Abstract
Background
To explore extraperitoneal approach as an optimal option for reducing peritoneal disruption at a single-level disc in anterior lumbar interbody fusion (ALIF).
Methods
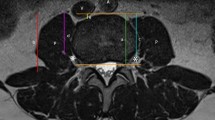
First, abdominal axial CT images obtained from 111 patients were observed to evaluate the distribution of extraperitoneal fat at L2-S1 and measure the lateral distances between the midline and the lateral borders of the rectus and the extraperitoneal fat for each disc level. Second, eight embalmed corpses were dissected along the lateral border of the rectus to expose the peritoneum, which was then separated laterally and medially to evaluate the distribution of fat and peritoneum adhesion. Finally, a total of 58 patients were selected for ALIF. For L2-L4 discs and L4-S1, the pararectus approach and the paramedian approach were utilized, respectively.
Results
Extraperitoneal fat was observed behind the rectus at the L5-S1 and the lateral distance between the fat and midline and the lateral border of the rectus gradually decreased on both sides of L2-5. On the cranial side of the arcuate line, it was easier to separate the peritoneum outward along the lateral edge of the rectus. When bluntly dissected medially, the peritoneum was closely adhered to abdominal wall. No complications such as peritoneal damage, retroperitoneal hematoma and neurological complications occurred in 58 patients undergoing the aforementioned surgical methods.
Conclusions
For L4-S1, the paramedian approach is the optimal technique to expose the disc, whereas the pararectus approach is the feasible surgical method at L2-4.






Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hoy, D., March, L., Brooks, P., Woolf, A., Blyth, F., Vos, T., & Buchbinder, R. (2010). Measuring the global burden of low back pain. Best Practice Research Clinical Rheumatology, 24, 155–165. https://doi.org/10.1016/j.berh.2009.11.002
Goode, A. P., Carey, T. S., & Jordan, J. M. (2013). Low back pain and lumbar spine osteoarthritis: how are they related? Current Rheumatology Reports, 15, 305. https://doi.org/10.1007/s11926-012-0305-z
Rubin, D. I. (2007). Epidemiology and risk factors for spine pain. Neurologic Clinics, 25, 353–371. https://doi.org/10.1016/j.ncl.2007.01.004
Walker, B. F., Muller, R., & Grant, W. D. (2003). Low back pain in Australian adults: the economic burden. Asia-Pacific Journal of Public Health, 15, 79–87. https://doi.org/10.1177/101053950301500202
Hartvigsen, J., Hancock, M. J., Kongsted, A., Louw, Q., Ferreira, M. L., Genevay, S., Hoy, D., Karppinen, J., Pransky, G., Sieper, J., Smeets, R. J., & Underwood, M. (2018). What low back pain is and why we need to pay attention. Lancet, 391, 2356–2367. https://doi.org/10.1016/s0140-6736(18)30480-x
Karunanayake, A. L., Pathmeswaran, A., & Wijayaratne, L. S. (2018). Chronic low back pain and its association with lumbar vertebrae and intervertebral disc changes in adults. A case control study. International Journal of Rheumatic Diseases, 21, 602–610. https://doi.org/10.1111/1756-185x.13026
An, H., Boden, S. D., Kang, J., Sandhu, H. S., Abdu, W., & Weinstein, J. (2003). Summary statement: emerging techniques for treatment of degenerative lumbar disc disease. Spine, 28, 24–25. https://doi.org/10.1097/01.Brs.0000076894.33269.19
Kapustka, B., Kiwic, G., Chodakowski, P., Miodoński, J. P., Wysokiński, T., Łączyński, M., Paruzel, K., Kotas, A., & Marcol, W. (2020). Anterior lumbar interbody fusion (ALIF): biometrical results and own experiences. Neurosurgical Review, 43, 687–693. https://doi.org/10.1007/s10143-019-01108-1
Phan, K., Thayaparan, G. K., & Mobbs, R. J. (2015). Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion–systematic review and meta-analysis. British Journal of Neurosurgery, 29, 705–711. https://doi.org/10.3109/02688697.2015.1036838
Fleege, C., Arabmotlagh, M., Rother, W., Rauschmann, M., & Rickert, M. (2016). ALIF and PLIF interposition in low-grade isthmic spondylolisthesis L5/S1: Longterm-Comparison of interbody fusion techniques (ALIF-PLIF). Der Orthopäde, 45, 760–769. https://doi.org/10.1007/s00132-016-3311-4
Xu, D. S., Walker, C. T., Godzik, J., Turner, J. D., Smith, W., & Uribe, J. S. (2018). Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Ann Transl Med, 6, 104. https://doi.org/10.21037/atm.2018.03.24
Oliveira, L., Marchi, L., Coutinho, E., & Pimenta, L. (2010). A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine, 35, 331–337. https://doi.org/10.1097/BRS.0b013e3182022db0
Rao, P. J., Maharaj, M. M., Phan, K., Lakshan Abeygunasekara, M., & Mobbs, R. J. (2015). Indirect foraminal decompression after anterior lumbar interbody fusion: A prospective radiographic study using a new pedicle-to-pedicle technique. Spine J, 15, 817–824. https://doi.org/10.1016/j.spinee.2014.12.019
Fujibayashi, S., Hynes, R. A., Otsuki, B., Kimura, H., Takemoto, M., & Matsuda, S. (2015). Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine, 40, 175–182. https://doi.org/10.1097/brs.0000000000000703
Sato, J., Ohtori, S., Orita, S., Yamauchi, K., Eguchi, Y., Ochiai, N., Kuniyoshi, K., Aoki, Y., Nakamura, J., Miyagi, M., Suzuki, M., Kubota, G., Inage, K., Sainoh, T., Fujimoto, K., Shiga, Y., Abe, K., Kanamoto, H., Inoue, G., & Takahashi, K. (2017). Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. European Spine Journal, 26, 671–678. https://doi.org/10.1007/s00586-015-4170-0
Phan, K., Xu, J., Scherman, D. B., Rao, P. J., & Mobbs, R. J. (2017). Anterior lumbar interbody fusion with and without an “access surgeon”: a systematic review and meta-analysis. Spine, 42, 592–601. https://doi.org/10.1097/brs.0000000000001905
Quraishi, N. A., Konig, M., Booker, S. J., Shafafy, M., Boszczyk, B. M., Grevitt, M. P., Mehdian, H., & Webb, J. K. (2013). Access related complications in anterior lumbar surgery performed by spinal surgeons. European Spine Journal, 22(1), S16-20. https://doi.org/10.1007/s00586-012-2616-1
Amaral, R., Ferreira, R., Marchi, L., Jensen, R., Nogueira-Neto, J., & Pimenta, L. (2017). Stand-alone anterior lumbar interbody fusion-complications and perioperative results. Rev Bras Ortop, 52, 569–574. https://doi.org/10.1016/j.rboe.2017.08.016
Coffin, A., Boulay-Coletta, I., Sebbag-Sfez, D., & Zins, M. (2015). Radioanatomy of the retroperitoneal space. Diagnostic and Interventional Imaging, 96, 171–186. https://doi.org/10.1016/j.diii.2014.06.015
Mwachaka, P. M., Saidi, H. S., Odula, P. O., Awori, K. O., & Kaisha, W. O. (2010). Locating the arcuate line of douglas: is it of surgical relevance? Clinical Anatomy, 23, 84–86. https://doi.org/10.1002/ca.20877
Cunningham, S. C., Rosson, G. D., Lee, R. H., Williams, J. Z., Lustman, C. A., Slezak, S., Goldberg, N. H., & Silverman, R. P. (2004). Localization of the arcuate line from surface anatomic landmarks: a cadaveric study. Annals of Plastic Surgery, 53, 129–131. https://doi.org/10.1097/01.sap.0000112285.44287.21
Loukas, M., Myers, C., Shah, R., Tubbs, R. S., Wartmann, C., Apaydin, N., Betancor, J., & Jordan, R. (2008). Arcuate line of the rectus sheath: clinical approach. Anatomical Science International, 83, 140–144. https://doi.org/10.1111/j.1447-073X.2007.00221.x
Burkett, D. J., & Burkett, J. S. (2021). Retroperitoneal exposure of the anterior lumbar spine. Oper Neurosurg (Hagerstown), 20, E190-e199. https://doi.org/10.1093/ons/opaa368
Brau, S. A. (2002). Mini-open approach to the spine for anterior lumbar interbody fusion: description of the procedure, results and complications. Spine J, 2, 216–223. https://doi.org/10.1016/s1529-9430(02)00184-5
Edgard-Rosa, G., Geneste, G., Nègre, G., & Marnay, T. (2012). Midline anterior approach from the right side to the lumbar spine for interbody fusion and total disc replacement: a new mobilization technique of the vena cava. Spine, 37, 562–569. https://doi.org/10.1097/BRS.0b013e31823a0a87
Wang, T., Hou, X., Zhou, Z., Liu, J., Zhang, S., Ge, S., Jia, S., & Zheng, L. (2022). Treatment of acetabular fracture involving anterior and posterior columns using a single pararectus approach: surgical experience and preliminary results. International Orthopaedics. https://doi.org/10.1007/s00264-022-05587-8
Wenzel, L., von Rüden, C., Thannheimer, A., Becker, J., Brand, A., Augat, P., & Perl, M. (2020). The pararectus approach in acetabular surgery: radiological and clinical outcome. Journal of Orthopaedic Trauma, 34, 82–88. https://doi.org/10.1097/bot.0000000000001636
Funding
The National Natural Science Foundation of China (82072491) and the Natural Science Foundation of Tianjin (20JCYBJC008200) were received in support of this work.
Author information
Authors and Affiliations
Contributions
KXQ drafted the manuscript; BSX designed the study; KXQ and KSZ dissected cadaver specimens and recorded data; HST analyzed data; BSX managed patients and performed surgery; LLD and KHZ reviewed and revised the manuscript; all the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there is no conflict of interest.
Ethical approval
This study was approved by Institutional Review Board of the tertiary care centre.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qin, K., Tian, H., Zhang, K. et al. Exploration of the Extraperitoneal Approach for Single-Level Anterior Lumbar Interbody Fusion: Imaging, Anatomical and Clinical Research. JOIO 57, 891–898 (2023). https://doi.org/10.1007/s43465-023-00869-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-023-00869-8