Abstract
Purpose
To biomechanically evaluate 3D corrective forces and deformity correction attributable to key parameters of rod contouring in posterior spinal fusion (PSF) for adolescent idiopathic scoliosis (AIS).
Methods
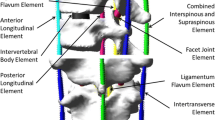
Computerised patient-specific biomechanical models of six AIS cases were used to simulate PSF and evaluate the effects of 5.5-mm cobalt-chrome rod contouring angle (concave–convex angles: 30°−15°, 45°−15° and 60°−15°), length (spanning 4 and 7 vertebrae), and apex location (T7, T9). 3D correction and bone-implant forces were computed and analysed.
Results
By increasing the concave rod contour from 30° to 60°, thoracic kyphosis (TK) increased from 18° ± 2° (15°−19°) to 24° ± 2° (22°−26°), apical vertebra rotation (AVR) correction increased from 41% (SD8%) to 66% (SD18%) whilst the main thoracic curve (MT) correction decreased from 68% (SD6%) to 56% (SD8%). With a contouring length of 4 vs. 7 vertebrae, the resulting TK, AVR and MT corrections were 22° ± 1° (19°−26°) vs. 19° ± 10° (15°−22°), 57% (SD18%) vs. 50% (SD26%) and 59% (SD1%) vs. 69% (SD35%), respectively. With the rod contouring apex at T7 (vs. T9), AVR corrections were 69% (SD19%) vs. 44% (SD9%), with no significant difference in TK and MT corrections, and with comparatively 67% of screw pull-out forces. Corrective forces were more evenly shared with fixation on 7 vs. 4 vertebrae.
Conclusion
Rod contouring of a greater angulation, over a shorter portion of the rod, and more centred at the apex of the main thoracic curve apex improved AVR correction and allowed greater restoration of TK, but resulted in significantly higher screw pull-out forces and came at the expense of less coronal plane correction.







Similar content being viewed by others
Data availability
Not applicable for this study.
References
Sucato DJ (2010) Management of severe spinal deformity: scoliosis and kyphosis. Spine 35(25):2186–2192
Zuckerman SL et al (2022) Three-dimensional assessment of vertebral derotation in adolescent idiopathic scoliosis: review of a surgical technique and its success in achieving derotation in the instrumented and uninstrumented spine. Oper Neurosurg 22(6):380–386
Ruwald JM et al (2020) An overview of the current state of pediatric scoliosis management. Z Orthop Unfall 158(5):508–516
Wang X et al (2016) How does differential rod contouring contribute to 3-dimensional correction and affect the bone-screw forces in adolescent idiopathic scoliosis instrumentation? Clin Biomech 39:115–121
Seki S et al (2019) Differential rod contouring on thoracolumbar/lumbar curvature in patients with adolescent idiopathic scoliosis: an analysis with intraoperative acquisition of three-dimensional imaging. J Orthop Sci 24(5):780–786
Le Naveaux F et al (2017) 3D rod shape changes in adolescent idiopathic scoliosis instrumentation: how much does it impact correction? Eur Spine J 26(6):1676–1683
Le Naveaux F et al (2016) How does implant distribution affect 3D correction and bone-screw forces in thoracic adolescent idiopathic scoliosis spinal instrumentation? Clin Biomech 39:25–31
La Barbera L, Larson AN, Aubin CE (2021) How do spine instrumentation parameters influence the 3D correction of thoracic adolescent idiopathic scoliosis? A patient-specific biomechanical study. Clin Biomech 84:105346
Cheriet F et al (2007) A novel system for thE 3-D reconstruction of the human spine and rib cage from biplanar X-ray images. IEEE Trans Biomed Eng 54(7):1356–1358
Delorme S et al (2003) Assessment of the 3-d reconstruction and high-resolution geometrical modeling of the human skeletal trunk from 2-D radiographic images. IEEE Trans Biomed Eng 50(8):989–998
Panjabi MM, Brand RA Jr, White AA 3rd (1976) Three-dimensional flexibility and stiffness properties of the human thoracic spine. J Biomech 9(4):185–192
Panjabi MM et al (1994) Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load-displacement curves. J Bone Joint Surg Am 76(3):413–424
Watkins R et al (2005) Stability provided by the sternum and rib cage in the thoracic spine. Spine 30(11):1283–1286
Aubin CE et al (2008) Preoperative planning simulator for spinal deformity surgeries. Spine 33(20):2143–2152
Petit Y, Aubin CE, Labelle H (2004) Patient-specific mechanical properties of a flexible multi-body model of the scoliotic spine. Med Biol Eng Comput 42(1):55–60
Cui G et al (2012) Morphologic evaluation of the thoracic vertebrae for safe free-hand pedicle screw placement in adolescent idiopathic scoliosis: a CT-based anatomical study. Surg Radiol Anat 34(3):209–216
Kim YJ et al (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine 29(3):333–342
Wang X et al (2012) Biomechanical analysis of 4 types of pedicle screws for scoliotic spine instrumentation. Spine 37(14):E823–E835
Newton PO et al (2015) Defining the “three-dimensional sagittal plane” in thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am 97(20):1694–1701
Bachmann KR et al (2019) A three-dimensional analysis of scoliosis progression in non-idiopathic scoliosis: is it similar to adolescent idiopathic scoliosis? Childs Nerv Syst 35(9):1585–1590
Hayashi K et al (2009) Three-dimensional analysis of thoracic apical sagittal alignment in adolescent idiopathic scoliosis. Spine 34(8):792–797
Acknowledgements
This project was funded by the Natural Sciences and Engineering Research Council of Canada (PCIPJ-346145-2011; Industrial Research chair with Medtronic of Canada).
Funding
This research was funded by the Natural Sciences and Engineering Research Council of Canada, PCIPJ-346145-2011, Carl-Eric Aubin.
Author information
Authors and Affiliations
Contributions
MG: simulations, analysis, interpretation of data for the work, drafting, final approbation, agree to be accountable. XW: design, simulations, analysis, interpretation of the data for the work, drafting work, revising, final approbation, agree to be accountable. TR: interpretation of the data for the work, revising, final approbation, agree to be accountable. LF: interpretation of the data for the work, revising, final approbation, agree to be accountable. RS: recruitment of cases, interpretation of the data for the work, revising, final approbation, agree to be accountable. CÉA: design, supervising the study, interpretation of the data for the work, comprehensive review, final approbation, agree to be accountable.
Corresponding author
Ethics declarations
Conflict of interest
Marine Gay and Xiaoyu Wang: supported by the Natural Sciences and Engineering Research Council of Canada (Industrial Research Chair with Medtronic of Canada). Richard M. Schwend: consultant for Orthopediatrics (outside the scope of the study). Todd Ritzman: grant/research support and consultant for Medtronic, honorarium from Stryker/K2M Spine and stock/shareholder for Apto Orthopaedics (all outside the scope of the study). Lorena Floccari: none. Carl-Éric Aubin: supported by the Natural Sciences and Engineering Research Council of Canada (Industrial Research Chair with Medtronic Canada), and consultant for Medtronic (outside the scope of the study).
Ethical approval
Approval was obtained from the ethics committees of the participating hospitals and of Polytechnique Montreal. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
Informed consents from the patients and parents were obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gay, M., Wang, X., Ritzman, T. et al. Biomechanical analysis of rod contouring in posterior spinal instrumentation and fusion for 3D correction of adolescent idiopathic scoliosis. Spine Deform 11, 1309–1316 (2023). https://doi.org/10.1007/s43390-023-00707-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00707-9