Abstract
In late 2018, the Food and Drug Administration (FDA) outlined a framework for evaluating the possible use of real-world evidence (RWE) to support regulatory decision-making. This framework was created to facilitate studies that would generate high-quality RWE, including pragmatic clinical trials (PCTs), which are randomized trials designed to inform clinical or policy decisions by assessing the real-world effectiveness of an intervention. There is general agreement among experts that the use of existing healthcare and patient-generated data holds promise for making randomized trials more efficient, less costly, and more generalizable. Yet the benefits of relying on real-world data sources must be weighed against difficulties with ensuring data integrity and completeness. Additionally, appropriately monitoring patient safety in randomized trials of new drugs using healthcare system data that might not be available in real time can be quite difficult. Recognizing that these and other concerns are critical to the development and acceptability of PCTs, a group of stakeholders from academia, industry, professional organizations, regulatory bodies, government agencies, and patient advocates discussed a path forward for PCT growth and sustainability at a think tank meeting entitled “Monitoring and Analyzing Data from Pragmatic Streamlined Randomized Clinical Trials,” which took place in January 2019 (Washington, DC). The goals of this meeting were to: (1) evaluate study design and methodological options specific to PCTs that have the potential to yield high-quality evidence; (2) discuss best practices to ensure data quality in PCTs; and (3) identify appropriate methods for study monitoring. Proceedings from the think tank meeting are summarized in this manuscript.




Similar content being viewed by others
References
Reinsel D, Gantz J, Rydning J. International Data Corporation. Data Age 2025. The Digitization of the World: From Edge to Core. SEAGATE web site. https://www.seagate.com/files/www-content/our-story/trends/files/idc-seagate-dataage-whitepaper.pdf. Published Nov 2018. Accessed 31 Jul 2019.
U.S. Food & Drug Administration (FDA). Framework for FDA’s Real-World Evidence Program. FDA web site. https://www.fda.gov/media/120060/download. Published Dec 2018. Accessed 31 Jul 2019.
Sherman RE, Anderson SA, Dal Pan GJ, et al. Real-world evidence—what is it and what can it tell us? N Engl J Med. 2016;375:2293–7.
First International Study of Infarct Survival Collaborative Group. Randomised trial of intravenous atenolol among 16 027 cases of suspected acute myocardial infarction: ISIS-1. Lancet. 1986;2:57–66.
ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet. 1988;2:349–60.
ISIS-3 (Third International Study of Infarct Survival) Collaborative Group. ISIS-3: a randomised comparison of streptokinase vs tissue plasminogen activator vs anistreplase and of aspirin plus heparin vs aspirin alone among 41,299 cases of suspected acute myocardial infarction. Lancet. 1992;339:753–70.
ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group. ISIS-4: a randomised factorial trial assessing early oral captopril, oral mononitrate, and intravenous magnesium sulphate in 58,050 patients with suspected acute myocardial infarction. Lancet. 1995;345:669–85.
Gökbuget N, Kelsh M, Chia V, et al. Blinatumomab vs historical standard therapy of adult relapsed/refractory acute lymphoblastic leukemia. Blood Cancer J. 2016;6:e473.
Daniel GW, Menis M, Sridhar G, et al. Immune globulins and thrombotic adverse events as recorded in a large administrative database in 2008 through 2010. Transfusion. 2012;52:2113–211.
Jarow JP, LaVange L, Woodcock J. Multidimensional evidence generation and FDA regulatory decision making: defining and using “real-world” data. JAMA. 2017;318:703–4.
Gabay M. 21st Century Cures Act. Hosp Pharm. 2017;52:264–5.
Ford I, Norrie J. Pragmatic trials. N Engl J Med. 2016;375:454–63.
Schwartz D, Lellouch J. Explanatory and pragmatic attitudes in therapeutical trials. J Clin Epidemiol. 2009;62:499–505.
Stafford PB, Garrett A. Using real-time data to drive better decisions, fater. Drug Inform. J. 2011;45:495–502.
Aroda VR, Saugstrup T, Buse JB, Donsmark M, Zacho J, Davies MJ. Incorporating and interpreting regulatory guidance on estimands in diabetes clinical trials: the PIONEER 1 randomized clinical trial as an example. Diabet Obes Metab. 2019;21(10):2203–10.
Loudon K, Treweek S, Sullivan F, et al. The PRECIS-2 tool: designing trials that are fit for purpose. BMJ. 2015;350:h2147.
Johnson KE, Neta G, Dember LM, et al. Use of PRECIS ratings in the National Institutes of Health (NIH) Health Care Systems Research Collaboratory. Trials. 2016;17:32.
Loudon K, Zwarenstein M, Sullivan F, et al. Making clinical trials more relevant: improving and validating the PRECIS tool for matching trial design decisions to trial purpose. Trials. 2013;14:115.
North American Symptomatic Carotid Endarterectomy Trial Collaborators, Barnett HJM, Taylor DW, et al. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325:445–53.
Jarvik JG, Comstock BA, James KT, et al. Lumbar imaging with reporting of epidemiology (LIRE): protocol for a pragmatic cluster randomized trial. Contemp Clin Trials. 2015;45:157–63.
Thorpe KE, Zwarenstein M, Oxman AD, et al. A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. CMAJ. 2009;180:E47–57.
Welsing PM, Oude Rengerink K, Collier S, et al. Series: pragmatic trials and real world evidence: paper 6. Outcome measures in the real world. J Clin Epidemiol. 2017;90:99–107.
Christian JB, Brouwer ES, Girman CJ, Dennett D, Davis KJ, Dreyer NA. Masking in pragmatic trials: who, what, and when to blind. Ther Innov Regul Sci. 2020;54:431–6.
Turner EL, Li F, Gallis JA, et al. Review of recent methodological developments in group-randomized trials: part 1-design. Am J Public Health. 2017;107:907–15.
Donner A, Klar N. Pitfalls of and controversies in cluster randomization trials. Am J Public Health. 2004;94:416–22.
Turner EL, Prague M, Gallis JA, et al. Review of recent methodological developments in group-randomized trials: part 2-analysis. Am J Public Health. 2017;107:1078–86.
Hughes JP, Granston TS, Heagerty PJ. Current issues in the design and analysis of stepped wedge trials. Contemp Clin Trials. 2015;45:55–60.
Cook AJ, Delong E, Murray DM, et al. Statistical lessons learned for designing cluster randomized pragmatic clinical trials from the NIH Health Care Systems Collaboratory Biostatistics and Design Core. Clin Trials. 2016;13:504–12.
Ellenberg SS. The stepped-wedge clinical trial: evaluation by rolling deployment. JAMA. 2018;319:607–8.
McKinney RE, Beskow LM, Ford DE, et al. Use of altered informed consent in pragmatic clinical research. Clin Trials Lond Engl. 2015;12:494–502.
U.S. Food & Drug Administration (FDA). Use of Electronic Informed Consent in Clinical Investigations—Questions and Answers | FDA. FDA web site. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/use-electronic-informed-consent-clinical-investigations-questions-and-answers. Updated 24 Aug 2018. Accessed 21 May 2019.
Aspirin Dosing: A Patient-Centric Trial Assessing Benefits and Long-term (ADAPTABLE). ClinicalTrials.gov web site. https://clinicaltrials.gov/ct2/show/NCT02697916. Updated 31 Jan 2019. Accessed 31 Jul 2019.
Johnston A, Jones WS, Hernandez AF. The ADAPTABLE trial and aspirin dosing in secondary prevention for patients with coronary artery disease. Curr Cardiol Rep. 2016;18:81.
ADAPTABLE prescreen video for patients. ADAPTABLE patient web site. https://adaptablepatient.com/en/prescreen/watch-video. Accessed July 31, 2019.
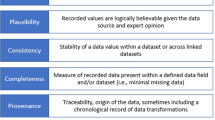
Mahendraratnam N, Silcox C, Mercon K, et al. Determining real-world data’s fitness for use and the role of reliability. Duke-Margolis Center for Health Policy; September 26, 2019.
Mayernik M, DiLauro T, Duerr R, et al. Data conservancy provenance, context, and lineage services: key components for data preservation and curation. Data Sci J. 2013;12:158–71.
El Fadly A, Rance B, Lucas N, et al. Integrating clinical research with the Healthcare Enterprise: from the RE-USE project to the EHR4CR platform. J Biomed Inform. 2011;44:S94–S102.
Nordo AH, Eisenstein EL, Hawley J, et al. A comparative effectiveness study of eSource used for data capture for a clinical research registry. Int J Med Inf. 2017;103:89–94.
Nordo AH, Levaux HP, Becnel LB, et al. Use of EHRs data for clinical research: historical progress and current applications. Learn Health Syst. 2019;3:e10076.
Guimarães PO, Krishnamoorthy A, Kaltenbach LA, et al. Accuracy of medical claims for identifying cardiovascular and bleeding events after myocardial infarction: a secondary analysis of the TRANSLATE-ACS study. JAMA Cardiol. 2017;2:750–7.
Phelan M, Bhavsar NA, Goldstein BA. Illustrating informed presence bias in electronic health records data: how patient interactions with a health system can impact inference. EGEMS Wash DC. 2017;5:22.
Ahmad T, Lund LH, Rao P, et al. Machine learning methods improve prognostication, identify clinically distinct phenotypes, and detect heterogeneity in response to therapy in a large cohort of heart failure patients. J Am Heart Assoc. 2018;7:10.
Tudor Smith C, Stocken DD, Dunn J, et al. The value of source data verification in a cancer clinical trial. PLoS ONE. 2012;7:e51623.
Anderson JR, Byrjalsen I, Bihlet A, et al. Impact of source data verification on data quality in clinical trials: an empirical post hoc analysis of three phase 3 randomized clinical trials. Br J Clin Pharmacol. 2015;79:660–8.
Olsen R, Bihlet AR, Kalakou F, et al. The impact of clinical trial monitoring approaches on data integrity and cost: a review of current literature. Eur J Clin Pharmacol. 2016;72:399–412.
Ellenberg SS, Culbertson R, Gillen DL, et al. Data monitoring committees for pragmatic clinical trials. Clin Trials Lond Engl. 2015;12:530–6.
Acknowledgements
The authors would like to thank Jennifer Gloc for her leadership and guidance in this manuscript effort, and Erin Campbell for her editorial contributions. Ms. Gloc and Ms. Campbell did not receive compensation for their contributions, apart from their employment at Duke Clinical Research Institute (Durham, NC USA).
Funding
This manuscript was funded internally by the Duke Clinical Research Institute (Durham, North Carolina). Funding support for the think tank meeting was provided through registration fees from AbbVie, Amgen, AstraZeneca, Bayer AG, Boehringer Ingelheim International GmbH, Eli Lilly and Company, Janssen Pharmaceutical Companies of Johnson & Johnson, Pfizer, and Sanofi.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Trevor A. Lentz reports no relevant disclosures. Lesley H. Curtis reports no relevant disclosures. Frank W. Rockhold reports grants from PCORI, the NIH, AstraZeneca, and Eidos Therapeutics; personal fees from Janssen, Amgen, Merck Healthcare KgaA, Merck Research Laboratories, NovoNordisk, and Eidos Therapeutics; other from GlaxoSmithKline and AthiraovoNordisk. David Martin reports no relevant disclosures. Tomas LG Andersson reports being an employee of AstraZeneca. Carolyn Arias reports no relevant disclosures. Jesse A. Berlin reports being an employee of Johnson & Johnson; holds equity in Johnson & Johnson. Cherie Binns reports no relevant disclosures. Andrea Cook reports no relevant disclosures. Mark Cziraky reports no relevant disclosures, but states even though he did not receive any direct payment, his company, HealthCore, conducts multiple research projects supported by various pharmaceutical companies. Ricardo Dent reports no relevant disclosures. Manisha Desai reports no relevant disclosures. Andrew Emmett reports no relevant disclosures. Denise Esserman reports no relevant disclosures. Jyothis George reports being an employee of Boehringer Ingelheim during the conduct of the study. Stefan Hantel reports being an employee of Boehringer Ingelheim Pharma GmbH & Co. KG, Germany. Patrick Heagerty reports no relevant disclosures. Adrian F. Hernandez reports no relevant disclosures. Thomas Hucko reports no relevant disclosures. Naeem Khan reports being a full-time employee of AstraZeneca. Shun Fu Lee reports no relevant disclosures. Robert LoCasale reports no relevant disclosures. Jack Mardekian reports being an employee of Pfizer Inc.; owning stock in Pfizer Inc. Debbe McCall reports no relevant disclosures. Keri Monda reports no relevant disclosures. Sharon-Lise Normand reports no relevant disclosures. Jeffrey Riesmeyer reports no relevant disclosures. Matthew Roe reports no relevant disclosures. Lothar Roessig reports being a full-time employee of Bayer AG. Rob Scott reports no relevant disclosures. Harald Siedentop has no relevant disclosures. Joanne Waldstreicher reports being an employee and shareholder for Johnson & Johnson; a former employee and former shareholder for Merck & Co. Lin Wang reports no relevant disclosures. Govinda Weerakkody reports no relevant disclosures. Myles Wolf served as a consultant to Akebia, AMAG, Amgen, Ardelyx, DiaDorin, Luitpold, and Pharmacosmos. Susan S. Ellenberg reports no relevant disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer
The views expressed are those of the authors and do not necessarily represent the views of their organization.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lentz, T.A., Curtis, L.H., Rockhold, F.W. et al. Designing, Conducting, Monitoring, and Analyzing Data from Pragmatic Randomized Clinical Trials: Proceedings from a Multi-stakeholder Think Tank Meeting. Ther Innov Regul Sci 54, 1477–1488 (2020). https://doi.org/10.1007/s43441-020-00175-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43441-020-00175-7