Abstract
Natural compounds originating from plants offer a wide range of pharmacological potential and have traditionally been used to treat a wide range of diseases including cancer. Tanshinone IIA (Tan IIA), a bioactive molecule found in the roots of the Traditional Chinese Medicine (TCM) herb Salvia miltiorrhiza, has been shown to have remarkable anticancer properties through several mechanisms, such as inhibition of tumor cell growth and proliferation, metastasis, invasion, and angiogenesis, as well as induction of apoptosis and autophagy. It has demonstrated excellent anticancer efficacy against cell lines from breast, cervical, colorectal, gastric, lung, and prostate cancer by modulating multiple signaling pathways including PI3K/Akt, JAK/STAT, IGF-1R, and Bcl-2–Caspase pathways. This review focuses on the role of Tan IIA in the treatment of various cancers, as well as the underlying molecular mechanisms.



Similar content being viewed by others
Availability of data and materials
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- AACT:
-
Acetyl-CoA C-acetyltransferase
- Akt:
-
Protein kinase B
- AML:
-
Acute myeloid leukemia
- AMPK:
-
AMP-activated protein kinase
- AP-1:
-
Activator protein 1
- ATF6:
-
Activating transcription factor 6
- AURKA:
-
Aurora kinase A
- BAX:
-
Bcl-2-associated X protein
- Bcl-XL:
-
B-cell lymphoma-extra large
- bFGF:
-
Basic fibroblast growth factor
- BIP:
-
Binding immunoglobulin protein
- CD80:
-
Cluster of differentiation 80
- Cdc25A:
-
Cell division cycle 25 A
- CDK:
-
Cyclin-dependent kinases
- CHOP:
-
C/EBP homologous protein
- CML:
-
Chronic myeloid leukemia
- CPP:
-
Copalyl diphosphate
- CRC:
-
Colorectal cancer cells
- CTLA-4:
-
Cytotoxic T-lymphocyte associated antigen-4
- DMAPP:
-
Dimethylallyl pyrophosphate
- DXS:
-
1-Deoxy-D-xylulose-5-phosphate synthase
- EGFR:
-
Epithelial growth factor receptor
- eIF2α:
-
Eukaryotic translation initiation factor 2α
- ERK:
-
Extracellular signal-related kinase
- FLIPs:
-
FLICE inhibitory protein
- FOXM1:
-
Forkhead box protein M1
- FPP:
-
Farnesyl diphosphate
- FPPS:
-
FPP synthase
- G3P:
-
Glyceraldehyde-3-phosphate
- GADD153:
-
α Growth arrest and DNA damage-inducible gene 153
- GFAP:
-
Glial fibrillary acidic protein
- GGPP:
-
Geranylgeranyl diphosphate
- GGPPS:
-
GGPP synthase
- GPP:
-
Geranyl diphosphate
- GPPS:
-
GPP synthase
- HER2:
-
Receptor tyrosine-protein kinase erbB-2
- HIF-1 α:
-
Hypoxia-inducible factor 1 α
- HMGR:
-
3-Hydroxy-3-methylglutaryl-CoA reductase
- HPV:
-
Human papillomavirus
- IGF-1:
-
Insulin-like growth factor- 1
- IL-6:
-
Interleukin 6
- IL-8:
-
Pro-inflammatory cytokine interleukin-8
- IPI:
-
IPP isomerase
- IPP:
-
Isopentenyl pyrophosphate
- IRE1:
-
Inositol-requiring gene 1
- JAK:
-
Janus-activated kinase
- JNK:
-
C-jun N-terminal kinase
- KEGG:
-
KEGG: Kyoto Encyclopedia of Genes and Genomes
- Ki-67:
-
Antigen KI-67
- MAPK:
-
Mitogen-activated protein kinase
- MEP:
-
Methylerythritol phosphate
- MFF:
-
Mitochondrial fission factor
- MMP-2:
-
Matrix metalloproteinase 2
- mTOR:
-
Mammalian target of rapamycin
- MVA:
-
Mevalonate
- NF-κB:
-
Nuclear factor kappa B
- Notch-1:
-
Notch homolog 1
- NSCLC:
-
Non‐small cell lung cancer
- PARP:
-
Poly(ADP ribose) polymerase
- PC12:
-
Pheochromocytoma cells
- PCNA:
-
Proliferating cell nuclear antigen
- PD-1:
-
Programmed cell death-1 receptor
- PD-L1:
-
Programmed cell death-ligand 1
- PERK:
-
Protein kinase RNA-like endoplasmic reticulum kinase
- PI3K:
-
Phosphatidylinositol-3-kinase
- PKC:
-
Protein kinase C
- PLC:
-
Phospholipase C
- RAS:
-
Rat sarcoma virus
- Rb:
-
Retinoblastoma
- Skp2:
-
S-phase kinase-associated protein 2
- SmCPS:
-
CPP synthase
- SmKSL:
-
Kaurene synthase-like cyclase
- STAT3:
-
Signal transducer and activator of transcription 3
- Tan IIA:
-
Tanshinone IIA
- TCM:
-
Traditional Chinese Medicine
- TIMP:
-
Tissue inhibitor of matrix metalloproteinase protein
- uPA:
-
Urokinase plasminogen activator
- VEGF/VEGFR2:
-
Vascular endothelial growth factor/VEGF receptor 2
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74. https://doi.org/10.1016/j.cell.2011.02.013.
Dutta S. Natural products: an upcoming therapeutic approach to cancer. Food Chem Toxicol. 2019;120:240–55.
Martin GS. Cell signaling and cancer. Cancer Cell 2003;4:167–74. https://doi.org/10.1016/S1535-6108(03)00216-2.
Gotwals P, Cameron S, Cipolletta D, Cremasco V, Crystal A, Hewes B, et al. Prospects for combining targeted and conventional cancer therapy with immunotherapy. Nat Rev Cancer. 2017;17:286–301. https://doi.org/10.1038/nrc.2017.17.
Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–61. https://doi.org/10.1016/j.ccell.2015.03.001.
Huang C-Y, Ju D-T, Chang C-F, Muralidhar Reddy P, Velmurugan BK. A review on the effects of current chemotherapy drugs and natural agents in treating non–small cell lung cancer. Biomedicine. 2017;7:23. https://doi.org/10.1051/bmdcn/2017070423.
Uddin F, Hoque M. Non-flavonoids targeting cancer stem cells: a promising therapeutic avenue for cancer treatment. In: Tabrez S, Imran Khan M, editors. Polyphenols-based nanotherapeutics cancer management. Singapore: Springer; 2021. p. 289–334. https://doi.org/10.1007/978-981-16-4935-6_8.
Christen P, Cuendet M. Plants as a source of therapeutic and health products. Chim Int J Chem. 2012;66:320–3. https://doi.org/10.2533/chimia.2012.320.
Hashem S, Ali TA, Akhtar S, Nisar S, Sageena G, Ali S, et al. Targeting cancer signaling pathways by natural products: exploring promising anti-cancer agents. Biomed Pharmacother. 2022;150:113054. https://doi.org/10.1016/j.biopha.2022.113054.
Wang H, Oo Khor T, Shu L, Su Z-Y, Fuentes F, Lee J-H, et al. Plants vs cancer: a review on natural phytochemicals in preventing and treating cancers and their druggability. Anticancer Agents Med Chem. 2012;12:1281–305. https://doi.org/10.2174/187152012803833026.
Jiang Z, Gao W, Huang L. Tanshinones, critical pharmacological components in Salvia miltiorrhiza. Front Pharmacol. 2019;10:202. https://doi.org/10.3389/fphar.2019.00202.
Ansari MA, Khan FB, Safdari HA, Almatroudi A, Alzohairy MA, Safdari M, et al. Prospective therapeutic potential of Tanshinone IIA: an updated overview. Pharmacol Res. 2021;164:105364. https://doi.org/10.1016/j.phrs.2020.105364.
Fu L, Han B, Zhou Y, Ren J, Cao W, Patel G, et al. The anticancer properties of tanshinones and the pharmacological effects of their active ingredients. Front Pharmacol. 2020;11:193. https://doi.org/10.3389/fphar.2020.00193.
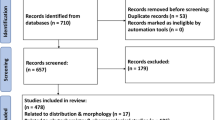
Alam SSM, Uddin F, Khan FB, Kamal MA, Hoque M. Therapeutic and pharmacological potential of Tanshinones against lung cancer: a systematic review. Phytomedicine Plus. 2022;2:100202. https://doi.org/10.1016/j.phyplu.2021.100202.
Lv C, Zeng H-W, Wang J-X, Yuan X, Zhang C, Fang T, et al. The antitumor natural product tanshinone IIA inhibits protein kinase C and acts synergistically with 17-AAG. Cell Death Dis. 2018;9:165. https://doi.org/10.1038/s41419-017-0247-5.
Lu L, Liu Y, Zhang Z, Zhang H. Analysis of Danshen and twelve related Salvia species. Nat Prod Commun. 2012;7:1934578X1200700. https://doi.org/10.1177/1934578X1200700121.
Won S-H, Lee H-J, Jeong S-J, Lee H-J, Lee E-O, Jung D-B, et al. Tanshinone IIA induces mitochondria dependent apoptosis in prostate cancer cells in association with an inhibition of phosphoinositide 3-kinase/AKT pathway. Biol Pharm Bull. 2010;33:1828–34. https://doi.org/10.1248/bpb.33.1828.
Zhong C, Lin Z, Ke L, Shi P, Li S, Huang L, et al. Recent research progress (2015–2021) and perspectives on the pharmacological effects and mechanisms of Tanshinone IIA. Front Pharmacol. 2021;12:778847. https://doi.org/10.3389/fphar.2021.778847.
Dong Y, Morris-Natschke SL, Lee K-H. Biosynthesis, total syntheses, and antitumor activity of tanshinones and their analogs as potential therapeutic agents. Nat Prod Rep. 2011;28:529. https://doi.org/10.1039/c0np00035c.
Gao W, Sun H-X, Xiao H, Cui G, Hillwig ML, Jackson A, et al. Combining metabolomics and transcriptomics to characterize tanshinone biosynthesis in Salvia miltiorrhiza. BMC Genomics. 2014;15:73. https://doi.org/10.1186/1471-2164-15-73.
Guo J, Zhou YJ, Hillwig ML, Shen Y, Yang L, Wang Y, et al. CYP76AH1 catalyzes turnover of miltiradiene in tanshinones biosynthesis and enables heterologous production of ferruginol in yeasts. Proc Natl Acad Sci. 2013;110:12108–13. https://doi.org/10.1073/pnas.1218061110.
Rohmer M, Knani M, Simonin P, Sutter B, Sahm H. Isoprenoid biosynthesis in bacteria: a novel pathway for the early steps leading to isopentenyl diphosphate. Biochem J. 1993;295:517–24. https://doi.org/10.1042/bj2950517.
Rodrı́guez-Concepción M, Boronat A. Elucidation of the methylerythritol phosphate pathway for isoprenoid biosynthesis in bacteria and plastids. A metabolic milestone achieved through genomics. Plant Physiol. 2002;130:1079–89. https://doi.org/10.1104/pp.007138.
Kai G, Xu H, Zhou C, Liao P, Xiao J, Luo X, et al. Metabolic engineering tanshinone biosynthetic pathway in Salvia miltiorrhiza hairy root cultures. Metab Eng. 2011;13:319–27. https://doi.org/10.1016/j.ymben.2011.02.003.
Ma Y, Yuan L, Wu B, Li X, Chen S, Lu S. Genome-wide identification and characterization of novel genes involved in terpenoid biosynthesis in Salvia miltiorrhiza. J Exp Bot. 2012;63:2809–23. https://doi.org/10.1093/jxb/err466.
Miziorko HM. Enzymes of the mevalonate pathway of isoprenoid biosynthesis. Arch Biochem Biophys. 2011;505:131–43. https://doi.org/10.1016/j.abb.2010.09.028.
Ge X, Wu J. Tanshinone production and isoprenoid pathways in Salvia miltiorrhiza hairy roots induced by Ag+ and yeast elicitor. Plant Sci. 2005;168:487–91. https://doi.org/10.1016/j.plantsci.2004.09.012.
Yang D, Du X, Liang X, Han R, Liang Z, Liu Y, et al. Different roles of the mevalonate and methylerythritol phosphate pathways in cell growth and tanshinone production of Salvia miltiorrhiza hairy roots. PLoS ONE. 2012;7:e46797. https://doi.org/10.1371/journal.pone.0046797.
Dai Z, Cui G, Zhou S-F, Zhang X, Huang L. Cloning and characterization of a novel 3-hydroxy-3-methylglutaryl coenzyme A reductase gene from Salvia miltiorrhiza involved in diterpenoid tanshinone accumulation. J Plant Physiol. 2011;168:148–57. https://doi.org/10.1016/j.jplph.2010.06.008.
Ma X-H, Ma Y, Tang J-F, He Y-L, Liu Y-C, Ma X-J, et al. The biosynthetic pathways of tanshinones and phenolic acids in Salvia miltiorrhiza. Molecules. 2015;20:16235–54. https://doi.org/10.3390/molecules200916235.
Kirby J, Keasling JD. Biosynthesis of plant isoprenoids: perspectives for microbial engineering. Annu Rev Plant Biol. 2009;60:335–55. https://doi.org/10.1146/annurev.arplant.043008.091955.
Bae WJ, Choi JB, Kim KS, Ha US, Hong SH, Lee JY, et al. Inhibition of proliferation of prostate cancer cell line DU-145 in vitro and in vivo using Salvia miltiorrhiza Bunge. Chin J Integr Med. 2020;26:533–8. https://doi.org/10.1007/s11655-017-2801-5.
Chen X, Guo J, Bao J, Lu J, Wang Y. The anticancer properties of Salvia miltiorrhiza Bunge (Danshen): a systematic review: the anticancer effects of salvia miltiorrhiza bunge. Med Res Rev. 2014;34:768–94. https://doi.org/10.1002/med.21304.
Wu C-Y, Yang Y-H, Lin Y-Y, Kuan F-C, Lin Y-S, Lin W-Y, et al. Anti-cancer effect of danshen and dihydroisotanshinone I on prostate cancer: targeting the crosstalk between macrophages and cancer cells via inhibition of the STAT3/CCL2 signaling pathway. Oncotarget. 2017;8:40246–63. https://doi.org/10.18632/oncotarget.14958.
Xie J, Liu J, Liu H, Liang S, Lin M, Gu Y, et al. The antitumor effect of tanshinone IIA on anti-proliferation and decreasing VEGF/VEGFR2 expression on the human non-small cell lung cancer A549 cell line. Acta Pharm Sin B. 2015;5:554–63. https://doi.org/10.1016/j.apsb.2015.07.008.
Munagala R, Aqil F, Jeyabalan J, Gupta RC. Tanshinone IIA inhibits viral oncogene expression leading to apoptosis and inhibition of cervical cancer. Cancer Lett. 2015;356:536–46. https://doi.org/10.1016/j.canlet.2014.09.037.
Zhang H-S, Zhang F-J, Li H, Liu Y, Du G-Y, Huang Y-H. Tanshinone IIA inhibits human esophageal cancer cell growth through miR-122-mediated PKM2 down-regulation. Arch Biochem Biophys. 2016;598:50–6. https://doi.org/10.1016/j.abb.2016.03.031.
Chen J, Shi D-Y, Liu S-L, Zhong L. Tanshinone IIA induces growth inhibition and apoptosis in gastric cancer in vitro and in vivo. Oncol Rep. 2012;27:523–8. https://doi.org/10.3892/or.2011.1524.
Su C-C. Tanshinone IIA inhibits gastric carcinoma AGS cells through increasing p-p38, p-JNK and p53 but reducing p-ERK, CDC2 and cyclin B1 expression. Anticancer Res. 2014;34:7097–110.
Gong Y, Li Y, Lu Y, Li L, Abdolmaleky H, Blackburn GL, et al. Bioactive tanshinones in Salvia miltiorrhiza inhibit the growth of prostate cancer cells in vitro and in mice. Int J Cancer. 2011;129:1042–52. https://doi.org/10.1002/ijc.25678.
Lin L-L, Hsia C-R, Hsu C-L, Huang H-C, Juan H-F. Integrating transcriptomics and proteomics to show that tanshinone IIA suppresses cell growth by blocking glucose metabolism in gastric cancer cells. BMC Genom. 2015;16:41. https://doi.org/10.1186/s12864-015-1230-0.
Wang J-F, Feng J-G, Han J, Zhang B-B, Mao W-M. The molecular mechanisms of tanshinone IIA on the apoptosis and arrest of human esophageal carcinoma cells. BioMed Res Int. 2014;2014:1–9. https://doi.org/10.1155/2014/582730.
Dai Z-K, Qin J-K, Huang J-E, Luo Y, Xu Q, Zhao H-L. Tanshinone IIA activates calcium-dependent apoptosis signaling pathway in human hepatoma cells. J Nat Med 2012;66:192–201. https://doi.org/10.1007/s11418-011-0576-0.
Chiu SC, Huang SY, Chen SP, Su CC, Chiu TL, Pang CY. Tanshinone IIA inhibits human prostate cancer cells growth by induction of endoplasmic reticulum stress in vitro and in vivo. Prostate Cancer Prostatic Dis 2013;16:315–22. https://doi.org/10.1038/pcan.2013.38.
Huang T, Yang X, Ji J, Wang Q, Wang H, Dong Z. Inhibitory effects of tanshinone IIA from Salvia miltiorrhiza Bge on human bladder cancer BIU-87 cells and xenograft in nude mice. Food Sci Technol 2020;40:209–14. https://doi.org/10.1590/fst.38818.
Nie Z-Y, Zhao M-H, Cheng B-Q, Pan R-F, Wang T-R, Qin Y, et al. Tanshinone IIA regulates human AML cell proliferation, cell cycle, and apoptosis through miR-497-5p/AKT3 axis. Cancer Cell Int 2020;20:379. https://doi.org/10.1186/s12935-020-01468-5.
Chiu T-L, Su C-C. Tanshinone IIA induces apoptosis in human lung cancer A549 cells through the induction of reactive oxygen species and decreasing the mitochondrial membrane potential. Int J Mol Med 2010;25:231–6.
Huang S-T, Huang C-C, Huang W-L, Lin T-K, Liao P-L, Wang P-W, et al. Tanshinone IIA induces intrinsic apoptosis in osteosarcoma cells both in vivo and in vitro associated with mitochondrial dysfunction. Sci Rep 2017;7:40382. https://doi.org/10.1038/srep40382.
Liu C, Li J, Wang L, Wu F, Huang L, Xu Y, et al. Analysis of tanshinone IIA induced cellular apoptosis in leukemia cells by genome-wide expression profiling. BMC Complement Altern Med 2012;12:5. https://doi.org/10.1186/1472-6882-12-5.
Cheng C-Y, Su C-C. Tanshinone IIA may inhibit the growth of small cell lung cancer H146 cells by up-regulating the Bax/Bcl-2 ratio and decreasing mitochondrial membrane potential. Mol Med Rep 2010;3:645–50. https://doi.org/10.3892/mmr_00000310.
Chiu T-L, Su CC. Tanshinone IIA increases protein expression levels of PERK, ATF6, IRE1α, CHOP, caspase-3 and caspase-12 in pancreatic cancer BxPC-3 cell-derived xenograft tumors. Mol Med Rep 2017;15:3259–63. https://doi.org/10.3892/mmr.2017.6359.
Su C-C, Chen G-W, Kang J-C, Chan M-H. Growth inhibition and apoptosis induction by tanshinone IIA in human colon adenocarcinoma cells. Planta Med 2008;74:1357–62. https://doi.org/10.1055/s-2008-1081299.
Chiu S-C, Huang S-Y, Chang S-F, Chen S-P, Chen C-C, Lin T-H, et al. Potential Therapeutic Roles of Tanshinone IIA in Human Bladder Cancer Cells. Int J Mol Sci 2014;15:15622–37. https://doi.org/10.3390/ijms150915622.
He L, Gu K. Tanshinone IIA regulates colorectal cancer apoptosis via attenuation of Parkin‑mediated mitophagy by suppressing AMPK/Skp2 pathways. Mol Med Rep 2018; 18(2):1692-1703. https://doi.org/10.3892/mmr.2018.9087.
Liu Z, Zhu W, Kong X, Chen X, Sun X, Zhang W, et al. Tanshinone IIA inhibits glucose metabolism leading to apoptosis in cervical cancer. Oncol Rep. 2019;42(5):1893–1903. https://doi.org/10.3892/or.2019.7294.
Jieensinue S, Zhu H, Li G, Dong K, Liang M, Li Y. Tanshinone IIA reduces SW837 colorectal cancer cell viability via the promotion of mitochondrial fission by activating JNK-Mff signaling pathways. BMC Cell Biol. 2018;19:21. https://doi.org/10.1186/s12860-018-0174-z.
Su C-C, Lin Y-H. Tanshinone IIA inhibits human breast cancer cells through increased Bax to Bcl-xL ratios. Int J Mol Med. 2008;22(3):357–61. https://doi.org/10.3892/ijmm_00000030.
Jung JH, Kwon T-R, Jeong S-J, Kim E-O, Sohn EJ, Yun M, et al. Apoptosis induced by tanshinone IIA and cryptotanshinone is mediated by distinct JAK/STAT3/5 and SHP1/2 signaling in chronic myeloid leukemia K562 cells. Evid Based Complement Alternat Med. 2013;2013:1–10. https://doi.org/10.1155/2013/805639.
Lin C-Y, Chang T-W, Hsieh W-H, Hung M-C, Lin I-H, Lai S-C, et al. Simultaneous induction of apoptosis and necroptosis by Tanshinone IIA in human hepatocellular carcinoma HepG2 cells. Cell Death Discov. 2016;2:16065. https://doi.org/10.1038/cddiscovery.2016.65.
Zhang X, Zhou Y, Gu Y-E. Tanshinone IIA induces apoptosis of ovarian cancer cells in vitro and in vivo through attenuation of PI3K/AKT/JNK signaling pathways. Oncol Lett. 2019;17:1896–902. https://doi.org/10.3892/ol.2018.9744.
Qiu Y, Li C, Wang Q, Zeng X, Ji P. Tanshinone IIA induces cell death via Beclin-1-dependent autophagy in oral squamous cell carcinoma SCC-9 cell line. Cancer Med. 2018;7:397–407. https://doi.org/10.1002/cam4.1281.
Yun S-M, Jeong S-J, Kim J-H, Jung JH, Lee H-J, Sohn EJ, et al. Activation of c-Jun N-terminal kinase mediates tanshinone IIA-induced apoptosis in KBM-5 chronic myeloid leukemia cells. Biol Pharm Bull. 2013;36:208–14. https://doi.org/10.1248/bpb.b12-00537.
Li G, Shan C, Liu L, Zhou T, Zhou J, Hu X, et al. Tanshinone IIA inhibits HIF-1α and VEGF expression in breast cancer cells via mTOR/p70S6K/RPS6/4E-BP1 signaling pathway. PLOS ONE 2015;10:e0117440. https://doi.org/10.1371/journal.pone.0117440.
Sui H, Zhao J, Zhou L, Wen H, Deng W, Li C, et al. Tanshinone IIA inhibits β-catenin/VEGF-mediated angiogenesis by targeting TGF-β1 in normoxic and HIF-1α in hypoxic microenvironments in human colorectal cancer. Cancer Lett. 2017;403:86–97. https://doi.org/10.1016/j.canlet.2017.05.013.
Shan Y, Shen X, Xie Y, Chen J, Shi H, Yu Z, et al. Inhibitory effects of tanshinone II-A on invasion and metastasis of human colon carcinoma cells. Acta Pharmacol Sin. 2009;30:1537–42. https://doi.org/10.1038/aps.2009.139.
Yu J, Wang X, Li Y, Tang B. Tanshinone IIA suppresses gastric cancer cell proliferation and migration by downregulation of FOXM1. Oncol Rep. 2017;37:1394–400. https://doi.org/10.3892/or.2017.5408.
Cao Y, Wang S, Li X, Zhang Y, Qiao Y. The anticancer mechanism investigation of Tanshinone IIA by pharmacological clustering in protein network. BMC Syst Biol. 2018;12:90. https://doi.org/10.1186/s12918-018-0606-6.
Naz I, Merarchi M, Ramchandani S, Khan MR, Malik MN, Sarwar S, et al. An overview of the anti-cancer actions of Tanshinones, derived from Salvia miltiorrhiza (Danshen). Explor Target Anti-Tumor Ther. 2020;1. https://doi.org/10.37349/etat.2020.00010.
Jingwen B, Yaochen L, Guojun Z. Cell cycle regulation and anticancer drug discovery. Cancer Biol Med. 2017;14:348. https://doi.org/10.20892/j.issn.2095-3941.2017.0033
Liao X, Gao Y, Huang S, Chen Z, Sun L, Liu J, et al. Tanshinone IIA combined with cisplatin synergistically inhibits non‐small‐cell lung cancer in vitro and in vivo via down‐regulating the phosphatidylinositol 3‐kinase/Akt signalling pathway. Phytother Res. 2019;33:2298–309. https://doi.org/10.1002/ptr.6392.
Wei X, Zhou L, Hu L, Huang Y. Tanshinone IIA arrests cell cycle and induces apoptosis in 786-O human renal cell carcinoma cells. Oncol Lett. 2012;3:1144–8. https://doi.org/10.3892/ol.2012.626.
Xie J, Liu J-H, Liu H, Liao X-Z, Chen Y, Lin M-G, et al. Tanshinone IIA combined with adriamycin inhibited malignant biological behaviors of NSCLC A549 cell line in a synergistic way. BMC Cancer 2016;16:899. https://doi.org/10.1186/s12885-016-2921-x.
Pan T-L, Hung Y-C, Wang P-W, Chen S-T, Hsu T-K, Sintupisut N, et al. Functional proteomic and structural insights into molecular targets related to the growth inhibitory effect of tanshinone IIA on HeLa cells. Proteomics 2010;10:914–29. https://doi.org/10.1002/pmic.200900178.
Zhou L, Chan WK, Xu N, Xiao K, Luo H, Luo KQ, et al. Tanshinone IIA, an isolated compound from Salvia miltiorrhiza Bunge, induces apoptosis in HeLa cells through mitotic arrest. Life Sci. 2008;83:394–403. https://doi.org/10.1016/j.lfs.2008.07.011
Xu M, Cao F-L, Li N-Y, Liu Y-Q, Li Y-P, Lv C-L. Tanshinone IIA reverses the malignant phenotype of SGC7901 gastric cancer cells. Asian Pac J Cancer Prev. 2013;14:173–7. https://doi.org/10.7314/APJCP.2013.14.1.173.
Wang J, Wang X, Jiang S, Yuan S, Lin P, Zhang J, et al. Growth inhibition and induction of apoptosis and differentiation of tanshinone IIA in human glioma cells. J Neurooncol. 2007;82:11–21. https://doi.org/10.1007/s11060-006-9242-x.
Yan M-Y, Chien S-Y, Kuo S-J, Chen D-R, Su C-C. Tanshinone IIA inhibits BT-20 human breast cancer cell proliferation through increasing caspase 12, GADD153 and phospho-p38 protein expression. Int J Mol Med. 2012;29:855–63. https://doi.org/10.3892/ijmm.2012.908.
Ma Z-L, Zhang B-J, Wang D-T, Li X, Wei J-L, Zhao B-T, et al. Tanshinones suppress AURKA through up-regulation of miR-32 expression in non-small cell lung cancer. Oncotarget 2015;6:20111–20. https://doi.org/10.18632/oncotarget.3933.
Zhang Y, Jiang P, Ye M, Kim S-H, Jiang C, Lü J. Tanshinones: sources, pharmacokinetics and anti-cancer activities. Int J Mol Sci. 2012;13:13621–66. https://doi.org/10.3390/ijms131013621.
Pencik J, Pham HTT, Schmoellerl J, Javaheri T, Schlederer M, Culig Z, et al. JAK-STAT signaling in cancer: from cytokines to non-coding genome. Cytokine 2016;87:26–36. https://doi.org/10.1016/j.cyto.2016.06.017.
Zhang Y, Guo S, Fang J, Peng B, Zhang Y, Cao T. Tanshinone IIA inhibits cell proliferation and tumor growth by downregulating STAT3 in human gastric cancer. Exp Ther Med 2018. https://doi.org/10.3892/etm.2018.6562.
Brahmkhatri VP, Prasanna C, Atreya HS. Insulin-like growth factor system in cancer: novel targeted therapies. BioMed Res Int. 2015;2015:1–24. https://doi.org/10.1155/2015/538019.
Fernández MC, Venara M, Nowicki S, Chemes HE, Barontini M, Pennisi PA. IGF-I regulates pheochromocytoma cell proliferation and survival in vitro and in vivo. Endocrinology 2012;153:3724–34. https://doi.org/10.1210/en.2012-1107.
Lönn S, Inskip PD, Pollak MN, Weinstein SJ, Virtamo J, Albanes D. Glioma risk in relation to serum levels of insulin-like growth factors. Cancer Epidemiol Biomarkers Prev. 2007;16:844–6. https://doi.org/10.1158/1055-9965.EPI-06-1010.
Wang H, Su X, Fang J, Xin X, Zhao X, Gaur U, et al. Tanshinone IIA attenuates insulin like growth factor 1-induced cell proliferation in PC12 cells through the PI3K/Akt and MEK/ERK pathways. Int J Mol Sci. 2018;19:2719. https://doi.org/10.3390/ijms19092719.
Baig S, Seevasant I, Mohamad J, Mukheem A, Huri HZ, Kamarul T. Potential of apoptotic pathway-targeted cancer therapeutic research: Where do we stand? Cell Death Dis. 2016;7:e2058. https://doi.org/10.1038/cddis.2015.275.
Zhang Y, Li S, He H, Han Q, Wang B, Zhu Y. Influence of Tanshinone IIA on apoptosis of human esophageal carcinoma Eca-109 cells and its molecular mechanism. Thorac Cancer 2017;8:296–303. https://doi.org/10.1111/1759-7714.12441.
Ahmad I, Hoque M, Alam SSM, Zughaibi TA, Tabrez S. Curcumin and plumbagin synergistically target the PI3K/Akt/mTOR pathway: a prospective role in cancer treatment. Int J Mol Sci. 2023;24:6651. https://doi.org/10.3390/ijms24076651.
Lee H-P, Liu Y-C, Chen P-C, Tai H-C, Li T-M, Fong Y-C, et al. Tanshinone IIA inhibits angiogenesis in human endothelial progenitor cells in vitro and in vivo. Oncotarget 2017;8:109217–27. https://doi.org/10.18632/oncotarget.22649.
Shimizu S, Yoshida T, Tsujioka M, Arakawa S. Autophagic cell death and cancer. Int J Mol Sci. 2014;15:3145–53. https://doi.org/10.3390/ijms15023145.
Chen H, Liu RH. Potential mechanisms of action of dietary phytochemicals for cancer prevention by targeting cellular signaling transduction pathways. J Agric Food Chem. 2018;66:3260–76. https://doi.org/10.1021/acs.jafc.7b04975.
Jamil Z, Uddin A, Alam SSM, Samanta A, Altwaijry N, Rauf MA, et al. Analysis of the compositional features and codon usage pattern of genes involved in human autophagy. Cells 2022;11:3203. https://doi.org/10.3390/cells11203203.
Usman RM, Razzaq F, Akbar A, Farooqui AA, Iftikhar A, Latif A, et al. Role and mechanism of autophagy‐regulating factors in tumorigenesis and drug resistance. Asia Pac J Clin Oncol. 2021;17:193–208. https://doi.org/10.1111/ajco.13449.
Jung CH, Ro S-H, Cao J, Otto NM, Kim D-H. mTOR regulation of autophagy. FEBS Lett. 2010;584:1287–95. https://doi.org/10.1016/j.febslet.2010.01.017.
Iwamaru A, Kondo Y, Iwado E, Aoki H, Fujiwara K, Yokoyama T, et al. Silencing mammalian target of rapamycin signaling by small interfering RNA enhances rapamycin-induced autophagy in malignant glioma cells. Oncogene 2007;26:1840–51. https://doi.org/10.1038/sj.onc.1209992.
Sohn EJ, Park HT. Natural agents mediated autophagic signal networks in cancer. Cancer Cell Int. 2017;17:110. https://doi.org/10.1186/s12935-017-0486-7.
Su C-C, Chien S-Y, Kuo S-J, Chen Y-L, Cheng C-Y, Chen D-R. Tanshinone IIA inhibits human breast cancer MDA-MB-231 cells by decreasing LC3-II, Erb-B2 and NF-κBp65. Mol Med Rep. 2012;5:1019–22. https://doi.org/10.3892/mmr.2012.756.
Yun S-M, Jung JH, Jeong S-J, Sohn EJ, Kim B, Kim S-H. Tanshinone IIA induces autophagic cell death via activation of AMPK and ERK and inhibition of mTOR and p70 S6K in KBM-5 leukemia cells: Tanshinone IIA induces autophagic cell death in KBM-5 cells. Phytother Res. 2014;28:458–64. https://doi.org/10.1002/ptr.5015.
Abuzenadah AM, Al-Sayes F, Mahafujul Alam SS, Hoque M, Karim S, Hussain IMR, et al. Elucidating antiangiogenic potential of Rauwolfia serpentina: VEGFR-2 targeting-based molecular docking study. Evid Based Complement Alternat Med. 2022;2022:1–10. https://doi.org/10.1155/2022/6224666.
Zhang Y, Wei R, Zhu X, Cai L, Jin W, Hu H. Tanshinone IIA induces apoptosis and inhibits the proliferation, migration, and invasion of the osteosarcoma MG-63 cell line in vitro. Anticancer Drugs 2012;23:212–9. https://doi.org/10.1097/CAD.0b013e32834e5592.
Dong W, Zhang Y, Chen X, Jia Y. High-dose Tanshinone IIA suppresses migration and proliferation while promoting apoptosis of astrocytoma cells via notch-1 pathway. Neurochem Res. 2018;43:1855–61. https://doi.org/10.1007/s11064-018-2601-0.
Su C-C. Abstract 3624: Tanshinone IIA could decrease programmed death ligand 1 expression in human breast cancer BT-20 cells. Cancer Res. 2018; 78:3624-3624. https://doi.org/10.1158/1538-7445.AM2018-3624.
Ding W-X, Yin X-M. Mitophagy: mechanisms, pathophysiological roles, and analysis. Biol Chem. 2012;393:547–64. https://doi.org/10.1515/hsz-2012-0119.
Jin X, Kim S-H, Jeon H-M, Beck S, Sohn Y-W, Yin J, et al. Interferon regulatory factor 7 regulates glioma stem cells via interleukin-6 and Notch signalling. Brain 2012;135:1055–69. https://doi.org/10.1093/brain/aws028.
Yang L, Guo H, Dong L, Wang L, Liu C, Wang X. Tanshinone IIA inhibits the growth, attenuates the stemness and induces the apoptosis of human glioma stem cells. Oncol Rep. 2014;32:1303–11. https://doi.org/10.3892/or.2014.3293.
Lin C, Wang L, Wang H, Yang L, Guo H, Wang X. Tanshinone IIA inhibits breast cancer stem cells growth in vitro and in vivo through attenuation of IL-6/STAT3/NF-kB signaling pathways: Tanshinone IIA Inhibits Breast CSCs Growth. J Cell Biochem 2013;114:2061–70. https://doi.org/10.1002/jcb.24553.
Li P, Li S-P, Yang F-Q, Wang Y-T. Simultaneous determination of four tanshinones insalvia miltiorrhiza by pressurized liquid extraction and capillary electrochromatography. J Sep Sci. 2007;30:900–5. https://doi.org/10.1002/jssc.200600368.
Ong ES, Len SM. Evaluation of pressurized liquid extraction and pressurized hot water extraction for tanshinone I and IIA in Salvia miltiorrhiza using LC and LC-ESI-MS. J Chromatogr Sci. 2004;42:211–6. https://doi.org/10.1093/chromsci/42.4.211.
Pan X, Niu G, Liu H. Microwave-assisted extraction of tanshinones from Salvia miltiorrhiza bunge with analysis by high-performance liquid chromatography. J Chromatogr A 2001;922:371–5. https://doi.org/10.1016/S0021-9673(01)00949-9.
Wang L, Song Y, Cheng Y, Liu X. Orthogonal array design for the optimization of supercritical fluid extraction of tanshinones from Danshen. J Sep Sci. 2008;31:321–8. https://doi.org/10.1002/jssc.200700386.
Ekins S, Mestres J, Testa B. In silico pharmacology for drug discovery: methods for virtual ligand screening and profiling: In silico pharmacology for drug discovery. Br J Pharmacol. 2007;152:9–20. https://doi.org/10.1038/sj.bjp.0707305.
Li M, Liu H, Zhao Q, Han S, Zhou L, Liu W, et al. Targeting Aurora B kinase with Tanshinone IIA suppresses tumor growth and overcomes radioresistance. Cell Death Dis. 2021;12:152. https://doi.org/10.1038/s41419-021-03434-z.
Xu X, Zhang Z, Liu L, Che C, Li W. Exploring the antiovarian cancer mechanisms of Salvia miltiorrhiza bunge by network pharmacological analysis and molecular docking. Comput Math. Methods Med. 2022;2022:1–12. https://doi.org/10.1155/2022/7895246.
Chen S-J. A potential target of Tanshinone IIA for acute promyelocytic leukemia revealed by inverse docking and drug repurposing. Asian Pac J Cancer Prev. 2014;15:4301–5. https://doi.org/10.7314/APJCP.2014.15.10.4301.
Kim E-O, Kang SE, Im CR, Lee J-H, Ahn KS, Yang WM, et al. Tanshinone IIA induces TRAIL sensitization of human lung cancer cells through selective ER stress induction. Int J Oncol. 2016;48:2205–12. https://doi.org/10.3892/ijo.2016.3441.
Wang R, Luo Z, Zhang H, Wang T. Tanshinone IIA reverses gefitinib-resistance in human non-small-cell lung cancer via regulation of VEGFR/Akt pathway. OncoTargets Ther. 2019;12:9355–65. https://doi.org/10.2147/OTT.S221228.
Bi Z, Wang Y, Zhang W. A comprehensive review of tanshinone IIA and its derivatives in fibrosis treatment. Biomed Pharmacother. 2021;137:111404. https://doi.org/10.1016/j.biopha.2021.111404.
Gupta J, Safdari HA, Hoque M. Nanoparticle mediated cancer immunotherapy. Semin Cancer Biol. 2021;69:307–24. https://doi.org/10.1016/j.semcancer.2020.03.015.
Hoque M, Samanta A, Alam SSM, Zughaibi TA, Kamal MA, Tabrez S. Nanomedicine-based immunotherapy for Alzheimer’s disease. Neurosci Biobehav Rev. 2023;144:104973. https://doi.org/10.1016/j.neubiorev.2022.104973.
Acknowledgements
The authors gratefully acknowledge the Department of Biological Sciences at Aliah University in Kolkata, India, for providing essential research facilities. SSMA sincerely acknowledges the Council of Scientific and Industrial Research (CSIR), Government of India for financial help in the form of a Junior Research Fellowship (JRF).
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
SSMA, AS, and FU wrote portions of the initial draft of the paper and modified the draft. SSMA, AS, and MH contributed to the figures. SA and MH edited the draft of the paper and made final changes to the final version before submission. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there exists no competing interest.
Ethical approval
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alam, S.S.M., Samanta, A., Uddin, F. et al. Tanshinone IIA targeting cell signaling pathways: a plausible paradigm for cancer therapy. Pharmacol. Rep 75, 907–922 (2023). https://doi.org/10.1007/s43440-023-00507-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-023-00507-y