Abstract
Purpose
This retrospective cohort study compared postoperative as-needed (PRN) opioid consumption pre and postimplementation of a perioperative multimodal analgesic injection composed of ropivacaine, epinephrine, ketorolac, and morphine in patients undergoing posterior spinal fusion (PSF) for adolescent idiopathic scoliosis (AIS). Secondary outcomes include pain score measurements, time to ambulation, length of stay, blood loss, 90-day complication rate, operating room time, nonopioid medication usage, and total inpatient medication cost before and after the initiation of this practice.
Methods
Consecutive patients weighing ≥ 20 kg who underwent PSF for a primary diagnosis of AIS between January 2017 and December 2020 were included. Data from 2018 were excluded to account for standardization of the practice. Patients treated in 2017 only received PCA. Patients treated in 2019 and 2020 only received the injection. Excluded were patients who had any diagnoses other than AIS, allergies to any of the experimental medications, or who were nonambulatory. Data were analyzed utilizing the two-sample t-test or Chi-squared test as appropriate.
Results
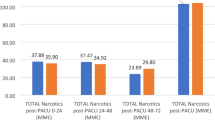
Results of this study show that compared with 47 patients treated postoperatively with patient-controlled analgesia (PCA), 55 patients treated with a multimodal perioperative injection have significantly less consumption of PRN morphine equivalents (0.3 mEq/kg vs. 0.5 mEq/kg; p = 0.02). Furthermore, patients treated with a perioperative injection have significantly higher rates of ambulation on postoperative day 1 compared with those treated with PCA (70.9 vs. 40.4%; p = 0.0023).
Conclusion
Administration of a perioperative injection is effective and should be considered in the perioperative protocol in patients undergoing PSF for AIS.
Level of Evidence
Therapeutic Level III.

Similar content being viewed by others
Data availability
The deidentified data that support the findings of this study could be made available from the corresponding author upon reasonable request.
References
Ma HH, Chou TA, Tsai SW et al (2019) The efficacy of intraoperative periarticular injection in total hip arthroplasty: a systematic review and meta-analysis. BMC Musculoskelet Disord 20(1):269. https://doi.org/10.1186/s12891-019-2628-7
Sreedharan Nair V, Ganeshan Radhamony N, Rajendra R et al (2019) Effectiveness of intraoperative periarticular cocktail injection for pain control and knee motion recovery after total knee replacement. Arthroplast Today 5(3):320–324. https://doi.org/10.1016/j.artd.2019.05.004
Ross JA, Greenwood AC, Sasser P 3rd et al (2017) Periarticular injections in knee and hip arthroplasty: where and what to inject. J Arthroplasty 32(9S):S77–S80. https://doi.org/10.1016/j.arth.2017.05.003
Pepper AM, Mercuri JJ, Behery OA et al (2018) Total hip and knee arthroplasty perioperative pain management: what should be in the cocktail. JBJS Rev 6(12):e5. https://doi.org/10.2106/JBJS.RVW.18.00023
Suarez JC, Al-Mansoori AA, Kanwar S et al (2018) Effectiveness of novel adjuncts in pain management following total knee arthroplasty: a randomized clinical trial. J Arthroplasty 33(7S):S136–S141. https://doi.org/10.1016/j.arth.2018.02.088
Amy MIL, McLeod C (2022) Local infiltration anesthesia with liposomal bupivacaine decreases postoperative narcotic consumption in AIS. JPOSNA 4(2):1–6. https://doi.org/10.55275/JPOSNA-2022-0024
Schroer WC, Diesfeld PG, LeMarr AR et al (2015) Does extended-release liposomal bupivacaine better control pain than bupivacaine after total knee arthroplasty (TKA)? A prospective, randomized clinical trial. J Arthroplasty 30(9 Suppl):64–67. https://doi.org/10.1016/j.arth.2015.01.059
Bagsby DT, Ireland PH, Meneghini RM (2014) Liposomal bupivacaine versus traditional periarticular injection for pain control after total knee arthroplasty. J Arthroplasty 29(8):1687–1690. https://doi.org/10.1016/j.arth.2014.03.034
Zhang Y, Mi F, Zhao H et al (2019) Effect of morphine added to multimodal cocktail on infiltration analgesia in total knee arthroplasty: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 98(41):e17503. https://doi.org/10.1097/MD.0000000000017503
Zhao X, Qin J, Tan Y et al (2015) Efficacy of steroid addition to multimodal cocktail periarticular injection in total knee arthroplasty: a meta-analysis. J Orthop Surg Res 10:75. https://doi.org/10.1186/s13018-015-0214-8
Fu P, Wu Y, Wu H et al (2009) Efficacy of intra-articular cocktail analgesic injection in total knee arthroplasty—a randomized controlled trial. Knee 16(4):280–284. https://doi.org/10.1016/j.knee.2008.12.012
Yue DB, Wang BL, Liu KP et al (2013) Efficacy of multimodal cocktail periarticular injection with or without steroid in total knee arthroplasty. Chin Med J (Engl) 126(20):3851–3855
Deng Z, Li Y, Storm GR et al (2019) The efficiency and safety of steroid addition to multimodal cocktail periarticular injection in knee joint arthroplasty: a meta-analysis of randomized controlled trials. Sci Rep 9(1):7031. https://doi.org/10.1038/s41598-019-43540-9
Kong DY, Oh JH, Choi WR et al (2020) The impact of epinephrine in the periarticular injection cocktail using ropivacaine for total knee arthroplasty: a prospective, randomized, double-blind comparison study. J Arthroplasty 35(9):2439–2443. https://doi.org/10.1016/j.arth.2020.04.042
Ren Z, Li Z, Li S et al (2019) Local infiltration with cocktail analgesics during 2 level lumbar spinal fusion surgery: Study protocol of a randomized controlled trial. Medicine (Baltimore) 98(19):e15526. https://doi.org/10.1097/MD.0000000000015526
Mazy A, Elmaadawy AEA, Serry M et al (2019) High-volume, multilevel local anesthetics-epinephrine infiltration in kyphoscoliosis surgery: blood conservation. Anesth Essays Res 13(3):405–410. https://doi.org/10.4103/aer.AER_89_19
Spangehl MJ, Clarke HD, Hentz JG et al (2015) The Chitranjan Ranawat Award: periarticular injections and femoral & sciatic blocks provide similar pain relief after TKA: a randomized clinical trial. Clin Orthop Relat Res 473(1):45–53. https://doi.org/10.1007/s11999-014-3603-0
Singhal NR, Jones J, Semenova J et al (2016) Multimodal anesthesia with the addition of methadone is superior to epidural analgesia: a retrospective comparison of intraoperative anesthetic techniques and pain management for 124 pediatric patients undergoing the Nuss procedure. J Pediatr Surg 51(4):612–616. https://doi.org/10.1016/j.jpedsurg.2015.10.084
Sink EL, Leunig M, Zaltz I et al (2012) Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res 470(8):2220–2226. https://doi.org/10.1007/s11999-012-2343-2
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Nelson KL, Locke LL, Rhodes LN et al (2020) Evaluation of outcomes before and after Implementation of a standardized postoperative care pathway in pediatric posterior spinal fusion patients. Orthop Nurs 39(4):257–263. https://doi.org/10.1097/NOR.0000000000000678
LeRoy TE, Moon AS, Gedman M et al (2021) Impact of body mass index on opioid consumption in lumbar spine fusion surgery. N Am Spine Soc J 6:100060. https://doi.org/10.1016/j.xnsj.2021.100060
Wang Y, Zhou A (2020) A new improvement: subperiosteal cocktail application to effectively reduce pain and blood loss after total knee arthroplasty. J Orthop Surg Res 15(1):33. https://doi.org/10.1186/s13018-020-1563-5
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
AMP, SK, KK: Made substantial contributions to the acquisition and interpretation of data, drafted the work, and revised it critically for important intellectual content, approved the version to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. XC: Made substantial contributions to the analysis and interpretation of data, revised the work critically for important intellectual content, approved the version to be published, and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. LNR, LLL, WCW, JRS, BWS, DDS, DMK: Made substantial contributions to the conception and design of the work, analysis, and interpretation of data, revised the work critically for important intellectual content, approved the version to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose the following declarations outside of this work. Dr. Warner: unpaid consultant for Sofamor Danek and publishing royalties from Saunders/Mosby-Elsevier and Wolters Kluwer Health; Dr. Sawyer: board/committee member for Children’s Spine Foundation and Pediatric Orthopaedic Society of North America, paid presenter for DePuy, A Johnson & Johnson Company, publishing royalties from Elsevier, and paid consultant for Orthopaediatrics; Dr. Spence: publishing royalties from Elsevier, research support from Orthopaediatrics, and board member for Pediatric Orthopaedic Society of North America; Dr. Kelly: publishing royalties from Elsevier and board/committee member for Pediatric Orthopaedic Society of North America. The authors declare no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the institutional review board of University of Tennessee Health Science Center (approval number 11-01362-XP).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Padgett, A.M., Kapoor, S., Rhodes, L.N. et al. Perioperative multimodal analgesic injection for patients with adolescent idiopathic scoliosis undergoing posterior spinal fusion surgery. Spine Deform 11, 977–984 (2023). https://doi.org/10.1007/s43390-023-00670-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00670-5