Abstract
Background
It is well known that the implementation of the WHO surgical safety checklist (SSC) leads to improved operating room team coordination and reduced perioperative complication and mortality rates. Although it is proven to be beneficial worldwide, its awareness and usage need to be evaluated in a diverse country like India. As orthopaedic surgeries involve implants and tourniquet usage, it is important to evaluate the applicability of WHO SSC specifically to orthopaedic surgeries, and whether any modifications are needed.
Materials and Methods
A web-based cross-sectional survey was conducted among Indian Orthopaedic Surgeons with a pre-defined questionnaire regarding awareness, usage and suggestions to modify the existing WHO SSC (2009) for orthopaedic surgeries.
Results
513 responses were included for final analysis. 90.3% of surgeons were aware of the surgical safety checklist; however, only 55.8% used it routinely in their practice. The awareness of SSC availability was 1.85 times more among younger surgeons (< 20 years of experience) than among those with > 20 years of experience. 17% of surgeons thought the usage of SSC was time-consuming and 52.4% of participants felt a need to modify the existing WHO SSC (2009) for orthopaedic surgeries. 34.5% recommended the inclusion of the patient blood group in the “Sign-in” section, 62.77% proposed the inclusion of details about the tourniquet, whereas only 6.63% suggested adding about surgical implant readiness in the “Time-out” section and 72.7% suggested including a check to make sure the tourniquet was deflated, removed and also recording of the total usage time during the “Sign-out” section.
Conclusion
Despite high (90%) awareness among Indian Orthopaedic surgeons, they have limited usage of the WHO SSC in their practice. Identifying barriers and considering modifications for orthopaedic surgeries, like details about tourniquet usage during the “Time-out” section and a check to ensure it was removed during the “Sign-out” section, will improve patient safety and outcomes.
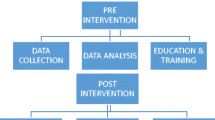
Graphical Abstract







Similar content being viewed by others
References
Haynes, A. B., Weiser, T. G., Berry, W. R., Lipsitz, S. R., Breizat, A.-H.S., Dellinger, E. P., et al. (2009). A surgical safety checklist to reduce morbidity and mortality in a global population. The New England Journal of Medicine, 360(5), 491–499. https://doi.org/10.1056/NEJMsa0810119
van Schoten, S. M., Kop, V., de Blok, C., Spreeuwenberg, P., Groenewegen, P. P., & Wagner, C. (2014). Compliance with a time-out procedure intended to prevent wrong surgery in hospitals: Results of a national patient safety programme in the Netherlands. British Medical Journal Open, 4(7), e005075. https://doi.org/10.1136/bmjopen-2014-005075
WHO Guidelines for Safe Surgery 2009: Safe Surgery Saves Lives. (2009). Geneva: World Health Organization.
Noordin, S., McEwen, J. A., Kragh, J. F., Eisen, A., & Masri, B. A. (2009). Surgical tourniquets in orthopaedics. The Journal of Bone and Joint Surgery American Volume, 91(12), 2958–2967. https://doi.org/10.2106/JBJS.I.00634
Lyons, V. E., & Popejoy, L. L. (2014). Meta-analysis of surgical safety checklist effects on teamwork, communication, morbidity, mortality, and safety. Western Journal of Nursing Research, 36(2), 245–261. https://doi.org/10.1177/0193945913505782
Haynes, A. B., Weiser, T. G., Berry, W. R., Lipsitz, S. R., Breizat, A.-H.S., Dellinger, E. P., et al. (2009). A surgical safety checklist to reduce morbidity and mortality in a global population. New England Journal of Medicine, 360(5), 491–499. https://doi.org/10.1056/NEJMsa0810119
Fudickar, A., Hörle, K., Wiltfang, J., & Bein, B. (2012). The effect of the WHO surgical safety checklist on complication rate and communication. Deutsches Ärzteblatt International, 109(42), 695–701. https://doi.org/10.3238/arztebl.2012.0695
Braham, D. L., Richardson, A. L., & Malik, I. S. (2014). Application of the WHO surgical safety checklist outside the operating theatre: Medicine can learn from surgery. Clinical Medicine, 14(5), 468–474. https://doi.org/10.7861/clinmedicine.14-5-468
Jain, D., Sharma, R., & Reddy, S. (2018). WHO safe surgery checklist: Barriers to universal acceptance. Journal of Anaesthesiology Clinical Pharmacology, 34(1), 7. https://doi.org/10.4103/joacp.JOACP_307_16
Tan, J., Ngwayi, J. R. M., Ding, Z., Zhou, Y., Li, M., Chen, Y., et al. (2021). Attitudes and compliance with the WHO surgical safety checklist: A survey among surgeons and operating room staff in 138 hospitals in China. Patient Safety in Surgery, 15(1), 3. https://doi.org/10.1186/s13037-020-00276-0
Tang, R., Ranmuthugala, G., & Cunningham, F. (2014). Surgical safety checklists: A review. ANZ Journal of Surgery, 84(3), 148–154. https://doi.org/10.1111/ans.12168
Haugen, A. S., Søfteland, E., Almeland, S. K., Sevdalis, N., Vonen, B., Eide, G. E., et al. (2015). Effect of the World Health Organization checklist on patient outcomes: A stepped wedge cluster randomized controlled trial. Annals of Surgery, 261(5), 821–828. https://doi.org/10.1097/SLA.0000000000000716
de Vries, E. N., Prins, H. A., Crolla, R. M. P. H., den Outer, A. J., van Andel, G., van Helden, S. H., et al. (2010). Effect of a comprehensive surgical safety system on patient outcomes. The New England Journal of Medicine, 363(20), 1928–1937. https://doi.org/10.1056/NEJMsa0911535
Delisle, M., Pradarelli, J. C., Panda, N., Koritsanszky, L., Sonnay, Y., Lipsitz, S., et al. (2020). Variation in global uptake of the Surgical Safety Checklist. British Journal of Surgery, 107(2), e151–e160. https://doi.org/10.1002/bjs.11321
Borchard, A., Schwappach, D. L. B., Barbir, A., & Bezzola, P. (2012). A systematic review of the effectiveness, compliance, and critical factors for implementation of safety checklists in surgery. Annals of Surgery, 256(6), 925–933. https://doi.org/10.1097/SLA.0b013e3182682f27
Alnaib, M., Samaraee, A. A., & Bhattacharya, V. (2012). The WHO Surgical Safety Checklist: A review. Journal of Perioperative Practice, 22(9), 289–292. https://doi.org/10.1177/175045891202200903
Papaconstantinou, H. T., Jo, C., Reznik, S. I., Smythe, W. R., & Wehbe-Janek, H. (2013). Implementation of a Surgical Safety Checklist: Impact on surgical team perspectives. Ochsner Journal, 13(3), 299–309.
Tully, P. A., Ng, B., McGagh, D., Meehan, N., Khachane, A., Higgs, J., et al. (2021). Improving the WHO Surgical Safety Checklist sign-out. BJS Open, 5(3), zrab028. https://doi.org/10.1093/bjsopen/zrab028
Motta Filho, Gd. R., Neves da Silva, Ld. F., Ferracini, A. M., & Bähr, G. L. (2013). The WHO Surgical Safety Checklist: Knowledge and use by Brazilian orthopedists. Revista Brasileira de Ortopedia (English Edition), 48(6), 554–562. https://doi.org/10.1016/j.rboe.2013.12.010
Sewell, M., Adebibe, M., Jayakumar, P., Jowett, C., Kong, K., Vemulapalli, K., et al. (2011). Use of the WHO surgical safety checklist in trauma and orthopaedic patients. International Orthopaedics, 35(6), 897–901. https://doi.org/10.1007/s00264-010-1112-7
Norton, E. K., & Rangel, S. J. (2010). Implementing a Pediatric Surgical Safety Checklist in the OR and beyond. AORN Journal, 92(1), 61–71. https://doi.org/10.1016/j.aorn.2009.11.069
Dabholkar, Y., Velankar, H., Suryanarayan, S., Dabholkar, T. Y., Saberwal, A. A., & Verma, B. (2018). Evaluation and customization of WHO Safety Checklist for Patient Safety in otorhinolaryngology. Indian Journal of Otolaryngology and Head & Neck Surgery, 70(1), 149–155. https://doi.org/10.1007/s12070-018-1253-3
Sleiman, B., Sayeed, Z., Padela, M. T., Padela, A. F., Bobba, V., Yassir, W., et al. (2019). Review article: Current literature on surgical checklists and handoff tools and application for orthopaedic surgery. Journal of Orthopaedics, 16(1), 86–90. https://doi.org/10.1016/j.jor.2018.12.006
Thomasson, B. G., Fuller, D., Mansour, J., Marburger, R., & Pukenas, E. (2016). Efficacy of surgical safety checklist: Assessing orthopaedic surgical implant readiness. Healthcare, 4(4), 307–311. https://doi.org/10.1016/j.hjdsi.2016.01.005
Solsky, I., Berry, W., Edmondson, L., Lagoo, J., Baugh, J., Blair, A., et al. (2020). World Health Organization Surgical Safety Checklist modification: Do changes emphasize communication and teamwork? Journal of Surgical Research, 246, 614–622. https://doi.org/10.1016/j.jss.2018.09.035
Barimani, B., Ahangar, P., Nandra, R., & Porter, K. (2020). The WHO Surgical Safety Checklist: A review of outcomes and implementation Strategies. Perioperative Care and Operating Room Management, 21, 100117. https://doi.org/10.1016/j.pcorm.2020.100117
Ragusa, P. S., Bitterman, A., Auerbach, B., & Healy, W. A. (2016). Effectiveness of Surgical Safety Checklists in improving patient safety. Orthopedics, 39(2), e307-310. https://doi.org/10.3928/01477447-20160301-02
Patel, J., Ahmed, K., Guru, K. A., Khan, F., Marsh, H., Shamim, K. M., et al. (2014). An overview of the use and implementation of checklists in surgical specialities—A systematic review. International Journal of Surgery (London, England), 12(12), 1317–1323. https://doi.org/10.1016/j.ijsu.2014.10.031
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rangasamy, K., Jeyaraman, M., Selvaraj, P. et al. Does the WHO Surgical Safety Checklist Need Modification for Orthopaedic Surgery Practices? A Cross-Sectional Survey Among Indian Orthopaedic Surgeons. JOIO 58, 278–288 (2024). https://doi.org/10.1007/s43465-024-01096-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-024-01096-5