Abstract
Purpose
In 2018, Best Practice Guidelines (BPGs) were published for preventing wrong-level surgery in pediatric spinal deformity, but successful implementation has not been established. The purpose of this study was to evaluate BPG compliance 5 years after publication. We hypothesized higher compliance among BPG authors and among surgeons with more experience, higher caseload, and awareness of the BPGs.
Methods
We queried North American and European surgeons, authors and nonauthors, and members of pediatric spinal study groups on adherence to BPGs using an anonymous survey consisting of 18 Likert scale questions. Respondents provided years in practice, yearly caseload, and guideline awareness. Mean compliance scores (MCS) were developed by correlating Likert responses with MCS scores (“None of the time” = no compliance = MCS 0, “Sometimes” = weak to moderate = MCS 1, “Most of the time” = high = MCS 2, and “All the time” = perfect = MCS 3).
Results
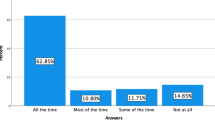
Of the 134 respondents, 81.5% reported high or perfect compliance. Average MCS for all guidelines was 2.4 ± 0.4. North American and European surgeons showed no compliance differences (2.4 vs. 2.3, p = 0.07). Authors and nonauthors showed significantly different compliance scores (2.8 vs 2.4, p < 0.001), as did surgeons with and without knowledge of the BPGs (2.5 vs 2.2, p < 0.001). BPG awareness and compliance showed a moderate positive correlation (r = 0.48, p < 0.001), with non-significant associations between compliance and both years in practice (r = 0.41, p = 0.64) and yearly caseload (r = 0.02, p = 0.87).
Conclusion
Surgeons reported high or perfect compliance 81.5% of the time with BPGs for preventing wrong-level surgery. Authorship and BPG awareness showed increased compliance. Location, study group membership, years in practice, and yearly caseload did not affect compliance.
Level of evidence
Level V—expert opinion.

Similar content being viewed by others
Data availability
Data available if requested to primary author.
References
Hsiang J (2011) Wrong-level surgery: a unique problem in spine surgery. Surg Neurol Int 2:47. https://doi.org/10.4103/2152-7806.79769
Mody MG, Nourbakhsh A, Stahl DL, Gibbs M, Alfawareh M, Garges KJ (2008) The prevalence of wrong-level surgery among spine surgeons. Spine 33(2):194–198
James MA, Seiler JG, Harrast JJ, Emery SE, Hurwitz S (2012) The occurrence of wrong-site surgery self-reported by candidates for certification by the American Board of Orthopaedic Surgery. J Bone Jt Surg. https://doi.org/10.2106/JBJS.K.00524
Longo UG, Loppini M, Maffulli N, Denaro V (2012) Errors of level in spinal surgery an evidence-based systematic review. J Bone Jt Surg- Ser B 94(11):1457–1461. https://doi.org/10.1302/0301-620X.94B11
Hashmi SS, Seifert KD, Massoud TF (2022) Thoracic and lumbosacral spine anatomy. Neuroimaging Clin North Am 32(4):889–902. https://doi.org/10.1016/j.nic.2022.07.024. (W.B. Saunders)
Ibrahim DA, Myung KS, Skaggs DL (2013) Ten percent of patients with adolescent idiopathic scoliosis have variations in the number of thoracic or lumbar vertebrae. J Bone Jt Surg 95(9):828–833. https://doi.org/10.2106/JBJS.L.00461. (Journal of Bone and Joint Surgery Inc.)
Hu Z, Zhang Z, Zhao Z, Zhu Z, Liu Z, Qiu Y (2016) A neglected point in surgical treatment of adolescent idiopathic scoliosis: variations in the number of vertebrae. Medicine (United States). https://doi.org/10.1097/MD.0000000000004682
Kidd Chiu C, Fu Chin T, Hong Chung W, Yin Wei Chan C, Keong Kwan M (2023) Variations in the number of vertebrae, prevalence of lumbosacral transitional vertebra and prevalence of cervical rib among surgical patients with adolescent idiopathic scoliosis: an analysis of 998 radiographs. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0000000000004711
Makhni MC et al (2018) The medicolegal landscape of spine surgery: how do surgeons fare? Spine J 18(2):209–215. https://doi.org/10.1016/j.spinee.2017.06.038
The Joint Commission (2008) Universal protocol for preventing wrong site, wrong procedure, wrong person surgery. Accessed: Feb. 10, 2023. Available: https://www.jointcommission.org/standards/universal-protocol/#33ea8500e8794bf08949c7ef319f4f65
Vitale M et al (2018) Building consensus: development of best practice guidelines on wrong level surgery in spinal deformity. Spine Deform 6(2):121–129. https://doi.org/10.1016/j.jspd.2017.08.005
Linstone HA, Turoff M and Helmer O (2002) The Delphi method techniques and applications
O’brien MF, Kuklo TR, Blanke KM and Lenke LG (2008) Spinal deformity study group radiographic measurement manual
Ammerman JM, Ammerman MD (2009) Wrong-sided surgery. J Neurosurg 9:105–106
Devine J, Chutkan N, Norvell DC and Dettori JR (2010) Avoiding wrong site surgery a systematic review. Spine (Phila Pa 1976) 35:28–36. http://links.lww.com/BRS/A418
Barrios C, Ahmed M, Arrotegui J, Bjornsson A, Gillstrom P (1990) Microsurgery versus standard removal of the herniated lumbar disc A 3-year comparison in 150 cases. Acta Orthop 61(5):399–403
Jhawar BS, Mitsis D, Duggal N (2007) Wrong-sided and wrong-level neurosurgery: a national survey. J Neurosurg 7(5):467–472. https://doi.org/10.3171/SPI-07/11/467. (American Association of Neurological Surgeons)
Matsumoto M et al (2010) Incidence of complications associated with spinal endoscopic surgery: nationwide survey in 2007 by the committee on spinal endoscopic surgical skill qualification of Japanese Orthopaedic Association. J Orthop Sci 15(1):92–96. https://doi.org/10.1007/s00776-009-1428-6
Eie N, Solgaard T, Kleppe H (1983) The knee-elbow position in lumbar disc surgery: a review of complications. Spine (Phila Pa 1976) 8:897–900
Groff MW, Heller JE, Potts EA, Mummaneni PV, Shaffrey CI, Smith JS (2013) A survey-based study of wrong-level lumbar spine surgery: the scope of the problem and current practices in place to help avoid these errors. World Neurosurg 79(3–4):585–592. https://doi.org/10.1016/j.wneu.2012.03.017
Spencer HT, Gold ME, Hresko MT (2014) Abnormal rib count in scoliosis surgery: impact on the reporting of spinal fusion levels. J Child Orthop 8(6):497–503. https://doi.org/10.1007/s11832-014-0623-y
Garg B, Mehta N, Goyal A, Rangaswamy N, Upadhayay A (2021) Variations in the number of thoracic and lumbar vertebrae in patients with adolescent idiopathic scoliosis: a retrospective, observational study. Int J Spine Surg. https://doi.org/10.14444/8047
Palumbo MA, Bianco AJ, Esmende S, Daniels AH (2013) Wrong-site spine surgery. J Am Acad Orthop Surg 21(5):312–320. https://doi.org/10.5435/JAAOS-21-05-312
Goodkin R, Laska LL, Fager CA, Pawl R, Matz MI (2004) Wrong disc space level surgery: medicolegal implications. Surg Neurol 61(4):323–341. https://doi.org/10.1016/j.surneu.2003.08.022
Johnson SB et al (2008) An electronic health record based on structured narrative. J Am Med Inform Assoc 15(1):54–64. https://doi.org/10.1197/jamia.M2131
Fielstein EM, Brown SH, Mcbrine CS, Clark TK, Hardenbrook SP and Speroff T (2006) The effect of standardized, computer-guided templates on quality of VA disability exams. In: AMIA Annual Symposium Proceedings Archive, pp 249–253
Cao J et al (2017) Standardized note templates improve electronic medical record documentation of neurovascular examinations for pediatric supracondylar humeral fractures. JBJS Open Access. https://doi.org/10.2106/JBJS.OA.17.00027
Gabel MJ, Shipan CR (2004) A social choice approach to expert consensus panels. J Health Econ. https://doi.org/10.1016/j.jhealeco.2003.10.004
Eddy DM (1990) Challenging the quality of clinical decisions. J Am Med Assoc 263:287–290. Available: http://jama.jamanetwork.com/
Chan CM et al (2016) Effect of preoperative indications conference on procedural planning for treatment of scoliosis. Spine Deform 4(1):27–32. https://doi.org/10.1016/j.jspd.2015.05.003
Lindley EM, Botolin S, Burger EL, Patel VV (2011) Unusual spine anatomy contributing to wrong-level spine surgery: a case report and recommendations for decreasing the risk of preventable ‘never events.’ Patient Saf Surg. https://doi.org/10.1186/1754-9493-5-33
Malanga GA, Cooke PM (2004) Malanga and Cooke • segmental anatomy leading to wrong level surgery segmental anomaly leading to wrong level disc surgery in cauda Equina syndrome a case report. Pain Physician 7(1):107–110
Mayer JE, Dang RP, Duarte Prieto GF, Cho SK, Qureshi SA, Hecht AC (2014) Analysis of the techniques for thoracic- and lumbar-level localization during posterior spine surgery and the occurrence of wrong-level surgery: results from a national survey. Spine J 14(5):741–748. https://doi.org/10.1016/j.spinee.2013.06.068
Kadzielski J, McCormick F, Herndon JH, Rubash H, Ring D (2015) Surgeons’ attitudes are associated with reoperation and readmission rates. Clin Orthop Relat Res 473(5):1544–1551. https://doi.org/10.1007/s11999-014-3687-6
Holt RW, Boehm-Davis DA, Fitzgerald KA, Matyuf MM, Baughman WA, Littman DC (1991) Behavioral validation of a hazardous thought pattern instrument. Proc Human Fact Soc Annual Meet 35(2):77–81
Buch G, Diehl A (1984) An investigation of the effectiveness of pilot judgment training. Human Fact Soc 26(5):557–564
Doria C, Vaccino S (2009) Topical hemostasis: a valuable adjunct to control bleeding in the operating room, with a special focus on thrombin and fibrin sealants. Expert Opin Biol Ther 9(2):243–247. https://doi.org/10.1517/14712590802689258
Acknowledgements
Special thanks to Regina Wood, MPH from PSSG and Michelle Marks, PT MA from the Harms study group for their help with the distribution of the survey. Our gratitude also goes to Drs. Carol Hasler, René Castelein, Sébastien Pesenta, Ilkka Helenius, Dror Ovadia, David Farrington, Muharrem Yazici, Moyo Kruyt, Jorge Mineiro, and Oliana Madeira for helping distribute our survey among the EPOS Spine Study Group.
Funding
This study was not conducted with financial support.
Author information
Authors and Affiliations
Consortia
Contributions
Alondra Concepción-González BA, J. Manuel Sarmiento MD, Christina C. Rymond BA, Chinenye Ezeh MPH, Rishi Sinha MD, Hannah Lin, Kevin Lu MS, Afrain Z. Boby MS, Prakash Gorroochurn PhD, A. Noelle Larson MD, Benjamin D. Roye MD MPH, Brice Iharreborde MD, Michael G. Vitale MD MPH, European Pediatric Orthopaedic Society Spine Study Group, Pediatric Spine Study Group, Harms Study Group: Made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work, Drafted the work or revised it critically for important intellectual content, Approved the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Columbia University Institutional Review Board (Protocol AAAU3145) and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
This study qualifies for a waiver of consent, because it is a survey of surgeons and does not involve patient participation. There is no potential to adversely affect the rights or welfare of subjects, since this is a survey to gather surgeon opinion, with no patient data being collected or intervention being tested.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the instutional author group “European Pediatric Orthopaedic Society Spine Study Group, Pediatric Spine Study Group, Harms Study Group” was processed under acknowledgements section.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Concepción-González, A., Sarmiento, J.M., Rymond, C.C. et al. Evaluating compliance with the best practice guidelines for wrong-level surgery prevention in high-risk pediatric spine surgery. Spine Deform (2024). https://doi.org/10.1007/s43390-024-00836-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43390-024-00836-9