Abstract
Purpose
Determine peri-operative risk factors predictive for prematurely stopping surgery prior to completion of deformity correction due to intra-operative neuromonitoring changes.
Methods
A single institution retrospective review of adolescent idiopathic scoliosis (AIS) patients that underwent spinal fusion for curves greater than 70°. Cases aborted due to persistent loss of IONM were compared to completed cases. Demographic, radiographic, neurologic, and surgical information was reviewed.
Results
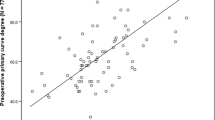
There were 453 total cases. Nine (9/453: (2%)) cases were aborted due to persistent loss of IONM, and 4 (4/453; (0.88%)) awoke with a neurologic deficit. Comparing to the 444 completed cases, pre-operative risk factors associated with case abortion were older age (15.3 vs. 13.8 years; p = 0.02), sex (male) (66.7% vs. 20.3%, p = 0.004), and larger cobb angles (87.6° vs. 79.2°; p = 0.01). Being male increased the risk of case abortion: 7.9X.
Intraoperative risk factors associated with case abortion were combined anterior/posterior approach (ASF/PSF) (44.4% vs. 7.2%; p = 0.003) and increased index procedure EBL (1127 vs. 769 mL; p = 0.043). ASF/PSF increased the risk: 10.3X.
Four (4/9;44%) of the aborted cases awoke with neurologic deficit. Motor strength returned at 2.3 days (0–18). Aborted cases returned to the OR after 12.6 ± 7.0 days (1–23) which was related to time to regain motor strength.
Conclusion
Pre-operative risk factors for AIS case abortion due to persistent loss of IOMN are older age, males, with larger Cobb angles. Intraoperative risk factors are combined ASF/PSF and increased index procedure EBL. Independent risk factors were sex (male) and ASF/PSF which increased the risk 7.9X and 10.3X, respectively.
Similar content being viewed by others
Availability of data and materials
Data will not be available.
References
Murphy RF, Mooney JF 3rd (2016) Complications following spine fusion for adolescent idiopathic scoliosis. Curr Rev Musculoskelet Med 9(4):462–469. https://doi.org/10.1007/s12178-016-9372-5
Bridwell KH, Shufflebarger HL, Lenke LG, Lowe TG, Betz Randal R, Bassett GS (2000) Parents’ and patients’ preferences and concerns in idiopathic adolescent scoliosis: a cross-sectional preoperative analysis. Spine 25(18):2392–2399
Mignemi M, Tran D, Ramo B, Richards BS (2018) Repeat surgical interventions following “definitive” instrumentation and fusion for idiopathic scoliosis: 25-year update. Spine Deform 6(4):409–416. https://doi.org/10.1016/j.jspd.2017.12.006
Vitale MG, Skaggs DL, Pace GI et al (2014) Best practices in intraoperative neuromonitoring in spine deformity surgery: development of an intraoperative checklist to optimize response. Spine Deform 2(5):333–339. https://doi.org/10.1016/j.jspd.2014.05.003
Vitale MG, Moore DW, Matsumoto H et al (2010) Risk factors for spinal cord injury during surgery for spinal deformity. J Bone Jt Surg Am 92(1):64–71. https://doi.org/10.2106/JBJS.H.01839
Lenke LG, Fano AN, Iyer RR et al (2022) Development of consensus-based best practice guidelines for response to intraoperative neuromonitoring events in high-risk spinal deformity surgery. Spine Deform 10(4):745–761. https://doi.org/10.1007/s43390-022-00485-w
Spitzer A, Patel R, Hasan S et al (2022) Absent baseline intraoperative neuromonitoring signals part I: adolescent idiopathic scoliosis: current concept review. J Pediatr Orthop Soc N Am. https://doi.org/10.55275/JPOSNA-2022-0018
IBM SPSS Statistics for Window, Version 27.0. Version 27.0. IBM; 2020
Stecker MM (2012) A review of intraoperative monitoring for spinal surgery. Surg Neurol Int 3(Suppl 3):S174–S187. https://doi.org/10.4103/2152-7806.98579
Park JH, Hyun SJ (2015) Intraoperative neurophysiological monitoring in spinal surgery. World J Clin Cases 3(9):765–773. https://doi.org/10.12998/wjcc.v3.i9.765
Thirumala PD, Huang J, Thiagarajan K, Cheng H, Balzer J, Crammond DJ (2016) Diagnostic accuracy of combined multimodality somatosensory evoked potential and transcranial motor evoked potential intraoperative monitoring in patients with idiopathic scoliosis. Spine (Phila Pa 1976) 41(19):E1177–E1184. https://doi.org/10.1097/BRS.0000000000001678
Hatef J, Katzir M, Toop N et al (2020) Damned if you monitor, damned if you don’t: medical malpractice and intraoperative neuromonitoring for spinal surgery. Neurosurg Focus 49(5):E19. https://doi.org/10.3171/2020.8.Focus20580
Feng B, Qiu G, Shen J et al (2012) Impact of multimodal intraoperative monitoring during surgery for spine deformity and potential risk factors for neurological monitoring changes. J Spinal Disord Tech 25(4):E108–E114. https://doi.org/10.1097/BSD.0b013e31824d2a2f
Bhagat S, Durst A, Grover H et al (2015) An evaluation of multimodal spinal cord monitoring in scoliosis surgery: a single centre experience of 354 operations. Eur Spine J 24(7):1399–1407. https://doi.org/10.1007/s00586-015-3766-8
Samdani AF, Bennett JT, Ames RJ et al (2016) Reversible intraoperative neurophysiologic monitoring alerts in patients undergoing arthrodesis for adolescent idiopathic scoliosis: what are the outcomes of surgery? J Bone Jt Surg Am 98(17):1478–1483. https://doi.org/10.2106/JBJS.15.01379
Lewis SJ, Gray R, Holmes LM et al (2011) Neurophysiological changes in deformity correction of adolescent idiopathic scoliosis with intraoperative skull-femoral traction. Spine (Phila Pa 1976) 36(20):1627–1638. https://doi.org/10.1097/BRS.0b013e318216124e
Fletcher N, Ghag R, Hedequist D, Imrie M, Bennett J, Glotzbecker M, POSNA QSVI Spine Committee (2023) Perioperative blood pressure management for patients undergoing spinal fusion for pediatric spinal deformity: current concept review. J Pediatr Orthop Soc N Am. https://doi.org/10.55275/JPOSNA-2023-602
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr. CZ, Dr. EF, Dr. CB, Ms. LK, and Dr. ALM. The first draft of the manuscript was written by Dr. CZ and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. CZ, MD: Substantially contributed to the design, data acquisition/interpretation. Drafted and revised critically for important intellectual content. Approval final version to be publish. Agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. EF, MD: Substantially contributed to the design, data acquisition/interpretation. Drafted and revised critically for important intellectual content. Approval final version to be publish. Agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. CB, MD: substantially contributed to the design, data acquisition/interpretation. Drafted and revised critically for important intellectual content. Approval final version to be publish. Agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. LK, BS: substantially contributed to the design, data acquisition/interpretation. Drafted and revised critically for important intellectual content. Approval final version to be publish. Agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. ALM, MD: substantially contributed to the design, data acquisition/interpretation. Drafted and revised critically for important intellectual content. Approval final version to be publish. Agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Connor Zale, Dr. Evan Fene, Dr. Claire Bonnyman, and Ms. Lydia Klinkerman have no relevant financial or non-financial interests to disclosure. Dr. Amy L McIntosh has no competing interests to declare that are relevant to the content of the article, however, does report being a paid speaker for NuVasive.
Ethical approval
Approval was granted for this study by our institution’s IRB, UT Southwestern (Study ID: 022017-011). This research study was conducted retrospectively from data obtained for clinical purposes.
Consent to participate
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zale, C., Fene, E., Bonnyman, C. et al. Aborted AIS spinal fusion due to persistent loss of IONM: which patients are at greatest risk?. Spine Deform 12, 681–687 (2024). https://doi.org/10.1007/s43390-024-00831-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-024-00831-0