Abstract
Purpose
Surgical treatment of early-onset scoliosis (EOS) is associated with high rates of complications, often requiring unplanned return to the operating room (UPROR). The aim of this study was to create and validate a machine learning model to predict which EOS patients will go on to require an UPROR during their treatment course.
Methods
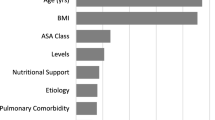
A retrospective review was performed of all surgical EOS patients with at least 2 years follow-up. Patients were stratified based on whether they had experienced an UPROR. Ten machine learning algorithms were trained using tenfold cross-validation on an independent training set of patients. Model performance was evaluated on a separate testing set via their area under the receiver operating characteristic curve (AUC). Relative feature importance was calculated for the top-performing model.
Results
257 patients were included in the study. 146 patients experienced at least one UPROR (57%). Five factors were identified as significant and included in model training: age at initial surgery, EOS etiology, initial construct type, and weight and height at initial surgery. The Gaussian naïve Bayes model demonstrated the best performance on the testing set (AUC: 0.79). Significant protective factors against experiencing an UPROR were weight at initial surgery, idiopathic etiology, initial definitive fusion construct, and height at initial surgery.
Conclusions
The Gaussian naïve Bayes machine learning algorithm demonstrated the best performance for predicting UPROR in EOS patients. Heavier, taller, idiopathic patients with initial definitive fusion constructs experienced UPROR less frequently. This model can be used to better quantify risk, optimize patient factors, and choose surgical constructs.
Level of evidence
Prognostic: III.



Similar content being viewed by others
Data availability
Data available upon request.
References
Williams BA, Matsumoto H, McCalla DJ et al (2014) Development and initial validation of the classification of early-onset scoliosis (C-EOS). J Bone Joint Surg 96:1359–1367. https://doi.org/10.2106/JBJS.M.00253
Anari JB, Flynn JM, Cahill PJ et al (2020) Unplanned return to OR (UPROR) for children with early onset scoliosis (EOS): a comprehensive evaluation of all diagnoses and instrumentation strategies. Spine Deform 8:295–302. https://doi.org/10.1007/S43390-019-00024-0/METRICS
Keil LG, Nash AB, Stürmer T et al (2021) When is a growth-friendly strategy warranted? A matched comparison of growing rods versus primary posterior spinal fusion in juveniles with early-onset scoliosis. J Pediatr Orthop 41:e859–e864. https://doi.org/10.1097/BPO.0000000000001926
Johnson MA, Lott C, Qiu C et al (2021) Rib-based distraction device implantation before age 3 associated with higher unplanned rate of return to the operating room. J Pediatr Orthop 41:e369–e373. https://doi.org/10.1097/BPO.0000000000001823
Roye BD, Fano AN, Matsumoto H et al (2021) The impact of unplanned return to the operating room on health-related quality of life at the end of growth-friendly surgical treatment for early-onset scoliosis. J Pediatr Orthop 42:17–22. https://doi.org/10.1097/BPO.0000000000002006
Basu S, Solanki AM, Srivastava A et al (2020) Unplanned return to operation room (OR) following growing spinal constructs (GSCs) in early onset scoliosis (EOS)-a multi-centric study. Eur Spine J 29:2075–2083. https://doi.org/10.1007/S00586-020-06506-4
Welborn MC, Bouton D (2021) Outcomes of MCGR at > 3 year average follow-up in severe scoliosis: who undergoes elective revision vs UPROR? Spine Deform 10:457–463. https://doi.org/10.1007/S43390-021-00424-1
Upasani VV, Parvaresh KC, Pawelek JB et al (2016) Age at initiation and deformity magnitude influence complication rates of surgical treatment with traditional growing rods in early-onset scoliosis. Spine Deform 4:344–350. https://doi.org/10.1016/J.JSPD.2016.04.002
Sankar WN, Acevedo DC, Skaggs DL (2010) Comparison of complications among growing spinal implants. Spine 35:2091–2096. https://doi.org/10.1097/BRS.0B013E3181C6EDD7
Bess S, Akbarnia BA, Thompson GH et al (2010) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg 92:2533–2543. https://doi.org/10.2106/JBJS.I.01471
Watanabe K, Uno K, Suzuki T et al (2013) Risk factors for complications associated with growing-rod surgery for early-onset scoliosis. Spine 38:E464–E468. https://doi.org/10.1097/BRS.0B013E318288671A
Lebon J, Batailler C, Wargny M et al (2017) Magnetically controlled growing rod in early onset scoliosis: a 30-case multicenter study. Eur Spine J 26:1567–1576. https://doi.org/10.1007/S00586-016-4929-Y
Kwan KYH, Alanay A, Yazici M et al (2017) Unplanned reoperations in magnetically controlled growing rod surgery for early onset scoliosis with a minimum of two-year follow-up. Spine 42:E1410–E1414. https://doi.org/10.1097/BRS.0000000000002297
Choi E, Yaszay B, Mundis G et al (2017) Implant complications after magnetically controlled growing rods for early onset scoliosis: a multicenter retrospective review. J Pediatr Orthop 37:e588–e592. https://doi.org/10.1097/BPO.0000000000000803
la Rosa G, Oggiano L, Ruzzini L (2017) Magnetically controlled growing rods for the management of early-onset scoliosis: a preliminary report. J Pediatr Orthop 37:79–85. https://doi.org/10.1097/BPO.0000000000000597
Liu Y, Chen PHC, Krause J et al (2019) How to read articles that use machine learning: users’ guides to the medical literature. JAMA 322:1806–1816. https://doi.org/10.1001/JAMA.2019.16489
Myers TG, Ramkumar PN, Ricciardi BF et al (2020) Artificial intelligence and orthopaedics: an introduction for clinicians. J Bone Joint Surg 102:830–840. https://doi.org/10.2106/JBJS.19.01128
Kunze KN, Polce EM, Clapp I et al (2021) Machine learning algorithms predict functional improvement after hip arthroscopy for femoroacetabular impingement syndrome in athletes. J Bone Joint Surg 103:1055–1062. https://doi.org/10.2106/JBJS.20.01640
Steyerberg EW, Vickers AJ, Cook NR et al (2010) Assessing the performance of prediction models: a framework for some traditional and novel measures. Epidemiology 21:128–138. https://doi.org/10.1097/EDE.0b013e3181c30fb2
el Khouli RH, Macura KJ, Barker PB et al (2009) The Relationship of temporal resolution to diagnostic performance for dynamic contrast enhanced (DCE) MRI of the breast. J Magn Reson Imaging 30:999. https://doi.org/10.1002/JMRI.21947
Polce EM, Kunze KN, Fu MC et al (2021) Development of supervised machine learning algorithms for prediction of satisfaction at 2 years following total shoulder arthroplasty. J Shoulder Elbow Surg 30:e290–e299. https://doi.org/10.1016/J.JSE.2020.09.007
Pedregosa F, Michel V, Grisel O et al (2011) Scikit-learn: machine learning in Python. J Mach Learn Res 12:2825–2830
Devana SK, Shah AA, Lee C et al (2021) Development of a machine learning algorithm for prediction of complications and unplanned readmission following reverse total shoulder arthroplasty. J Shoulder Elbow Arthroplasty 5:247154922110381. https://doi.org/10.1177/24715492211038172
Matsumoto H, Larson EL, Warren SI et al (2022) A clinical risk model for surgical site infection following pediatric spine deformity surgery. J Bone Joint Surg 104:364–375. https://doi.org/10.2106/JBJS.21.00751
Li Y, Swallow J, Gagnier J et al (2021) Growth-friendly surgery results in more growth but a higher complication rate and unplanned returns to the operating room compared to single fusion in neuromuscular early-onset scoliosis: a multicenter retrospective cohort study. Spine Deform 9:851–858. https://doi.org/10.1007/S43390-020-00270-7
Mackey C, Hanstein R, Lo Y et al (2022) Magnetically controlled growing rods (MCGR) versus single posterior spinal fusion (PSF) versus vertebral body tether (VBT) in older early onset scoliosis (EOS) patients: how do early outcomes compare? Spine 47:295–302. https://doi.org/10.1097/BRS.0000000000004245
Johnston CE, Thornberg DC, Palmer R (2023) Comparison of treatment outcomes between growth-sparing instrumentation and definitive one-stage fusion for EOS patients ages 6–10 years. Spine Deform 11:1529–1537. https://doi.org/10.1007/S43390-023-00731-9
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Brett R. Lullo, MD: conception, design, data collection, analysis, writing—first draft, reviewing and editing, approval, accountability; Patrick J. Cahill, MD: conception, design, data collection, reviewing and editing, approval, accountability; John M. Flynn, MD: conception, design, data collection, reviewing and editing, approval, accountability; Jason B. Anari, MD: conception, design, data collection, reviewing and editing, approval, accountability, project administration, supervision.
Corresponding author
Ethics declarations
Conflict of interest
Brett Lullo has no financial interests. Patrick Cahill has research grants from Setting Scoliosis Straight Foundation in support of Harms Study Group; research grants from the Pediatric Spine Foundation in support of research with the Pediatric Spine Study Group; a patent for dynamic lung magnetic resonance imaging, but this has not been commercialized nor has he received money for it; provisional patent for pediatric deformity system. John Flynn receives royalties from Wolters Kluwer and ZimVie. Jason Anari receives consulting fees from DePuy Synthes.
Ethical approval
The study was reviewed by the Children’s Hospital of Philadelphia IRB on 3/13/2019. The IRB has determined that it meets the exemption criteria per 45 CFR 46.104(d) 4(iii).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lullo, B.R., Cahill, P.J., Flynn, J.M. et al. Predicting early return to the operating room in early-onset scoliosis patients using machine learning techniques. Spine Deform (2024). https://doi.org/10.1007/s43390-024-00848-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43390-024-00848-5