Abstract
Purpose
To investigate the effect of a prehabilitation program on peri- and post-operative outcomes in adult cervical deformity (CD) surgery.
Methods
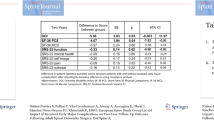
Operative CD patients ≥ 18 years with complete baseline (BL) and 2-year (2Y) data were stratified by enrollment in a prehabilitation program beginning in 2019. Patients were stratified as having undergone prehabilitation (Prehab+) or not (Prehab−). Differences in pre and post-op factors were assessed via means comparison analysis. Costs were calculated using PearlDiver database estimates from Medicare pay-scales.
Results
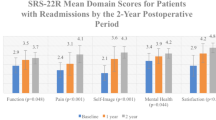
115 patients were included (age: 61 years, 70% female, BMI: 28 kg/m2). Of these patients, 57 (49%) were classified as Prehab+. At baseline, groups were comparable in age, gender, BMI, CCI, and frailty. Surgically, Prehab+ were able to undergo longer procedures (p = 0.017) with equivalent EBL (p = 0.627), and shorter SICU stay (p < 0.001). Post-operatively, Prehab+ patients reported greater reduction in pain scores and greater improvement in quality of life metrics at both 1Y and 2Y than Prehab− patients (all p < 0.05). Prehab+ patients reported significantly less complications overall, as well as less need for reoperation (all p < 0.05).
Conclusion
Introducing prehabilitation protocols in adult cervical deformity surgery may aid in improving patient physiological status, enabling patients to undergo longer surgeries with lessened risk of peri- and post-operative complications.


Similar content being viewed by others
References
Scheer JK, Lau D, Ames CP (2021) Sagittal balance of the cervical spine. J Orthop Surg. https://doi.org/10.1177/23094990211024454
Smith JS, Line B, Bess S et al (2017) The health impact of adult cervical deformity in patients presenting for surgical treatment: comparison to united states population norms and chronic disease states based on the EuroQuol-5 dimensions questionnaire. Neurosurgery 80(5):716–725. https://doi.org/10.1093/neuros/nyx028
Elias E, Bess S, Line BG et al (2022) Operative treatment outcomes for adult cervical deformity: a prospective multicenter assessment with mean 3-year follow-up. J Neurosurg Spine 37(6):855–864. https://doi.org/10.3171/2022.6.Spine22422
Smith JS, Buell TJ, Shaffrey CI et al (2020) Prospective multicenter assessment of complication rates associated with adult cervical deformity surgery in 133 patients with minimum 1-year follow-up. J Neurosurg Spine. https://doi.org/10.3171/2020.4.Spine20213
Flexman AM, Charest-Morin R, Stobart L et al (2016) Frailty and postoperative outcomes in patients undergoing surgery for degenerative spine disease. Spine J 16(11):1315–1323. https://doi.org/10.1016/j.spinee.2016.06.017
Gometz A, Maislen D, Youtz C et al (2018) The effectiveness of prehabilitation (prehab) in both functional and economic outcomes following spinal surgery: a systematic review. Cureus 10(5):e2675. https://doi.org/10.7759/cureus.2675
Fors M, Enthoven P, Abbott A et al (2019) Effects of pre-surgery physiotherapy on walking ability and lower extremity strength in patients with degenerative lumbar spine disorder: secondary outcomes of the PREPARE randomised controlled trial. BMC Musculoskelet Disord 20(1):468. https://doi.org/10.1186/s12891-019-2850-3
Eubanks JE, Carlesso C, Sundaram M et al (2023) Prehabilitation for spine surgery: a scoping review. PM R J Injury Funct Rehabil 15(10):1335–1350. https://doi.org/10.1002/pmrj.12956
Passias PG, Williamson TK, Pierce KE et al (2023) The importance of incorporating proportional alignment in adult cervical deformity corrections relative to regional and global alignment: steps toward development of a cervical-specific score. Spine (Phila Pa 1976). https://doi.org/10.1097/brs.0000000000004843
Passias PG, Tretiakov PS, Smith JS et al (2023) Are we improving in the optimization of surgery for high-risk adult cervical spine deformity patients over time? J Neurosurg Spine. https://doi.org/10.3171/2023.5.Spine23457
Tretiakov PS, Budis E, Dave P et al (2023) Does the presence of cervical deformity in patients with baseline mild myelopathy increase operative urgency in adult cervical spinal surgery? A retrospective analysis. Neurosurg Focus 55(3):E9. https://doi.org/10.3171/2023.6.Focus23304
Tetreault L, Kopjar B, Côté P et al (2015) A clinical prediction rule for functional outcomes in patients undergoing surgery for degenerative cervical myelopathy: analysis of an international prospective multicenter data set of 757 subjects. J Bone Jt Surg Am 97(24):2038–2046. https://doi.org/10.2106/jbjs.O.00189
Carreon LY, Glassman SD, Campbell MJ et al (2010) Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J 10(6):469–474. https://doi.org/10.1016/j.spinee.2010.02.007
Le QA, Doctor JN, Zoellner LA et al (2013) Minimal clinically important differences for the EQ-5D and QWB-SA in Post-traumatic Stress Disorder (PTSD): results from a Doubly Randomized Preference Trial (DRPT). Health Quali Life Outcomes 11:59. https://doi.org/10.1186/1477-7525-11-59
Parker SL, Adogwa O, Paul AR et al (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 14(5):598–604. https://doi.org/10.3171/2010.12.Spine10472
Champain S, Benchikh K, Nogier A et al (2006) Validation of new clinical quantitative analysis software applicable in spine orthopaedic studies. Eur Spine J 15(6):982–991. https://doi.org/10.1007/s00586-005-0927-1
Rillardon L, Levassor N, Guigui P et al (2003) Validation of a tool to measure pelvic and spinal parameters of sagittal balance [Validation d’un outil de mesure des paramètres pelviens et rachidiens de l’équilibre sagittal du rachis]. Rev Chir Orthop Reparatrice Appar Mot 89(3):218–227
O’Brien MF KT, Blanke KM, Lenke LG (2022) Spinal Deformity Study Group radiographic measurement manual. Medtronic Sofamor Danek USA, Inc. https://www.oref.org/docs/default-source/default-document-library/sdsg-radiographic-measuremnt-manual.pdf?sfvrsn=2&sfvrsn=2. Accessed 4 Jan 2022
Santa Mina D, Clarke H, Ritvo P et al (2014) Effect of total-body prehabilitation on postoperative outcomes: a systematic review and meta-analysis. Physiotherapy 100(3):196–207. https://doi.org/10.1016/j.physio.2013.08.008
Raad M, Neuman BJ, Jain A et al (2018) The use of patient-reported preoperative activity levels as a stratification tool for short-term and long-term outcomes in patients with adult spinal deformity. J Neurosurg Spine 29(1):68–74. https://doi.org/10.3171/2017.10.Spine17830
Debono B, Wainwright TW, Wang MY et al (2021) Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Spine J 21(5):729–752. https://doi.org/10.1016/j.spinee.2021.01.001
Cabilan CJ, Hines S, Munday J (2015) The effectiveness of prehabilitation or preoperative exercise for surgical patients: a systematic review. JBI Database Syst Rev Implement Rep 13(1):146–187. https://doi.org/10.11124/jbisrir-2015-1885
Rolving N, Nielsen CV, Christensen FB et al (2015) Does a preoperative cognitive-behavioral intervention affect disability, pain behavior, pain, and return to work the first year after lumbar spinal fusion surgery? Spine (Phila Pa 1976) 40(9):593–600. https://doi.org/10.1097/brs.0000000000000843
Rolving N, Sogaard R, Nielsen CV et al (2016) Preoperative cognitive-behavioral patient education versus standard care for lumbar spinal fusion patients: economic evaluation alongside a randomized controlled trial. Spine (Phila Pa 1976) 41(1):18–25. https://doi.org/10.1097/brs.0000000000001254
Nielsen PR, Jørgensen LD, Dahl B et al (2010) Prehabilitation and early rehabilitation after spinal surgery: randomized clinical trial. Clin Rehabil 24(2):137–148. https://doi.org/10.1177/0269215509347432
Maitra S, Mikhail C, Cho SK et al (2020) Preoperative maximization to reduce complications in spinal surgery. Glob Spine J 10(1 Suppl):45s–52s. https://doi.org/10.1177/2192568219882349
Minhas SV, Mazmudar AS, Patel AA (2017) Pre-operative functional status as a predictor of morbidity and mortality after elective cervical spine surgery. Bone Jt J 99-B(6):824–828. https://doi.org/10.1302/0301-620x.99b6.Bjj-2016-1149.R1
Smith JS, Kelly MP, Buell TJ et al (2023) Adult cervical deformity patients have higher baseline frailty, disability, and comorbidities compared with complex adult thoracolumbar deformity patients: a comparative cohort study of 616 patients. Glob Spine J. https://doi.org/10.1177/21925682231214059
Oe S, Yamato Y, Hasegawa T et al (2020) Association between a prognostic nutritional index less than 50 and the risk of medical complications after adult spinal deformity surgery. J Neurosurg Spine. https://doi.org/10.3171/2020.1.Spine191410
Oe S, Watanabe J, Akai T et al (2022) The effect of preoperative nutritional intervention for adult spinal deformity patients. Spine (Phila Pa 1976) 47(5):387–395. https://doi.org/10.1097/brs.0000000000004227
Gillis C, Loiselle SE, Fiore JF Jr et al (2016) Prehabilitation with whey protein supplementation on perioperative functional exercise capacity in patients undergoing colorectal resection for cancer: a pilot double-blinded randomized placebo-controlled trial. J Acad Nutr Diet 116(5):802–812. https://doi.org/10.1016/j.jand.2015.06.007
Smedley F, Bowling T, James M et al (2004) Randomized clinical trial of the effects of preoperative and postoperative oral nutritional supplements on clinical course and cost of care. Br J Surg 91(8):983–990. https://doi.org/10.1002/bjs.4578
Funding
None to disclose.
Author information
Authors and Affiliations
Contributions
Pawel P. Jankowski, Peter S. Tretiakov, Oluwatobi O. Onafowokan, Ankita Das, Bailey Imbo, Oscar Krol, Rachel Joujon-Roche, Tyler Williamson, Pooja Dave, Jamshaid Mir, Stephane Owusu-Sarpong, Peter G. Passias: Active involvement in drafting and critical revision of manuscript, Provided final approval of version to be published, Study Design, Data Acquisition, Analysis and interpretation of data.
Corresponding author
Ethics declarations
Conflict of interest
None to disclose. Disclosures unrelated to current work: Peter G Passias: Cerapedics: Other financial or material support. Cervical Scoliosis Research Society: Research support. Globus Medical: Paid presenter or speaker. Medtronic: Paid consultant. Royal Biologics: Paid consultant. Spine: Editorial or governing board. Spinevision: Other financial or material support. SpineWave: Paid consultant. Terumo: Paid consultant.
Ethical approval
Institutional review board approval was gained prior to commencement of the study.
Informed consent
Gained from all patients prior to enrolment in study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jankowski, P.P., Tretiakov, P.S., Onafowokan, O.O. et al. Assessing the effects of prehabilitation protocols on post-operative outcomes in adult cervical deformity surgery: does early optimization lead to optimal clinical outcomes?. Spine Deform (2024). https://doi.org/10.1007/s43390-024-00845-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43390-024-00845-8