Abstract
Background and aim
This study evaluates a novel benzylidene-chromanone derivative, FNF-12, for efficacy in in vitro and in vivo asthma models.
Methods
Rat basophilic leukemia (RBL-2H3) and acute monocytic leukemia (THP-1)-derived M2 macrophages were used. Human whole blood-derived neutrophils and basophils were employed. Flow cytometry was used for studying key signalling proteins. Platelet activation factor (PAF)-induced asthma model in guinea pigs was used for in vivo studies.
Results
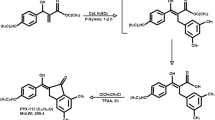
The chemical structure of FNF-12 was confirmed with proton-nuclear mass resonance (NMR) and mass spectroscopy. FNF-12 controlled degranulation in RBL-2H3 cells with an IC50 value of 123.7 nM and inhibited TNF-α release from these cells in a dose-responsive way. The compound effectively controlled the migration and elastase release in activated neutrophils. IC50 value in the FcεRI-basophil activation assay was found to be 205 nM. FNF-12 controlled the release of lipopolysaccharide (LPS)-induced interleukin-10, I-309/CCL1 and MDC/CCL22 in THP-1 derived M2 macrophages. The compound suppressed LPS-induced mitogen activated protein kinase (MAPK)-p-p38 and nuclear factor kappa B(NF-kB)-p-p65 expression in these cells. A dose-dependent decrease in the accumulation of total leucocytes, eosinophils, neutrophils and macrophages was observed in PAF-induced animal models.
Conclusion
FNF-12 was able to control the inflammatory responses in in vitro and in vivo asthma models, which may be driven by controlling M2-related Th2 cytokines via MAPK and NF-kB signaling.
Graphic abstract










Similar content being viewed by others
Abbreviations
- ACD solution:
-
Citrate–dextrose solution
- Avidin–HRP:
-
Avidin–horseradish peroxidase
- BAL:
-
Bronchoalveolar lavage
- DMSO:
-
Dimethylsulphoxide
- DNP–BSA:
-
2,4-Dinitrophenol–bovine serum albumin
- ELISA:
-
Enzyme-linked immunosorbent assay
- EMEM:
-
Eagle's minimum essential medium
- fMLP:
-
N-Formyl-methionyl-leucyl-phenylalanine
- HBSS:
-
Hank’s balanced salt solution
- HWB:
-
Human whole blood
- IgE:
-
Immunoglobulin E
- LPS:
-
Lipopolysaccharide
- MAPK:
-
Mitogen-activated protein kinase
- MPO:
-
Myeloperoxidase
- MTT:
-
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyl-2H-tetrazolium bromide
- NF-kB:
-
Nuclear factor kappa B
- NMR:
-
Nuclear mass resonance
- PAF:
-
Platelet activation factor
- PBS:
-
Phosphate-buffered saline
- PE:
-
Phycoerythrin
- PIPES:
-
Ethanesulphonic acid
- RBL-2H3:
-
Rat basophilic leukemia
- THP-1:
-
Acute monocytic leukaemia
- TNF-α:
-
Tumor necrosis factor-α
References
Mizgerd JP. Lung infection—a public health priority. PLoS Med. 2006;3:e76.
Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–43.
Spannhake EW, Reddy SP, Jacoby DB, Yu XY, Saatian B, Tian J. Synergism between rhinovirus infection and oxidant pollutant exposure enhances airway epithelial cell cytokine production. Environ Health Perspect. 2002;110:665–70.
Edwards MR, Bartlett NW, Clarke D, Birrell M, Belvisi M, Johnston SL. Targeting the NF-kappaB pathway in asthma and chronic obstructive pulmonary disease. Pharmacol Ther. 2009;121:1–13.
Wenzel SE. Asthma: defining of the persistent adult phenotypes. Lancet. 2006;368:804–13.
Green RM, Custovic A, Sanderson G, Hunter J, Johnston SL, Woodcock A. Synergism between allergens and viruses and risk of hospital admission with asthma: case–control study. BMJ. 2002;324:763.
Athari SS. Targeting cell signaling in allergic asthma. Signal Transduct Target Ther. 2019;4:45.
Zhu L, Chen X, Chong L, Kong L, Wen S, Zhang H, et al. Adiponectin alleviates exacerbation of airway inflammation and oxidative stress in obesity-related asthma mice partly through AMPK signaling pathway. Int Immunopharmacol. 2019;67:396–407.
Catz SD, Johnson JL. Transcriptional regulation of bcl-2 by nuclear factor kappa B and its significance in prostate cancer. Oncogene. 2001;20:7342–51.
Ajuwon KM, Spurlock ME. Adiponectin inhibits LPS-induced NF-kappaB activation and IL-6 production and increases PPARgamma2 expression in adipocytes. Am J Physiol Regul Integr Comp Physiol. 2005;288:R1220–5.
Qiu YY, Wu Y, Lin MJ, Bian T, Xiao YL, Qin C. LncRNA-MEG3 functions as a competing endogenous RNA to regulate Treg/Th17 balance in patients with asthma by targeting microRNA-17/ RORγt. Biomedicine & pharmacotherapy (Biomedecine & pharmacotherapie). 2019;111:386–94.
Shieh YH, Huang HM, Ching-Chiung W, Lee CC, Fan CK, Lee YL. Corrigendum to “Zerumbone enhances the Th1 response and ameliorates ovalbumin-induced Th2 responses and airway inflammation in mice” [Int. Immunopharmacol. 24 (2015) 383-391]. Int Immunopharmacol. 2017;50:371.
Yuan F, Liu R, Hu M, Rong X, Bai L, Xu L, et al. JAX2, an ethanol extract of Hyssopus cuspidatus Boriss, can prevent bronchial asthma by inhibiting MAPK/NF-κB inflammatory signaling. Phytomed Int J phytother phytopharmacol. 2019;57:305–14.
Takao K, Yamashita M, Yashiro A, Sugita Y. Synthesis and biological evaluation of 3-benzylidene-4-chromanone derivatives as free radical scavengers and α-glucosidase inhibitors. Chem Pharm Bull. 2016;64:1203–7.
Livingstone R. Naturally occurring oxygen ring compounds. Nature. 1963;200:509.
Kabbe H-J, Widdig A. Synthesis and reactions of 4-chromanones. Angew Chem Int Ed Engl. 1982;21:247–56.
Dera A, Rajagopalan P. Thymoquinone attenuates phosphorylation of AKT to inhibit kidney cancer cell proliferation. J Food Biochem. 2019;43:e12793.
Naal RM, Tabb J, Holowka D, Baird B. In situ measurement of degranulation as a biosensor based on RBL-2H3 mast cells. Biosens Bioelectron. 2004;20:791–6.
Maqbool M, Vidyadaran S, George E, Ramasamy R. Optimisation of laboratory procedures for isolating human peripheral blood derived neutrophils. Med J Malays. 2011;66:296–9.
Craciun I, Fenner AM, Kerns RJ. N-Arylacyl O-sulfonated aminoglycosides as novel inhibitors of human neutrophil elastase, cathepsin G and proteinase 3. Glycobiology. 2016;26:701–9.
Dera A, Rajagopalan P, Ahmed I, Alfhili M, Alsughayyir J, Chandramoorthy HC. Thymoquinone attenuates IgE-mediated allergic response via pi3k-Akt-NFκB pathway and upregulation of the Nrf2-HO1 axis. J Food Biochem. 2020;44:e13216.
Chanput W, Mes JJ, Savelkoul HF, Wichers HJ. Characterization of polarized THP-1 macrophages and polarizing ability of LPS and food compounds. Food Funct. 2013;4:266–76.
Raju BC, Tiwari AK, Kumar JA, Ali AZ, Agawane SB, Saidachary G, et al. alpha-Glucosidase inhibitory antihyperglycemic activity of substituted chromenone derivatives. Bioorg Med Chem. 2010;18:358–65.
Das U, Lorand T, Dimmock SG, Perjesi P, Dimmock JR. 3-benzylidene-4-chromanones: a novel cluster of anti-tubercular agents. J Enzyme Inhib Med Chem. 2015;30:259–63.
Takao K, Yamashita M, Yashiro A, Sugita Y. Synthesis and biological evaluation of 3-benzylidene-4-chromanone derivatives as free radical scavengers and α-glucosidase inhibitors. Chem Pharm Bull (Tokyo). 2016;64:1203–7.
Noushini S, Alipour E, Emami S, Safavi M, Ardestani SK, Gohari AR, et al. Synthesis and cytotoxic properties of novel (E)-3-benzylidene-7-methoxychroman-4-one derivatives. Daru J Fac Pharm Tehran Univ Med Sci. 2013;21:31.
Méndez-Enríquez E, Hallgren J. Mast cells and their progenitors in allergic asthma. Front Immunol. 2019;10:821.
Cruse G, Bradding P. Mast cells in airway diseases and interstitial lung disease. Eur J Pharmacol. 2016;778:125–38.
Zhang H, Wang J, Wang L, Zhan M, Li S, Fang Z, et al. Induction of mast cell accumulation by chymase via an enzymatic activity- and intercellular adhesion molecule-1-dependent mechanism. Br J Pharmacol. 2018;175:678–92.
Radermecker C, Louis R, Bureau F, Marichal T. Role of neutrophils in allergic asthma. Curr Opin Immunol. 2018;54:28–34.
Radermecker C, Sabatel C, Vanwinge C, Ruscitti C, Maréchal P, Perin F, et al. Locally instructed CXCR4(hi) neutrophils trigger environment-driven allergic asthma through the release of neutrophil extracellular traps. Nat Immunol. 2019;20:1444–55.
Oliveira SH, Canetti C, Ribeiro RA, Cunha FQ. Neutrophil migration induced by IL-1beta depends upon LTB4 released by macrophages and upon TNF-alpha and IL-1beta released by mast cells. Inflammation. 2008;31:36–46.
Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3:23–35.
Melgert BN, ten Hacken NH, Rutgers B, Timens W, Postma DS, Hylkema MN. More alternative activation of macrophages in lungs of asthmatic patients. J Allergy Clin Immunol. 2011;127:831–3.
Lin YC, Huang MY, Lee MS, Hsieh CC, Kuo HF, Kuo CH, et al. Effects of montelukast on M2-related cytokine and chemokine in M2 macrophages. J Microbiol Immunol Infect. 2018;51:18–26.
Wu AY, Chik SC, Chan AW, Li Z, Tsang KW, Li W. Anti-inflammatory effects of high-dose montelukast in an animal model of acute asthma. Clin Exp Allergy. 2003;33:359–66.
Schuliga M. NF-kappaB signaling in chronic inflammatory airway disease. Biomolecules. 2015;5:1266–83.
Park EK, Jung HS, Yang HI, Yoo MC, Kim C, Kim KS. Optimized THP-1 differentiation is required for the detection of responses to weak stimuli. Inflamm Res. 2007;56:45–50.
Gagliardo R, Chanez P, Profita M, Bonanno A, Albano GD, Montalbano AM, et al. IκB kinase-driven nuclear factor-κB activation in patients with asthma and chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2011;128(635–45):e1-2.
Brown V, Elborn JS, Bradley J, Ennis M. Dysregulated apoptosis and NFkappaB expression in COPD subjects. Respir Res. 2009;10:24.
Tahan F, Jazrawi E, Moodley T, Rovati GE, Adcock IM. Montelukast inhibits tumour necrosis factor-alpha-mediated interleukin-8 expression through inhibition of nuclear factor-kappaB p65-associated histone acetyltransferase activity. Clin Exp Allergy. 2008;38:805–11.
Li YT, He B, Wang YZ, Wang J. Effects of intratracheal administration of nuclear factor-kappaB decoy oligodeoxynucleotides on long-term cigarette smoke-induced lung inflammation and pathology in mice. Respir Res. 2009;10:79.
Rajendrasozhan S, Hwang JW, Yao H, Kishore N, Rahman I. Anti-inflammatory effect of a selective IkappaB kinase-beta inhibitor in rat lung in response to LPS and cigarette smoke. Pulm Pharmacol Ther. 2010;23:172–81.
Dong C, Davis RJ, Flavell RA. MAP kinases in the immune response. Annu Rev Immunol. 2002;20:55–72.
Wong CK, Wang CB, Ip WK, Tian YP, Lam CW. Role of p38 MAPK and NF-kB for chemokine release in coculture of human eosinophils and bronchial epithelial cells. Clin Exp Immunol. 2005;139:90–100.
Barnes PJ. Kinases as novel therapeutic targets in asthma and chronic obstructive pulmonary disease. Pharmacol Rev. 2016;68:788–815.
Saccani S, Pantano S, Natoli G. p38-Dependent marking of inflammatory genes for increased NF-kappa B recruitment. Nat Immunol. 2002;3:69–75.
Kasperska-Zajac A, Brzoza Z, Rogala B. Platelet-activating factor (PAF): a review of its role in asthma and clinical efficacy of PAF antagonists in the disease therapy. Recent Pat Inflamm Allergy Drug Discov. 2008;2:72–6.
Tsukioka K, Matsuzaki M, Nakamata M, Kayahara H, Nakagawa T. Increased plasma level of platelet-activating factor (PAF) and decreased serum PAF acetylhydrolase (PAFAH) activity in adults with bronchial asthma. J Investig Allergol Clin Immunol. 1996;6:22–9.
Kuijpers TW, van den Berg JM, Tool AT, Roos D. The impact of platelet-activating factor (PAF)-like mediators on the functional activity of neutrophils: anti-inflammatory effects of human PAF-acetylhydrolase. Clin Exp Immunol. 2001;123:412–20.
Stafforini DM. PAF acetylhydrolase gene polymorphisms and asthma severity. Pharmacogenomics. 2001;2:163–75.
Sanjar S, Aoki S, Boubekeur K, Burrows L, Colditz I, Chapman I, et al. Inhibition of PAF-induced eosinophil accumulation in pulmonary airways of guinea pigs by anti-asthma drugs. Jpn J Pharmacol. 1989;51:167–72.
Bruijnzeel PL, Rihs S, Virchow JC Jr, Warringa RA, Moser R, Walker C. Early activation or “priming” of eosinophils in asthma. Schweizerische medizinische Wochenschrift. 1992;122:298–301.
Ilmarinen P, Kankaanranta H. Eosinophil apoptosis as a therapeutic target in allergic asthma. Basic Clin Pharmacol Toxicol. 2014;114:109–17.
Yang L, Cohn L, Zhang DH, Homer R, Ray A, Ray P. Essential role of nuclear factor kappaB in the induction of eosinophilia in allergic airway inflammation. J Exp Med. 1998;188:1739–50.
Donovan CE, Mark DA, He HZ, Liou HC, Kobzik L, Wang Y, et al. NF-kappa B/Rel transcription factors: c-Rel promotes airway hyperresponsiveness and allergic pulmonary inflammation. J Immunol (Baltimore, Md: 1950). 1999;163:6827–33.
Acknowledgements
The authors express their gratitude to SMARTBIO LABS, Chennai, Tamil Nadu, India, for the help rendered in this study.
Funding
The authors extend their thanks to the Deanship of Scientific Research at King Khalid University, Abha, Saudi Arabia, for funding this work through Grant number RGP. 1/265/42.
Author information
Authors and Affiliations
Contributions
MA—funding, experimental, data curing. MAS—data analysis, statistical analysis, experimental. MYA—experimental, manuscript preparation. NB—data analysis, revision of manuscript. SR—experimental, data analysis, reference management. PR—conceptional design, data analysis, manuscript finalization, supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abohassan, M., Al Shahrani, M., Alshahrani, M.Y. et al. FNF-12, a novel benzylidene-chromanone derivative, attenuates inflammatory response in in vitro and in vivo asthma models mediated by M2-related Th2 cytokines via MAPK and NF-kB signaling. Pharmacol. Rep 74, 96–110 (2022). https://doi.org/10.1007/s43440-021-00325-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-021-00325-0