Abstract
Objective
To evaluate the role of composite (Chitosan/Chondroitin sulphate/gelatin/nano-bioglass) scaffold in the union of critical size bone defect created in the rabbit’s ulna.
Methods
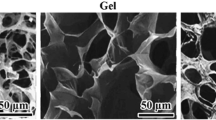
The composite (Chitosan/Chondroitin sulphate/gelatin/nano-bioglass) scaffold was fabricated using the freeze-drying technique under standard laboratory conditions. The scaffold was cut into the appropriate size and transferred into the defect created (critical bone size defect 1 cm) over the right ulna in the rabbit. The scaffold was not implanted on the left side thus the left side ulna served as control. Results were assessed on serial radiological examination. Rabbits were sacrificed at 20 weeks for histopathological examination (Haematoxylin–Eosin staining and Mason’s trichrome staining) and scanning electron microscope observation. Radiological scoring was done by Lane and Sandhu’s scoring.
Results
Among 12 rabbits, 10 could complete the follow-up. Among those 10 rabbits, 8 among the test group showed good evidence of bone formation at the gap non-union scaffold implanted site. Histological evidence of new bone formation, collagen synthesis, scaffold resorption, minimal chondrogenesis was evident by 20 weeks in the test group. Two rabbits had poor bone formation.
Conclusion
The chitosan-chondroitin sulphate-gelatin-nano-bioglass composite scaffold is efficient in osteoconduction and osteoinduction in the gap non-union model as it is biocompatible, bioactive, and non-immunogenic as well.











Similar content being viewed by others
References
Turnbull, G., Clarke, J., Picard, F., et al. (2017). 3D bioactive composite scaffolds for bone tissue engineering. Bioact Mater., 3(3), 278–314. https://doi.org/10.1016/j.bioactmat.2017.10.001.
Campana, V., Milano, G., Pagano, E., et al. (2014). Bone substitutes in orthopaedic surgery: from basic science to clinical practice. Journal of Materials Science. Materials in Medicine, 25(10), 2445–2461. https://doi.org/10.1007/s10856-014-5240-2.
Faour, O., Dimitriou, R., Cousins, C. A., & Giannoudis, P. V. (2011). The use of bone graft substitutes in large cancellous voids: any specific needs? Injury, 42(Suppl 2), S87-90. https://doi.org/10.1016/j.injury.2011.06.020.
Greenwald AS, Boden SD, Goldberg VM, et al. (2001) Bone-graft substitutes: facts, fictions, and applications. J Bone Joint Surg Am. 83-A(Suppl 2 Pt 2):98–103. doi: https://doi.org/10.2106/00004623-200100022-00007
Cooper, G. M., Mooney, M. P., Gosain, A. K., Campbell, P. G., Losee, J. E., & Huard, J. (2010). Testing the “critical-size” in calvarial bone defects: revisiting the concept of a critical-sized defect (CSD). Plastic and Reconstructive Surgery, 125(6), 1685–1692. https://doi.org/10.1097/PRS.0b013e3181cb63a3.
Sohn, H.-S., & Oh, J.-K. (2019). Review of bone graft and bone substitutes with an emphasis on fracture surgeries. Biomaterials Research, 23(1), 9. https://doi.org/10.1186/s40824-019-0157-y.
Goulet, J. A., Senunas, L. E., DeSilva, G. L., & Greenfield, M. L. V. H. (1997). Autogenous iliac crest bone graft: complications and functional assessment. Clinical Orthopaedics and Related Research, 339, 76–81.
Fernandez de Grado G, Keller L, Idoux-Gillet Y, et al. Bone substitutes: a review of their characteristics, clinical use, and perspectives for large bone defects management. J Tissue Eng. 9:2041731418776819. doi: https://doi.org/10.1177/2041731418776819
Schlickewei, W., & Schlickewei, C. (2007). The use of bone substitutes in the treatment of bone defects – the clinical view and history. Macromolecular Symposium, 253(1), 10–23. https://doi.org/10.1002/masy.200750702.
Pryor, L. S., Gage, E., Langevin, C.-J., et al. (2009). Review of bone substitutes. Craniomaxillofacial Trauma Reconstr., 2(3), 151–160. https://doi.org/10.1055/s-0029-1224777.
Singh, B. N., Veeresh, V., Mallick, S. P., et al. (2019). Design and evaluation of chitosan/chondroitin sulfate/nano-bioglass based composite scaffold for bone tissue engineering. International Journal of Biological Macromolecules, 133, 817–830. https://doi.org/10.1016/j.ijbiomac.2019.04.107.
Singh, B. N., Veeresh, V., Mallick, S. P., Sinha, S., Rastogi, A., & Srivastava, P. (2020). Generation of scaffold incorporated with nanobioglass encapsulated in chitosan/chondroitin sulfate complex for bone tissue engineering. International Journal of Biological Macromolecules, 153, 1–16. https://doi.org/10.1016/j.ijbiomac.2020.02.173.
Lane, J. M., & Sandhu, H. S. (1987). Current approaches to experimental bone grafting. Orthopedic Clinics of North America, 18(2), 213–225.
Jones, J. R. (2013). Review of bioactive glass: from Hench to hybrids. Acta Biomaterialia, 9(1), 4457–4486. https://doi.org/10.1016/j.actbio.2012.08.023.
Hench, L. L. (2006). The story of Bioglass. Journal of Materials Science. Materials in Medicine, 17(11), 967–978. https://doi.org/10.1007/s10856-006-0432-z.
Chaudhari, A., Braem, A., Vleugels, J., et al. (2011). Bone tissue response to porous and functionalized titanium and silica based coatings. PLoS ONE, 6(9), e24186. https://doi.org/10.1371/journal.pone.0024186.
Kawakami, T., Antoh, M., Hasegawa, H., Yamagishi, T., Ito, M., & Eda, S. (1992). Experimental study on osteoconductive properties of a chitosan-bonded hydroxyapatite self-hardening paste. Biomaterials, 13(11), 759–763. https://doi.org/10.1016/0142-9612(92)90014-F.
Zou, X. H., Foong, W. C., Cao, T., Bay, B. H., Ouyang, H. W., & Yip, G. W. (2004). Chondroitin sulfate in palatal wound healing. Journal of Dental Research, 83(11), 880–885. https://doi.org/10.1177/154405910408301111.
Büttner, M., Möller, S., Keller, M., et al. (2013). Over-sulfated chondroitin sulfate derivatives induce osteogenic differentiation of hMSC independent of BMP-2 and TGF-β1 signalling. Journal of Cellular Physiology, 228(2), 330–340. https://doi.org/10.1002/jcp.24135.
Kavya, K. C., Dixit, R., Jayakumar, R., Nair, S. V., & Chennazhi, K. P. (2012). Synthesis and characterization of chitosan/chondroitin sulfate/nano-SiO2 composite scaffold for bone tissue engineering. Journal of Biomedical Nanotechnology, 8(1), 149–160. https://doi.org/10.1166/jbn.2012.1363.
Criado Gonzalez, Miryam & Rey, Jose & Mijangos, C. & Hernandez, Rebeca (2016) Doublemembrane thermoresponsive hydrogels from gelatin and chondroitin sulphate with enhanced mechanical properties. RSC Adv 6:105821–105826
Webster, T. J., Ergun, C., Doremus, R. H., Siegel, R. W., & Bizios, R. (2000). Enhanced functions of osteoblasts on nanophase ceramics. Biomaterials, 21(17), 1803–1810. https://doi.org/10.1016/s0142-9612(00)00075-2.
Marelli, B., Ghezzi, C. E., Mohn, D., et al. (2011). Accelerated mineralization of dense collagen-nano bioactive glass hybrid gels increases scaffold stiffness and regulates osteoblastic function. Biomaterials, 32(34), 8915–8926. https://doi.org/10.1016/j.biomaterials.2011.08.016.
Lemos, E. M. F., Patrício, P. S. O., Pereira, M. M., Lemos, E. M. F., Patrício, P. S. O., & Pereira, M. M. (2016). 3D nanocomposite chitosan/bioactive glass scaffolds obtained using two different routes: an evaluation of the porous structure and mechanical properties. Quím Nova., 39(4), 462–466. https://doi.org/10.5935/0100-4042.20160047.
Xu, C., Su, P., Chen, X., et al. (2011). Biocompatibility and osteogenesis of biomimetic bioglass-collagen-phosphatidylserine composite scaffolds for bone tissue engineering. Biomaterials, 32(4), 1051–1058. https://doi.org/10.1016/j.biomaterials.2010.09.068.
Fu, Q., Saiz, E., Rahaman, M. N., & Tomsia, A. P. (2011). Bioactive glass scaffolds for bone tissue engineering: state of the art and future perspectives. Mater Sci Eng C Mater Biol Appl., 31(7), 1245–1256. https://doi.org/10.1016/j.msec.2011.04.022.
Rezwan, K., Chen, Q. Z., Blaker, J. J., & Boccaccini, A. R. (2006). Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials, 27(18), 3413–3431. https://doi.org/10.1016/j.biomaterials.2006.01.039.
Suárez-González, D., Barnhart, K., Saito, E., Vanderby, R., Hollister, S. J., & Murphy, W. L. (2010). Controlled nucleation of hydroxyapatite on alginate scaffolds for stem cell-based bone tissue engineering. J Biomed Mater Res A., 95(1), 222–234. https://doi.org/10.1002/jbm.a.32833.
Zhou, H., & Xu, H. H. (2011). The fast release of stem cells from alginate-fibrin microbeads in injectable scaffolds for bone tissue engineering. Biomaterials, 32(30), 7503–7513. https://doi.org/10.1016/j.biomaterials.2011.06.045.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We hereby declare that we do not have any sort of conflict of interest with any person or authority.
Ethical standard statement
Approval of CPCSEA was obtained for animal experiment.
Informed consent
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Veeresh, V., Sinha, S., Manjhi, B. et al. How is Biodegradable Scaffold Effective in Gap Non-union? Insights from an Experiment. JOIO 55, 741–748 (2021). https://doi.org/10.1007/s43465-020-00313-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-020-00313-1