Abstract
Background
Metabolic bone disease and fractures are a great problem for patients with epilepsy. The use of antiepileptic drugs (AEDs) is known to play an essential role in the progression of bone loss by various pathophysiological mechanisms. The aim of this study was to evaluate the effects of AEDs on bone microstructure as an additional cause of an increased fracture risk in patients with epilepsy.
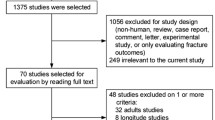
Methods
Five groups of each of 12 female rats were orally dosed daily for 8 weeks with either carbamazepine (CBZ) (60 mg/kg), eslicarbazepine (ESL) (80 mg/kg), valproic acid (VPA) (300 mg/kg), levetiracetam (LEV) (50 mg/kg) or saline (control (CTL)). Following killing, dissected femurs were analyzed using X-ray micro-computed tomography (µCT), dual-energy X-ray absorptiometry (DXA) and biomechanical testing. In addition, serum bone turnover markers (BTM) were monitored throughout the experiment.
Results
Compared to CTL treatment, VPA decreased bone volume fraction by 19%, decreased apparent density by 14% and increased structural model index by 41%. No changes were observed in bone biomechanics nor mineral density evaluated by DXA or in levels of BTM.
Conclusions
Our findings suggest that VPA affects the microarchitectural properties of the bone. The AEDs CBZ, ESL and LEV appear to have less adverse effects on bone biology and may be a better choice when treating patients with respect to bone health.




Similar content being viewed by others
References
Fedorenko M, Wagner ML, Wu BY. Survey of risk factors for osteoporosis and osteoprotective behaviors among patients with epilepsy. Epilepsy Behav. 2015;45:1–6. https://doi.org/10.1016/j.yebeh.2015.01.021.
Svalheim S, Røste LS, Nakken KO, Taubøll E. Bone health in adults with epilepsy. Acta Neurol Scand Suppl. 2011;124:89–95. https://doi.org/10.1111/j.1600-0404.2011.01551.x.
Jetté N, Lix LM, Metge CJ, Prior HJ, McChesney J, Leslie WD. Association of antiepileptic drugs with nontraumatic fractures: a population-based analysis. Arch Neurol. 2011;68:107–12. https://doi.org/10.1001/archneurol.2010.341.
Vestergaard P, Tigaran S, Rejnmark L, Tigaran C, Dam M, Mosekilde L. Fracture risk is increased in epilepsy. Acta Neurol Scand. 1999;99:269–75. https://doi.org/10.1111/j.1600-0404.1999.tb00675.x.
Darba J, Kaskens L, Perez-Alvarez N, Palacios S, Neyro JL, Rejas J. Disability-adjusted-life-years losses in postmenopausal women with osteoporosis: a burden of illness study. BMC Public Health. 2015;15:324. https://doi.org/10.1186/s12889-015-1684-7.
Carbone LD, Johnson KC, Robbins J, Larson JC, Curb JD, Watson K, et al. Antiepileptic drug use, falls, fractures, and BMD in postmenopausal women: findings from the Women’s Health Initiative (WHI). J Bone Miner Res. 2010;25:873–81. https://doi.org/10.1359/jbmr.091027.
Souverein PC, Webb DJ, Weil JG, Van Staa TP, Egberts ACG. Use of antiepileptic drugs and risk of fractures—case–control study among patients with epilepsy. Neurology. 2006;66:1318–24.
Schelleman H, Pollard JR, Newcomb C, Markowitz CE, Bilker WB, Leonard MB, et al. Exposure to CYP3A4-inducing and CYP3A4-non-inducing antiepileptic agents and the risk of fractures. Pharmacoepidemiol Drug Saf. 2011;20:619–25. https://doi.org/10.1002/pds.2141.
Hahn TJ, Halstead LR. Anticonvulsant drug-induced osteomalacia: alterations in mineral metabolism and response to vitamin D3 administration. Calcif Tissue Int. 1979;27:13–8. https://doi.org/10.1007/BF02441155.
Hahn TJ. Bone complications of anticonvulsants. Drugs. 1976;12:201–11. https://doi.org/10.2165/00003495-197612030-00003.
Teagarden DL, Meador KJ, Loring DW. Low vitamin D levels are common in patients with epilepsy. Epilepsy Res. 2014;108:1352–6. https://doi.org/10.1016/j.eplepsyres.2014.06.008.
Kulak CAM, Borba VZC, Bilezikian JP, Silvado CE, De Paola L, Boguszewski CL. Bone mineral density and serum levels of 25 OH vitamin D in chronic users of antiepileptic drugs. Arq Neuropsiquiatr. 2004;62:940–8. https://doi.org/10.1590/S0004-282X2004000600003.
Boluk A, Guzelipek M, Savli H, Temel I, Ozişik HI, Kaygusuz A. The effect of valproate on bone mineral density in adult epileptic patients. Pharmacol Res. 2004;50:93–7. https://doi.org/10.1016/j.phrs.2003.11.011.
El-Haggar SM, Mostafa TM, Allah HMS, Akef GH. Levetiracetam and lamotrigine effects as mono-and polytherapy on bone mineral density in epileptic patients. Arq Neuropsiquiatr. 2018;76:452–8. https://doi.org/10.1590/0004-282x20180068.
Vestergaard P. Epilepsy, osteoporosis and fracture risk—a meta-analysis. Acta Neurol Scand. 2005;112:277–86. https://doi.org/10.1111/j.1600-0404.2005.00474.x.
Herrera S, Diez-Perez A. Clinical experience with microindentation in vivo in humans. Bone. 2017;95:175–82. https://doi.org/10.1016/j.bone.2016.11.003.
Diez-Perez A, Güerri R, Nogues X, Cáceres E, Peñ MJ, Mellibovsky L, et al. Microindentation for in vivo measurement of bone tissue mechanical properties in humans. J Bone Miner Res. 2010;25:1877–85. https://doi.org/10.1002/jbmr.73.
Parveen B, Tiwari AK, Jain M, Pal S, Chattopadhyay N, Tripathi M, et al. The anti-epileptic drugs valproate, carbamazepine and levetiracetam cause bone loss and modulate Wnt inhibitors in normal and ovariectomised rats. Bone. 2018;113:57–67. https://doi.org/10.1016/j.bone.2018.05.011.
Nissen-Meyer LSH, Svalheim S, Taubøll E, Reppe S, Lekva T, Solberg LB, et al. Levetiracetam, phenytoin, and valproate act differently on rat bone mass, structure, and metabolism. Epilepsia. 2007;48:1850–60. https://doi.org/10.1111/j.1528-1167.2007.01176.x.
Chbili C, Hassine A, Laouani A, Amor SB, Nouira M, Ammou SB, et al. The relationship between pharmacokinetic parameters of carbamazepine and therapeutic response in epileptic patients. Arch Med Sci. 2017;13:353–60. https://doi.org/10.5114/aoms.2016.60090.
Ding M. Microarchitectural adaptations in aging and osteoarthrotic subchondral bone issues. Acta Orthop. 2010;81:1–53. https://doi.org/10.3109/17453671003619037.
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res. 2010;25:1468–86. https://doi.org/10.1002/jbmr.141.
Humphrey EL, Morris GE, Fuller HR. Valproate reduces collagen and osteonectin in cultured bone cells. Epilepsy Res. 2013;106:446–50. https://doi.org/10.1016/j.eplepsyres.2013.06.011.
Schroeder TM, Westendorf JJ. Histone deacetylase inhibitors promote osteoblast maturation. J Bone Miner Res. 2005;20:2254–63. https://doi.org/10.1359/JBMR.050813.
Schroeder TM, Nair AK, Staggs R, Lamblin A-F, Westendorf JJ. Gene profile analysis of osteoblast genes differentially regulated by histone deacetylase inhibitors. BMC Genom. 2007;8:362. https://doi.org/10.1186/1471-2164-8-362.
Gold PW, Pavlatou MG, Michelson D, Mouro CM, Kling MA, Wong ML, et al. Chronic administration of anticonvulsants but not antidepressants impairs bone strength: clinical implications. Transl Psychiatry. 2015;5:e576. https://doi.org/10.1038/tp.2015.38.
Pack AM, Olarte LS, Morrell MJ, Flaster E, Resor SR, Shane E. Bone mineral density in an outpatient population receiving enzyme-inducing antiepileptic drugs. Epilepsy Behav. 2003;4:169–74. https://doi.org/10.1016/S1525-5050(03)00036-2.
Ohta T, Wergedal JE, Gruber HE, Baylink DJ, William Lau KH. Low dose phenytoin is an osteogenic agent in the rat. Calcif Tissue Int. 1995;56:42–8. https://doi.org/10.1007/BF00298743.
Abou-Khalil B, Schaich L. Long-term efficacy of levetiracetam for partial seizures. Seizure. 2005;14:577–85.
Karesova I, Simko J, Fekete S, Zimcikova E, Malakova J, Zivna H, et al. The effect of levetiracetam on rat bone mineral density, bone structure and biochemical markers of bone metabolism. Eur J Pharmacol. 2018;824:115–9. https://doi.org/10.1016/j.ejphar.2018.02.010.
Kanda J, Izumo N, Kobayashi Y, Onodera K, Shimakura T, Yamamoto N, et al. Effects of the antiepileptic drugs phenytoin, gabapentin, and levetiracetam on bone strength, bone mass, and bone turnover in rats. Biol Pharm Bull. 2017;40:1934–40.
Fekete S, Simko J, Gradosova I, Malakova J, Zivna H, Palicka V, et al. The effect of levetiracetam on rat bone mass, structure and metabolism. Epilepsy Res. 2013;107:56–60. https://doi.org/10.1016/j.eplepsyres.2013.08.012.
Jayo MJ, Register TC, Hughes CL, Blas-Machado U, Sulistiawati E, Borgerink H, et al. Effects of an oral contraceptive combination with or without androgen on mammary tissues: a study in rats. J Soc Gynecol Investig. 2000;7:257–65. https://doi.org/10.1016/S1071-5576(00)00059-9.
Hansson L, Menander-Sellman K, Stenström A, Thorngren K. Rate of normal longitudinal bone growth in the rat. Calcif Tissue Res. 1972;10:238–51.
Smith S, Varela A, Samadfam R, editors. Bone toxicology. 1st ed. Berlin: Springer; 2017.
McHugh J, Delanty N. Epidemiology and classification of epilepst: gender comparisons. Int Rev Neurobiol. 2008;83:11–6.
Pack AM, Morrell MJ, Randall A, Mcmahon DJ, Shane E. Bone health in young women with epilepsy after 1 year of antiepileptic drug monotherapy. Neurology. 2008. https://doi.org/10.1212/01.wnl.0000310981.44676.de.
Ensrud KE, Walczak TS, Blackwell T, Ensrud ER, Bowman PJ, Stone KL. Antiepileptic drug use increases rates of bone loss in older women—a prospective study. Neurology. 2004;62:2051–7.
Ensrud KE, Walczak TS, Blackwell TL, Ensrud ER, Barrett-Connor E, Orwoll ES. Antiepileptic drug use and rates of hip bone loss in older men: a prospective study. Neurology. 2008;71:723–30. https://doi.org/10.1212/01.wnl.0000324919.86696.a9.
Välimäki MJ, Tiihonen M, Laitinen K, Tähtelä R, Kärkkäinen M, Lamberg-Allardt C, et al. Bone mineral density measured by dual-energy X-ray absorptiometry and novel markers of bone formation and resorption in patients on antiepileptic drugs. J Bone Miner Res. 1994;9:631–7.
Sato Y, Kondo I, Ishida S, Motooka H, Takayama K, Tomita Y, et al. Decreased bone mass and increased bone turnover with valproate therapy in adults with epilepsy. Neurology. 2001;57:445–9.
Beniczky SA, Viken J, Jensen LT, Andersen NB. Bone mineral density in adult patients treated with various antiepileptic drugs. Seizure. 2012;21:471–2. https://doi.org/10.1016/j.seizure.2012.04.002.
Kobau R, DiIorio CA, Price PH, Thurman DJ, Martin LM, Ridings DL, et al. Prevalence of epilepsy and health status of adults with epilepsy in Georgia and Tennessee: behavioral risk factor surveillance system, 2002. Epilepsy Behav. 2004;5:358–66. https://doi.org/10.1016/j.yebeh.2004.02.007.
Elliott JO, Jacobson MP. Bone loss in epilepsy: barriers to prevention, diagnosis, and treatment. Epilepsy Behav. 2006;8:169–75. https://doi.org/10.1016/j.yebeh.2005.08.013.
El-Hajj Fuleihan G, Dib L, Yamout B, Sawaya R, Mikati MA. Predictors of bone density in ambulatory patients on antiepileptic drugs. Bone. 2008;43:149–55. https://doi.org/10.1016/j.bone.2008.03.002.
Bin JH, Kim G, Chung SY. Effect of antiepileptic drugs on bone mineral density in pediatric epilepsy patients. Eur J Paediatr Neurol. 2017;21:e41. https://doi.org/10.1016/j.ejpn.2017.04.824.
Chavassieux P, Seeman E, Delmas PD. Insights into material and structural basis of bone fragility from diseases associated with fractures: how determinants of the biomechanical properties of bone are compromised by disease. Endocr Rev. 2007;28:151–64. https://doi.org/10.1210/er.2006-0029.
Acknowledgements
The authors specially thank Tanja Hegner and Katja Serena for taking care of the animals and Kira Joensen and Britt Lisette Corfixen for analyzing the samples.
Funding
The study has been funded by an unrestricted educational grant from Eisai Co, Ltd and grants from the Jascha Foundation and the A. P. Møller Foundation, Fonden til Lægevidenskabens Fremme. The sponsors had no role in study design, collection of data, analysis or interpretation of data.
Author information
Authors and Affiliations
Contributions
Concept and design of the study: SSD, ASS, PE, NBA, NRJ. Conducting experiments: SSD, ME, MD. Analyzing and interpreting data: SSD, ASS, PE, ME, MD, NBA, NRJ. Writing, critically reviewing and approving the manuscript: SSD, ASS, PE, ME, MD, NBA, NRJ.
Corresponding author
Ethics declarations
Conflict of interest
SSD has received unrestricted research grants from Eisai Co, Ltd. A-SS has since the initiation of the work been employed by Novo Nordisk A/S. NRJ, ME, and MD have no conflicts of interest to disclose. PE is an advisory board member for Amgen Inc. and Eli Lilly A/S, and on the speakers’ bureau for Amgen Inc. and Eli Lilly A/S, and own shares in Novo Nordisk A/S. NBA is a lecturer at scientific meetings organized by Eisai Co, Ltd, and has received unrestricted research grants from Eisai Co, Ltd.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Diemar, S.S., Sejling, AS., Eiken, P. et al. Effects of carbamazepine, eslicarbazepine, valproic acid and levetiracetam on bone microarchitecture in rats. Pharmacol. Rep 72, 1323–1333 (2020). https://doi.org/10.1007/s43440-020-00087-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-020-00087-1