orthopaedic Surgeons, 17(8), 494–503.
Tuli, S. M. (2013). Historical aspects of Pott’s disease (spinal tuberculosis) management. European Spine Journal, 22(Suppl 4), 529–538.
Fallatah, S. (2013). Posterior inter-body fusion in lumbar spine surgery: A systematic review. Journal of Taibah University Medical Sciences., 8(1), 7–11.
Verma, R., Virk, S., & Qureshi, S. (2020). Interbody fusions in the lumbar spine: A review. HSS Journal, 16(2), 162–167.
Garg, S., Hosalkar, H., & Dormans, J. P. (2007). Autofusion of the cervical spine in 2 children following open biopsy of Langerhans cell histiocytosis. American Journal of Orthopedics, 36(8), E124–E126.
Hyun, S. J., Riew, K. D., & Rhim, S. C. (2013). Range of motion loss after cervical laminoplasty: A prospective study with minimum 5-year follow-up data. Spine Journal, 13(4), 384–390.
Kieser, D. C., Cawley, D. T., Fujishiro, T., et al. (2018). Risk factors for anterior bone loss in cervical disc arthroplasty. Journal of Neurosurgery Spine, 29, 123–129.
Ogawa, Y., Toyama, Y., Chiba, K., et al. (2004). Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. Journal of Neurosurgery Spine, 1(2), 168–174.
Putzier, M., Funk, J. F., Schneider, S. V., et al. (2006). Charité total disc replacement—Clinical and radiographical results after an average follow-up of 17 years. European Spine Journal, 15(2), 183–195.
Li, A. Y., Post, A. F., Dai, J. B., Kamdar, P., & Choudhri, T. F. (2019). Robust bone regrowth achieving autofusion across interlaminar space following lumbar microdiscectomy: Case report. Interdisciplinary Neurosurgery, 17, 143–145.
Lee, C. K., Vessa, P., & Lee, J. K. (1995). Chronic disabling low back pain syndrome caused by internal disc derangements. The results of disc excision and posterior lumbar interbody fusion. Spine, 20, 356–361.
Lenke, L. G., Bridwell, K. H., Bullis, D., Betz, R. R., Baldus, C., & Schoenecker, P. L. (1992). Results of in situ fusion for isthmic spondylolisthesis. Journal of Spinal Disorders, 5, 433–442.
Reid, J. J., Johnson, J. S., & Wang, J. C. (2011). Challenges to bone formation in spinal fusion. Journal of Biomechanics, 44, 213–220.
Korres, D. S., Babis, G. C., Paraskevakou, H., Stamos, K., Tsarouchas, J., & Lykomitros, V. (2000). Spontaneous interbody fusion after controlled injuries to the spine: An experimental study in rabbits. Journal of Spinal Disorders, 13(1), 31–35.
Huang, K. T., Adogwa, O., Babu, R., Lad, S. P., Bagley, C. A., & Gottfried, O. N. (2014). Radiological evidence of spontaneous spinal arthrodesis in patients with lower lumbar spondylolisthesis. Spine, 39(8), 656–663.
Gehrchen, P. M., Dahl, B., Katonis, P., Blyme, P., Tøndevold, E., & Kiær, T. (2002). No difference in clinical outcome after posterolateral lumbar fusion between patients with isthmic spondylolisthesis and those with degenerative disc disease using pedicle screw instrumentation: A comparative study of 112 patients with 4 years of follow-up. European Spine Journal, 11, 423–427.
Ekman, P., Möller, H., Shalabi, A., Yu, Y. X., & Hedlund, R. (2009). A prospective randomised study on the long-term effect of lumbar fusion on adjacent disc degeneration. European Spine Journal, 18, 1175–1186.
Ekman, P., Möller, H., & Hedlund, R. (2009). Predictive factors for the outcome of fusion in adult isthmic spondylolisthesis. Spine, 34, 1204–1210.
Triebel, J., Snellman, G., Sandén, B., Strömqvist, F., & Robinson, Y. (2017). Women do not fare worse than men after lumbar fusion surgery: Two-year follow-up results from 4,780 prospectively collected patients in the Swedish National Spine Register with lumbar degenerative disc disease and chronic low back pain. Spine J, 17(5), 656–662.
Fischgrund, J. S., Mackay, M., Herkowitz, H. N., Brower, R., Montgomery, D. M., & Kurz, L. T. (1997). Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: A prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine, 22, 2807–2812.
Thomsen, K., Christensen, F. B., Eiskjaer, S. P., Hansen, E. S., Fruensgaard, S., & Bünger, C. E. (1997). Volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: A prospective, randomized clinical study. Spine, 22(24), 2813–2822.
Postacchini, F., & Cinotti, G. (1992). Bone regrowth after surgical decompression for lumbar spinal stenosis. Journal of Bone and Joint Surgery. British Volume, 74(6), 862–869.
Lee, S. C., Chen, J. F., Wu, C. T., & Lee, S. T. (2009). In situ local autograft for instrumented lower lumbar or lumbosacral posterolateral fusion. Journal of Clinical Neuroscience, 16(1), 37–43.
Ohtori, S., Suzuki, M., Koshi, T., Takaso, M., Yamashita, M., Yamauchi, K., et al. (2011). Single-level instrumented posterolateral fusion of the lumbar spine with a local bone graft versus an iliac crest bone graft: A prospective, randomized study with a 2-year follow-up. European Spine Journal, 20(4), 635–639.
Inage, K., Ohtori, S., Koshi, T., Suzuki, M., Takaso, M., Yamashita, M., et al. (2011). One, two-, and three-level instrumented posterolateral fusion of the lumbar spine with a local bone graft: A prospective study with a 2-year follow-up. Spine, 36(17), 1392–1396.
Sengupta, D. K., Truumees, E., Patel, C. K., Kazmierczak, C., Hughes, B., Elders, G., et al. (2006). Outcome of local bone versus autogenous iliac crest bone graft in the instrumented posterolateral fusion of the lumbar spine. Spine, 31(9), 985–991.
Audat, Z., Moutasem, O., Yousef, K., & Mohammad, B. (2012). Comparison of clinical and radiological results of posterolateral fusion, posterior lumbar interbody fusion and transforaminal lumbar interbody fusion techniques in the treatment of degenerative lumbar spine. Singapore Medical Journal, 53(3), 183–187.
Høy, K., Bünger, C., Niederman, B., Helmig, P., Hansen, E. S., Li, H., & Andersen, T. (2013). Transforaminal lumbar interbody fusion (TLIF) versus posterolateral instrumented fusion (PLF) in degenerative lumbar disorders: A randomized clinical trial with 2-year follow-up. European Spine Journal, 22(9), 2022–2029.
Farrokhi, M. R., Yadollahikhales, G., Gholami, M., Mousavi, S. R., Mesbahi, A. R., & Asadi-Pooya, A. A. (2018). Clinical outcomes of posterolateral fusion versus posterior lumbar interbody fusion in patients with lumbar spinal stenosis and degenerative instability. Pain Physician, 21, 383–406.
Bozkurt, G., Isikay, I., & Hanalioglu, S. (2018). Radiological and clinical comparison of posterolateral fusion and transforaminal interbody fusion techniques in degenerative lumbar stenosis. World Neurosurgery, 116, e1060–e1065.
Said, E., Abdel-Wanis, M. E., Ameen, M., Sayed, A. A., Mosallam, K. H., Ahmed, A. M., et al. (2021). Posterolateral fusion versus posterior lumbar interbody fusion: A systematic review and meta-analysis of randomized controlled trials. Global Spine Journal. https://doi.org/10.1177/21925682211016426
Lehr, A. M., Oner, F. C., Delawi, D., Stellato, R. K., Hoebink, E. A., Kempen, D. H. R., et al. (2020). Dutch Clinical Spine Research Group. Increasing fusion rate between 1 and 2 years after instrumented posterolateral spinal fusion and the role of bone grafting. Spine, 45(20), 1403–1410.
Acknowledgements
The authors would like to thank Dr. Vikas S. Sharma (MD), CEO, Maverick Medicorum® (India), for statistical analyses and medical writing assistance in the preparation of this article.
Funding
None.
Author information
Authors and Affiliations
Contributions
TA—conceptualisation, design, methodology, interpretation of data, writing, review and editing, approval of the version to be published. SYB—conceptualisation, design, methodology, interpretation of data, writing, review and editing, approval of the version to be published. PBN—interpretation of data, writing, review and editing, approval of the version to be published. ADK—formal analysis, writing, review and editing, approval of the version to be published. MB—formal analysis, writing, review and editing, approval of the version to be published. GP—conceptualisation, design, methodology, interpretation of data, writing, review and editing, approval of the version to be published. HA—conceptualisation, design, methodology, interpretation of data, writing, review and editing, approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflict of interest to declare.
Ethical Approval
The study was performed in line with the principles of the Declaration of Helsinki. Due to retrospective nature of the study, approval of the Institutional Ethics Committee was waived-off.
Informed Consent
As this was a retrospective record review, formal consent from patients was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agarwal, T., Bhojraj, S.Y., Nagad, P.B. et al. Spontaneous Lumbar Interbody Fusion Following Posterolateral Fusion Surgery: A Retrospective Analysis of 5-Year Data. JOIO 58, 598–605 (2024). https://doi.org/10.1007/s43465-024-01148-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-024-01148-w