Abstract
Background
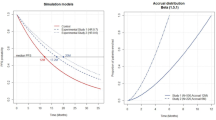
Progression-free survival (PFS) is frequently used as a primary endpoint in late-phase clinical trials for anti-metastatic cancer agents. Previous studies have indicated that the frequency of tumor assessment affects the statistical power for PFS because progression dates are inaccurate; however, this finding may be difficult to generalize because of its unrealistic assumptions. Therefore, we re-examined this issue under realistic assumptions and various scenarios that approximate actual clinical trials.
Methods
Randomized clinical trials comparing two interventions against a solid tumor were simulated under conditions where progressive disease (PD)-dominant PFS or a non-negligible number of deaths (death-competitive PFS) contributed to PFS events, which are conditions that resemble clinical trials of first-line therapy and later-line therapy, respectively. We assessed the impact of tumor assessment frequency on the statistical power.
Results
Under the PD-dominant PFS condition, even in extreme scenarios, statistical power loss was only approximately 3%. Under the death-competitive PFS condition, tumor assessment frequency affected the statistical power of PFS if the effect of the treatment on overall survival was lower than that on time to progression. In this case, loss of statistical power was often more than 10% in some realistic scenarios.
Conclusion
In trials investigating first-line treatments (PD-dominant PFS), tumor assessment frequency has a negligible impact on statistical power, whereas in trials investigating late-line therapies (death-competitive PFS), the potential impact of tumor assessment frequency on statistical power should be carefully evaluated at the design stage.
Similar content being viewed by others
References
Marion S, Sophie G, Anoine I, et al. Meta-analyses evaluating surrogate endpoints for overall survival in cancer randomized trials: a critical review. Crit Rev Oncol Hematol. 2018;123:21–41. https://doi.org/10.1016/j.critrevonc.2017.11.014.
Frederic F, Virginie W, Franck B. Surrogate endpoints for overall survival in lung cancer trials: a review. Expert Rev Anticancer Ther. 2017;5:447–54. https://doi.org/10.1080/14737140.2017.1316196.
Michael PL, Sarah B, Stephanie H, et al. Surrogate threshold effect based on a meta-analysis for the predictive value of progression-free survival for overall survival in hormone receptor-positive, HER2-negative metastatic breast cancer. Breast Cancer Res Treat. 2019;176:495–506. https://doi.org/10.1007/s10549-019-05262-4.
Giuseppe C, Rossella DL, Francesco D. Progression-free survival as a surrogate endpoint of overall survival in patients with metastatic colorectal cancer. Oncol Targets Ther. 2018;11:3059–63. https://doi.org/10.2147/OTT.S151276.
Food & Drug Administration. Guidance for Industry: Clinical Trial Endpoints for the Approval of Cancer Drugs and Biologics. Silver Spring, MD; 2018.
European Medicines Agency. Guideline on the Evaluation of Anticancer Medical Products in Man, London; 2017.
Broglio KR, Berry DA. Detecting an overall survival benefit that is derived from progression-free survival. J Natl Cancer Inst. 2009;101:1642–9. https://doi.org/10.1093/jnci/djp369.
Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13:239–46. https://doi.org/10.1016/S1470-2045(11)70393-X.
Peters S, Camidge DR, Shaw AT, et al. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N Engl J Med. 2017;377:829–38. https://doi.org/10.1056/NEJMoa1704795.
Robert NJ, Diéras V, Glaspy J, et al. RIBBON-1: randomized, double-blind, placebo-controlled, phase III trial of chemotherapy with or without bevacizumab for first-line treatment of human epidermal growth factor receptor 2-negative, locally recurrent or metastatic breast cancer. J Clin Oncol. 2011;29:1252–60. https://doi.org/10.1200/JCO.2010.28.0982.
Robson M, Im SA, Senkus E, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377:523–33. https://doi.org/10.1056/NEJMoa1706450.
Saltz LB, Clarke S, Díaz-Rubio E, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol. 2008;26:2013–9. https://doi.org/10.1200/JCO.2007.14.9930.
Yamada Y, Takahari D, Matsumoto H, et al. Leucovorin, fluorouracil, and oxaliplatin plus bevacizumab versus S-1 and oxaliplatin plus bevacizumab in patients with metastatic colorectal cancer (SOFT): an open-label, non-inferiority, randomised phase 3 trial. Lancet Oncol. 2013;14:1278–86. https://doi.org/10.1016/S1470-2045(13)70490-X.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Carroll KJ. Analysis of progression-free survival in oncology trials: some common statistical issues. Pharm Stat. 2007;6:99–113. https://doi.org/10.1002/pst.251.
Tanase T, Hamada C, Yoshino T, et al. A proposal for progression-free survival assessment in patients with early progressive cancer. Anticancer Res. 2017;37:5851–5. https://doi.org/10.21873/anticanres.12029.
Michael JR, Schucany WR. The mixture approach for simulating new families of bivariate distributions with specified correlations. Am Statistician. 2002;56:48–54. https://doi.org/10.2307/3087327.
Acknowledgements
The authors would like to thank the associate editor and referees for very helpful suggestions that substantially improved the article.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Analysis was performed by Yuki Nakagawa and Takuya Yoshimoto. The first draft of the manuscript was written by Yuki Nakagawa and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors are employees of Chugai Pharmaceutical Co., Ltd.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nakagawa, Y., Yoshimoto, T., Nakagawa, S. et al. Impact of Tumor Assessment Frequency on Statistical Power in Randomized Cancer Clinical Trials Evaluating Progression-Free Survival. Ther Innov Regul Sci 55, 1258–1264 (2021). https://doi.org/10.1007/s43441-021-00328-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43441-021-00328-2