Abstract
Purpose
The aim of this study is to determine preoperative predictors of good radiographic outcomes in VBT patients at a minimum 2-year follow-up.
Methods
From a single-center dataset, we reviewed patients who underwent VBT from January 2014 to November 2018. Data analysis included age, gender, Risser grade and biometric data. Radiographically, maximum Cobb angle, C-DAR and apical vertebral and disc wedging were measured preop and at a minimum 2-year follow-up. Patients were divided into two cohorts following two different outcome measures: (1) vertebral growth modulation, those patients that growth modulated or corrected ≥ 5° and those who did not; and (2) Maximum Cobb angle at 2 years, < and ≥ 40°. Student T and Chi2 tests were used for comparison and a multiple linear correlation test was implemented between statistically significant variables.
Results
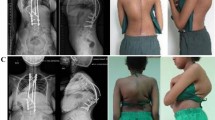
79 patients were recruited. 26 patients (33%) did growth modulate their spine at 2-year follow-up. These patients were significantly younger, and more skeletally immature with less height (147 cm vs 155 cm; p < 0.0001), weight (38 kg vs. 45 kg; p = 0.0009) and BMI (17 vs 18.8; p = 0.0229) as those who did not. Multiple linear regression model with these variables resulted in a moderate correlation (r2 = 0.234). 67 patients (85%) finished at a 2-year follow-up with a maximum Cobb angle < 40°. These patients were also younger and skeletally immature. We found significant differences in outcome 2 regarding the average preoperative maximum Cobb angle (48.5° ± 9.5 vs. 59.1° ± 10), average C-DAR (7 ± 1.5 vs. 8.5 ± 2.1), average apical vertebral wedging (6.5° vs. 8.3°), average vertebral/disc wedging ratio (1.5 vs. 2.4) and the average immediate postoperative Cobb angle (25° vs. 38°). These variables predicted a 36% of the variation in final Cobb angle measurement at a 2-year follow-up (r2 = 0.362).
Conclusion
Curve severity determined by a preoperative C-DAR, preoperative Cobb angles and immediate postoperative Cobb angle are significantly related to curves < 40° at a minimum 2-year follow-up, while the potential to growth modulate the spine is more dependent on skeletal maturity, lower body weight and lower BMI. These patients’ characteristics should be considered preoperatively.


Similar content being viewed by others
Data availability
Measurements and analysis done at the CHU Sainte-Justine are on a password protected server. Access may be arranged through application to the REB.
References
Newton PO, Faro FD, Farnsworth CL et al (2005) Multilevel spinal growth modulation with an anterolateral flexible tether in an immature bovine model. Spine (Phila Pa 1976) 30:2608–2613
Samdani AF, Ames RJ, Kimball JS, Pahys JM, Grewal H, Pelletier GJ, Betz RR (2014) Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine (Phila Pa 1976) 39(20):1688–1693. https://doi.org/10.1097/BRS.0000000000000472
Newton PO, Kluck DG, Saito W, Yaszay B, Bartley CE, Bastrom TP (2018) Anterior spinal growth tethering for skeletally immature patients with scoliosis: a retrospective look two to four years postoperatively. J Bone Jt Surg Am 100(19):1691–1697. https://doi.org/10.2106/JBJS.18.00287
Crawford CH, Lenke LG (2010) Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: a case report. J Bone Jt Surg Am 92:202–209
Newton PO (2020) Spinal growth tethering: indications and limits. Ann Transl Med 8:27
Pereira Duarte M, Aubin CE, Cobetto N, Roy-Beaudry M, Bellefleur C, Turgeon I, Labelle H, Guy A, Barchi S, Parent S (2022) 3D radiological outcomes and quality of life of patients with moderate idiopathic scoliosis treated with anterior vertebral growth modulation vs bracing: 2-year follow-up. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0000000000004335
Alanay A, Yucekul A, Kindan P, Tanriover HH, Zulemyan T, Ergene G, Senay S, Ay B, Yavuz Y, Yilgor C (2019) Thoracoscopic vertebral body tethering for adolescent idiopathic scoliosis: minimum 2 years results of patients reaching skeletal maturity. In: Presented at the annual meeting of Eurospine, Helsinki, 2019
Parent S, Alzakri A, Roy-Beaudry M, Turgeon I, Beauséjour M, Turcot O. (2019). Surgical complications of anterior vertebral body growth modulation for skeletally immature patients with idiopathic scoliosis. In: Presented at the annual meeting of Eurospine, Helsinki, 2019
Mishreky A, Parent S, Miyanji F, Smit K, Murphy J, Bowker R, Al Khatib N, El-Hawary R, Pediatric Spine Study Group (2022) Body mass index affects outcomes after vertebral body tethering surgery. Spine Deform. 10(3):563–571. https://doi.org/10.1007/s43390-021-00455-8
Zuckerman SL, Lenke LG, Cerpa M, Kelly MP, Yaszay B, Sponseller P, Erickson M, Garg S, Pahys J, Cahill P, Sides B, Gupta M, Fox Pediatric Spinal Deformity Study Group (2021) Interobserver and intraobserver reliability of determining the deformity angular ratio in severe pediatric deformity curves. Spine Deform 9(2):435–440. https://doi.org/10.1007/s43390-020-00239-6. (Epub 2020 Nov 17)
Harrington PR (1962) Treatment of scoliosis. JBJS 44A:591–610
Wang XB, Lenke LG, Thuet E, Blanke K, Koester LA, Roth M (2016) Deformity angular ratio describes the severity of spinal deformity and predicts the risk of neurologic deficit in posterior vertebral column resection surgery. Spine (Phila Pa 1976) 41(18):1447–1455. https://doi.org/10.1097/BRS.0000000000001547
CDC (2000) Centers for Disease Control and Prevention BMI-for-age charts, United States. https://www.cdc.gov/growthcharts/clinical_charts.htm. Accessed 8 Mar 2021
Modi HN, Suh SW, Song HR, Yang JH, Kim HJ, Modi CH (2008) Differential wedging of vertebral body and intervertebral disc in thoracic and lumbar spine in adolescent idiopathic scoliosis—a cross sectional study in 150 patients. Scoliosis 3:11. https://doi.org/10.1186/1748-7161-3-11
Hoernschemeyer DG, Boeyer ME, Robertson ME, Loftis CM, Worley JR, Tweedy NM, Gupta SU, Duren DL, Holzhauser CM, Ramachandran VM (2020) Anterior vertebral body tethering for adolescent scoliosis with growth remaining: a retrospective review of 2 to 5-year postoperative results. J Bone Jt Surg Am 102(13):1169–1176. https://doi.org/10.2106/JBJS.19.00980
Newton PO, Bartley CE, Bastrom TP et al (2020) Anterior spinal growth modulation in skeletally immature patients with idiopathic scoliosis. J Bone Jt Surg 102:769–777. https://doi.org/10.2106/jbjs.19.01176
Weinstein SL (1986) Idiopathic scoliosis. Natural history. Spine (Phila Pa 1976) 11(8):780–783. https://doi.org/10.1097/00007632-198610000-00006
Stokes IAF (2002) Mechanical effects on skeletal growth. J Musculoskelet Neuronal Interact 2:277–280
Lee BH, Hyun SJ, Han S, Jeon SI, Kim KJ, Jahng TA, Kim HJ (2018) Total deformity angular ratio as a risk factor for complications after posterior vertebral column resection surgery. J Korean Neurosurg Soc 61(6):723–730. https://doi.org/10.3340/jkns.2018.0125
Lewis ND, Keshen SG, Lenke LG, Zywiel MG, Skaggs DL, Dear TE, Strantzas S, Lewis SJ (2015) The deformity angular ratio: does it correlate with high-risk cases for potential spinal cord monitoring alerts in pediatric 3-column thoracic spinal deformity corrective surgery? Spine (Phila Pa 1976) 40(15):E879–E885. https://doi.org/10.1097/BRS.0000000000000984
Parent S, Labelle H, Skalli W, de Guise J (2004) Vertebral wedging characteristic changes in scoliotic spines. Spine (Phila Pa 1976) 29(20):E455–E462. https://doi.org/10.1097/01.brs.0000142430.65463.3a
Nault ML, Mac-Thiong JM, Roy-Beaudry M, deGuise J, Labelle H, Parent S (2013) Three-dimensional spine parameters can differentiate between progressive and nonprogressive patients with AIS at the initial visit: a retrospective analysis. J Pediatr Orthop 33(6):618–623. https://doi.org/10.1097/BPO.0b013e318292462a
Taylor TK, Ghosh P, Bushell GR (1981) The contribution of the intervertebral disk to the scoliotic deformity. Clin Orthop 156:79–90
Braun JT, Ogilvie JW, Akyuz E, Brodke DS, Bachus KN, Stefko RM (2003) Experimental scoliosis in an immature goat model: a method that creates idiopathic-type deformity with minimal violation of the spinal elements along the curve. Spine 28:2198–2203
Perdriolle R, Becchetti S, Vidal J, Lopez P (1993) Mechanical process and growth cartilages. Essential factors in the progression of scoliosis. Spine 18:343–349
Xiong B, Sevastik JA, Hedlund R, Sevastik B (1994) Radiographic changes at the coronal plane in early scoliosis. Spine 19:159–164
Reem J, Carney J, Stanley M, Cassidy J (2009) Risser sign inter-rater and intra-rater agreement: is the Risser sign reliable? Skeletal Radiol 38(4):371–375. https://doi.org/10.1007/s00256-008-0603-8
Funding
Bourse de jumelage de fonds du CHU Sainte-Justine.
Author information
Authors and Affiliations
Contributions
Design of the work: J-MM-T, HL, SP. Data acquisition: MP-D, MR-B, IT, JJ, SB. Analysis interpretation of data: MP-D, MR-B, HL, SB, SP. Drafting the work: MP-D, SB, SP. Critical revisión, final approval, agree to be accountable for all aspects of the work: MP-D, MR-B, IT, JJ, J-MM-T, HL, SB, SP. Supervision: SB.
Corresponding author
Ethics declarations
Conflict of interest
MPD, MRB, IT, JJ, and SB declare that they have no conflict of interest. JMMT has received a peer-reviewed grant from the Natural Sciences and Engineering Research Council of Canada (industrial research chair program with Medtronic of Canada) related to the work, and other funds not related to the work (i.e. Discovery grant from the Natural Sciences and Engineering Research Council of Canada, grant from the Canada First Research Excellence Funds, and development contracts with Medtronic Spine and Biologics through the university Polytechnique Montreal); HL is he is Co-founder of the company Spinologics Inc, SP has received outside the submitted work: royalties from EOS imaging, he is Co-founder of the company Spinologics Inc., he received consultancy fees from K2M, Medtronic and DePuy Synthes Spine, he received grants from DePuy Synthes Spine, Canadian Institutes of Health Research, Pediatric Orthopaedic Society of North America, Scoliosis Research Society, Medtronic, EOS imaging, Canadian Foundation for Innovation, Setting Scoliosis Straight Foundation, Natural Sciences and Engineering Council of Canada, Fonds de recherche Québec—Santé, grants and Orthopaedic Research and Education Foundation, he received fellowship support from DePuy Synthes and Medtronic, he is the holder of the Academic Chair in Pediatric Spinal Deformities of CHU Ste-Justine, he is member of speaker bureau of Orthopaediatrics.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the ethics Committee of the CHU Sainte-Justine.
Consent to participate
All research participants or their legal guardians provided written consent to be a part of the database and have the data collected be used in ongoing research on scoliosis.
Consent for publication
We obtained consent from the responsible authorities to submit this scientific work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pereira-Duarte, M., Roy-Beaudry, M., Turgeon, I. et al. Pre-operative parameters influencing vertebral body tethering outcomes: patient’s characteristics play an important role in determining the outcomes at a minimum of 2 years post-op. Spine Deform 11, 1389–1397 (2023). https://doi.org/10.1007/s43390-023-00739-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00739-1