Abstract
Purpose
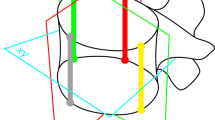
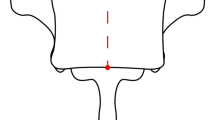
Scoliosis can be treated with vertebral body tethering (VBT) as a motion-sparing procedure. However, the knowledge of how growth is affected by a tether spanning multiple levels is unclear in the literature. Three-dimensional true spine length (3D-TSL) is a validated assessment technique that accounts for the shape of the spine in both the coronal and sagittal planes. This study aimed to assess if 3D-TSL increases over a five-year period after VBT implantation in thoracic curves for idiopathic scoliosis.
Methods
Prospectively collected radiographic data from an international pediatric spine registry was analyzed. Complete radiographic data over three visits (post-operative, 2 years, and 5 years) was available for 53 patients who underwent VBT.
Results
The mean age at instrumentation of this cohort was 12.2 (9–15) years. The average number of vertebrae instrumented was 7.3 (SD 0.7). Maximum Cobb angles were 50° pre-op, which improved to 26° post-op (p < 0.001) and was maintained at 5 years (30°; p = 0.543). Instrumented Cobb angle was 22° at 5 years (p < 0.001 vs 5-year maximum Cobb angle). An accentuation was seen in global kyphosis from 29° pre-operative to 41° at 5 years (p < 0.05). The global spine length (T1-S1 3D-TSL) started at 40.6 cm; measured 42.8 cm at 2 years; and 44.0 cm at the final visit (all p < 0.05). At 5 years, patients reached an average T1-S1 length that is comparable to a normal population at maturity. Immediate mean post-operative instrumented 3D-TSL (top of UIV–top of LIV) was 13.8 cm two-year length was 14.3 cm; and five-year length was 14.6 cm (all p < 0.05). The mean growth of 0.09 cm per instrumented level at 2 years was approximately 50% of normal thoracic growth. Patients who grew more than 0.5 cm at 2 years had a significantly lower BMI (17.0 vs 19.0, p < 0.05) and smaller pre-operative scoliosis (48° vs 53°, p < 0.05). Other subgroup analyses were not significant for age, skeletal maturity, Cobb angles or number of spanned vertebras as contributing factors.
Conclusions
This series demonstrates that 3D-TSL increased significantly over the thoracic instrumented levels after VBT surgery for idiopathic scoliosis. This represented approximately 50% of expected normal thoracic growth over 2 years.




Similar content being viewed by others
Data availability
Registry data is available to member institutions. Measurements and analysis done at the IWK Health Centre are on a password-protected server. Access may be arranged through an application to the REB.
Code availability
Statistical analysis was conducted using Excel version 16.63.1 (Microsoft Corporation, Redmond, Washington, USA) and SPSS version 28.0.1.1 (IBM Corp, Armonk, NY, USA).
References
Cobb JR (1948) Outline for the study of scoliosis. In: Arbor A (ed) Instructional course lectures. The American academy of orthopaedic surgeons. JW Edwards Publishing Co., pp 261–275
Bunnell WP (1988) The natural history of idiopathic scoliosis. Clin Orthop Relat Res 229:20–25
Weinstein SL, Ponseti I (1983) Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 65:4475
Charles YP, Daures JP, de Rosa V et al (2006) Progression risk of idiopathic juvenile scoliosis during pubertal growth. Spine 31:1933e42
Kepler CK, Meredith DS, Green DW, Widmann RF (2012) Long-term outcomes after posterior spine fusion for adolescent idiopathic scoliosis. Curr Opin Pediatr 24(1):68–75. https://doi.org/10.1097/MOP.0b013e32834ec982
Green DW, Lawhorne TW, Widmann RF, Kepler CK, Ahern C, Mintz DN, Rawlins BA, Burke SW, Boachie-Adjei O (2011) Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 36(23):1948–1954. https://doi.org/10.1097/BRS.0b013e3181ff1ea9
Skaggs DL, Akbarnia BA, Flynn JM, Myung KS, Sponseller PD, Vitale MG, Chest Wall and Spine Deformity Study Group, Growing Spine Study Group, Pediatric Orthopaedic Society of North America, Scoliosis Research Society Growing Spine Study Committee (2014) A classification of growth friendly spine implants. J Pediatr Orthop 34(3):260–274. https://doi.org/10.1097/BPO.0000000000000073
Newton PO, Kluck DG, Saito W, Yaszay B, Bartley CE, Bastrom TP (2018) Anterior spinal growth tethering for skeletally immature patients with scoliosis: a retrospective look two to four years postoperatively. J Bone Joint Surg Am 100(19):1691–1697. https://doi.org/10.2106/JBJS.18.00287
Samdani AF, Ames RJ, Kimball JS et al (2015) Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one- year results on the first 32 patients. Eur Spine J 24:1533–1539
Mehlman CT, Araghi A, Roy DR (1997) Hyphenated history: the Hueter-Volkmann law. Am J Orthop (Belle Mead NJ) 26:798–800
Parent S, Shen J (2020) Anterior vertebral body growth-modulation tethering in idiopathic scoliosis: surgical technique. J Am Acad Orthop Surg 28(17):693–699. https://doi.org/10.5435/JAAOS-D-19-00849
Spurway AJ, Hurry JK, Gauthier L, Orlik B, Chukwunyerenwa CK, Kishta WE, El-Hawary R (2017) Three-dimensional true spine length: a novel technique for assessing the outcomes of scoliosis surgery. J Pediatr Orthop 37(8):e631–e637. https://doi.org/10.1097/BPO.0000000000001031
Brown JD et al (2022) Paper 2, 16th international congress on early onset scoliosis. Spine Deform 10(Suppl 1):1–27. https://doi.org/10.1007/s43390-022-00597-3
Dimeglio A, Canavese F (2012) The growing spine: how spinal deformities influence normal spine and thoracic cage growth. Eur Spine J 21(1):64–70. https://doi.org/10.1007/s00586-011-1983-3
Dimeglio A, Canavese F (2020) The immature spine: growth and idiopathic scoliosis. Ann Transl Med 8(2):22. https://doi.org/10.21037/atm.2019.11.134
Dimeglio A, Canavese F, Bonnel F, Parent S (2022) Normal Growth of the Spine. In: Akbarnia BA, Thompson GH, Yazici M, El-Hawary R (eds) The growing spine. Springer, Cham
Photopoulos G, Hurry J, Murphy J, Brooks J, Fitzgerald R, Louer C, Shaw K, Smit K, Miyanji F, Parent S, El-Hawary R, Pediatric Spine Study Group (2022) Reliability of radiographic assessment of growth modulation from anterior vertebral body tethering surgery in pediatric scoliosis. Spine Deform. https://doi.org/10.1007/s43390-022-00570-0
Photopoulos et al (2022) Paper 20, 16th international congress on early onset scoliosis. Spine Deform 10(Suppl 1):1–27. https://doi.org/10.1007/s43390-022-00597-3
Farivar D, Parent S, Miyanji F, Heffernan MJ, El-Hawary R, Larson AN, Andras LM, Skaggs DL, Pediatric Spine Study Group (2023) Concave and convex growth do not differ over tethered vertebral segments, even with open tri-radiate cartilage. Spine Deform. https://doi.org/10.1007/s43390-023-00683-0. (Epub ahead of print)
Mishreky A, Parent S, Miyanji F et al (2022) Body mass index affects outcomes after vertebral body tethering surgery. Spine Deform 10(3):563–571. https://doi.org/10.1007/s43390-021-00455-8
Sanders JO, Khoury JG, Kishan S, Browne RH, Mooney JF 3rd, Arnold KD, McConnell SJ, Bauman JA, Finegold DN (2008) Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am 90(3):540–553. https://doi.org/10.2106/JBJS.G.00004
Baroncini A, Courvoisier A, Berjano P et al (2022) The effects of vertebral body tethering on sagittal parameters: evaluations from a 2-years follow-up. Eur Spine J 31:1060–1066. https://doi.org/10.1007/s00586-021-07076-9
Hoernschemeyer DG, Boeyer ME, Robertson ME, Loftis CM, Worley JR, Tweedy NM, Gupta SU, Duren DL, Holzhauser CM, Ramachandran VM (2020) Anterior vertebral body tethering for adolescent scoliosis with growth remaining: a retrospective review of 2–5-year postoperative results. J Bone Joint Surg Am 102(13):1169–1176. https://doi.org/10.2106/JBJS.19.00980
Rushton PRP, Nasto L, Parent S, Turgeon I, Aldebeyan S, Miyanji F (2021) Anterior vertebral body tethering for treatment of idiopathic scoliosis in the skeletally immature: results of 112 cases. Spine (Phila Pa 1976) 46(21):1461–1467. https://doi.org/10.1097/BRS.0000000000004061
Author information
Authors and Affiliations
Consortia
Contributions
Design or the acquisition, analysis, or interpretation of data: Mathieu Boulet, Jennifer Hurry, David Skaggs, Michelle Welborn, Lindsay Andras, Craig Louer, A. Noelle Larson, Firoz Miyanji, Stefan Parent, Pediatric Spine Study Group, Ron El-Hawary.
Corresponding author
Ethics declarations
Conflict of interest
Mathieu Boulet has nothing to disclose. Jennifer Hurry reports a fellowship from Depuy Synthes. David Skaggs reports personal fees or stocks from Globus Medical, Orthobullets, Top Doctors, ZimmerBiomet, and Zipline Medical; IP or publishing royalties from Globus Medical, Medtronic, ZimmerBiomet and Wolters Kluwer Health; grant from Nuvasive; board or committee member for Pediatric Spine Foundation, Pediatric Spine Study Group, and the Scoliosis Research Society; and editorial or governing board of OrthoBullets, Orthopedics Today, and the Journal of Children’s Orthopaedics, outside the submitted work. Michelle Cameron Welborn reports personal fees from AstraZeneca Rare Disease, DePuy, A Johnson & Johnson Company, Nuvasive, Orthopediatrics, Stryker, and Synthes; research support from the Pediatric Orthopaedic Society of North America, Shriners Hospital for Children, and ZimVie; board or committee member of the Pediatric Orthopaedic Society of North America, Pediatric Spine Study Group, and the Scoliosis Research Society; and editorial or governing board of the Journal of Pediatric Orthopedics, Spine Journal, and the Journal of Spine Deformity, outside the submitted work. Lindsay Andras reports personal fees or stocks from Eli Lilly, Medtronic, Nuvasive, Orthobullets, and Zimmer Biomet; board or committee member for the Pediatric Orthopaedic Society of North America and the Scoliosis Research Society; and editorial or governing board of Journal of Pediatric Orthopedics, outside the submitted work. Craig Louer reports personal fees from DePuy, A Johnson & Johnson Company, royalties from National Scoliosis Clinics, Inc., research grants from Pediatric Orthopaedic Society of North America and NuVasive, outside the submitted work. A. Noelle Larson reports grants from DePuy, A Johnson & Johnson Company, Globus Medical, Medtronic, Orthopediatrics, and Zimmer; and board or committee member of the Scoliosis Research Society, outside the submitted work. Firoz Miyanji reports personal fees from DePuy, A Johnson & Johnson Company, Stryker, Zimmer and OrthoPediatrics; board or committee member of the Pediatric Orthopaedic Society of North America; and grant from DePuy, outside the submitted work. Stefan Parent reports personal fees from EOS-imaging, Spinologics, and DePuy, a Johnson & Johnson Company; Academic Research chair in spine deformities of the CHU Sainte-Justine (DePuy), grants from EOS-imaging, DePuy and the Setting Scoliosis Straight Foundation; board or committee member with the Canadian Spine Society, Pediatric Orthopaedic Society of North America, and the Scoliosis Research Society; and IP royalties from Rodin 4D, outside the submitted work. Pediatric Spine Study Group reports grants from DePuy Synthes Spine, grants from Medtronic, grants from NuVasive, grants from Globus Medical Inc., grants from OrthoPediatrics, grants from Zimmer Biomet, grants from Pediatric Spine Foundation, grants from Stryker, outside the submitted work. Ron El-Hawary reports personal fees from Depuy Synthes Spine, personal fees from Medtronic Spine, grants from Depuy Synthes Spine, grants from Medtronic Spine, personal fees from Orthopediatrics, other from Pediatric Spine Foundation, other from Scoliosis Research Society, outside the submitted work.
Ethical approval
This work is a sub-study of the Pediatric Spine Study Group Registry which was approved by the Research Ethics Board at the IWK Health Centre (#1002256) in accordance with the ethical standards outlined in the Tri-Council Policy Statement and the 1964 Declaration of Helsinki and its later amendments.
Consent to participate
All research participants or their legal guardians provided written consent to be a part of the registry and have the data collected be used in ongoing research on scoliosis.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Boulet, M., Hurry, J., Skaggs, D. et al. Analysis of three-dimensional spine growth for vertebral body tethering patients at 2 and 5 years post operatively. Spine Deform (2024). https://doi.org/10.1007/s43390-024-00857-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43390-024-00857-4