Abstract
Purpose
The aim of this study was to identify factors associated with the outpatient narcotic intake of patients following posterior spinal fusion (PSF) for adolescent idiopathic scoliosis (AIS) and to introduce a safe and effective method of disposing of unused narcotics.
Methods
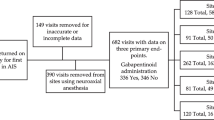
Following Institutional Review Board approval, retrospective review of prospectively collected data from patients undergoing PSF for AIS took place. Pain scores, narcotic use, patient demographic data, pre-, intra-, and postoperative parameters, and discharge data were gathered via chart review. Patients were divided into two groups according to home narcotic use, high use (top 25th percentiles) and low use (bottom 75th percentiles), and multivariate statistical analysis was conducted. Narcotic surplus was collected during postoperative clinic visits and disposed of using biodegradable bags.
Results
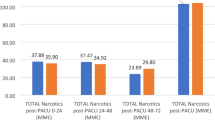
Statistical analysis of 27 patients included in the study showed that patients with a higher home narcotic use correlated with increased length of hospitalization with an average of 3.4 days compared to the lower-use group of 2.8 day (p = 0.03). Higher-use group also showed increased inpatient morphine milligram equivalent than the lower-use group. There was no significant difference of home narcotic use when looking at patient age, height, weight, BMI, levels fused, intraoperative blood loss, or length of surgery. A total of 502 narcotic doses were disposed of in the clinic.
Conclusion
Our study suggests that there are not a significant number of patient- or surgical-level factors predisposing patients to increased home narcotic usage following spinal fusion for adolescent idiopathic scoliosis.
Level of evidence
Level I, prospective study.




Similar content being viewed by others
Data availability
The data from this manuscript is available upon request.
Change history
02 March 2023
A Correction to this paper has been published: https://doi.org/10.1007/s43390-023-00673-2
References
Gibson PRJ (2004) Anaesthesia for correction of scoliosis in children. Anaesth Intensive Care 32(4):548–559. https://doi.org/10.1177/0310057X0403200413
Choudhry DK, Brenn BR, Sacks K, Shah S (2019) Evaluation of gabapentin and clonidine use in children following spinal fusion surgery for idiopathic scoliosis: a retrospective review. J Pediatr Orthop 39(9):e687–e693. https://doi.org/10.1097/BPO.0000000000000989
Grant DR, Schoenleber SJ, McCarthy AM et al (2016) Are we prescribing our patients too much pain medication?: Best predictors of narcotic usage after spinal surgery for scoliosis. J Bone Joint Surg 98(18):1555–1562. https://doi.org/10.2106/JBJS.16.00101
Bates C, Laciak R, Southwick A, Bishoff J (2011) Overprescription of postoperative narcotics: a look at postoperative pain medication delivery, consumption and disposal in urological practice. J Urol 185(2):551–555. https://doi.org/10.1016/j.juro.2010.09.088
Rodgers J, Cunningham K, Fitzgerald K, Finnerty E (2012) Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am 37(4):645–650. https://doi.org/10.1016/j.jhsa.2012.01.035
U.S. Department of Health & Human Services. Drug Overdose Deaths in the U.S. Top 100,000 Annually. Centers for Disease Control and Prevention. Published November 17, 2021. Accessed February 15, 2022. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm
U.S. Department of Health and Human Services. Highlights for the 2020 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration Accessed February 15, 2022. https://www.samhsa.gov/data/sites/default/files/2021-10/2020_NSDUH_Highlights.pdf
Lindgren AM, Bennett R, Yaszay B, Newton PO, Upasani VV (2020) Quality improvement in post-operative opioid and benzodiazepine regimen in adolescent patients after posterior spinal fusion. Spine Deform 8(3):441–445. https://doi.org/10.1007/s43390-019-00002-6
Ramos O, Speirs J, Morrison M, Danisa O (2022) Effect of narcotic prescription limiting legislation on opioid utilization following pediatric spinal fusion for scoliosis. Spine Deform 10(2):335–341. https://doi.org/10.1007/s43390-021-00406-3
Sarkisova N, Andras LM, Yang J, Tolo VT, Skaggs DL (2020) High parental anxiety increases narcotic use in adolescent patients following spinal fusion. J Pediatr Orthop 40(9):e794–e797. https://doi.org/10.1097/BPO.0000000000001549
Winsauer A, Sharma C, Bukowsky S, Greenberg S, Birch C, Ramo B. Simple measures to reduce opioid prescriptions following pediatric spinal fusion surgery: a multidisciplinary quality improvement project. JPOSNA®. 2021;3(4). Accessed August 2, 2022. https://www.jposna.org/index.php/jposna/article/view/308
Harris AB, Puvanesarajah V, Marrache M et al (2020) Correction to: Opioid prescribing practices after posterior spinal arthrodesis for adolescent idiopathic scoliosis. Spine Deform 8(5):975. https://doi.org/10.1007/s43390-020-00152-y
Khorfan R, Shallcross ML, Yu B et al (2020) Preoperative patient education and patient preparedness are associated with less postoperative use of opioids. Surgery 167(5):852–858. https://doi.org/10.1016/j.surg.2020.01.002
Yang S, Werner BC (2019) Risk factors for prolonged postoperative opioid use after spinal fusion for adolescent idiopathic scoliosis. J Pediatr Orthop 39(10):500–504. https://doi.org/10.1097/BPO.0000000000001139
Voepel-Lewis T, Caird MS, Tait AR et al (2017) A high preoperative pain and symptom profile predicts worse pain outcomes for children after spine fusion surgery. Anesth Analg 124(5):1594–1602. https://doi.org/10.1213/ANE.0000000000001963
Buffington DE, Lozicki A, Alfieri T, Bond TC (2019) Understanding factors that contribute to the disposal of unused opioid medication. J Pain Res 12:725–732
Funding
Funding was received from a QSVI grant from the Pediatric Orthopaedic Society of North America.
Author information
Authors and Affiliations
Contributions
J.G.M: acquisition of data; drafted the work; approved the version to be published; agree to be accountable for all aspects of the work. C.E.: acquisition of data; drafted the work; approved the version to be published; agree to be accountable for all aspects of the work. W.D.: analysis of data; drafted the work; approved the version to be published; agree to be accountable for all aspects of the work. A.E.: interpretation of data; critically revised the work; approved the version to be published; agree to be accountable for all aspects of the work. D.T.: substantial contributions to conception of the work; critically revised the work; approved the version to be published; agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Tuason wishes to disclose the following conflicts of interest: DePuy, A Johnson & Johnson Company: Paid consultant; Paid presenter or speaker. Globus Medical: Paid presenter or speaker. OrthoPediatrics: Paid consultant; Paid presenter or speaker. Pediatric Orthopaedic Society of North America: Board or committee member. Scoliosis Research Society: Board or committee member.
Ethics approval
Institutional review board approval was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Dr. Tuason wishes to disclose the following conflicts of interest: DePuy, A Johnson & Johnson Company: Paid consultant; Paid presenter or speaker. Globus Medical: Paid presenter or speaker. OrthoPediatrics: Paid consultant; Paid presenter or speaker. Pediatric Orthopaedic Society of North America: Board or committee member. Scoliosis Research Society: Board or committee member. Additionally, funding was received from a QSVI grant from the Pediatric Orthopaedic Society of North America.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garcia-Muñoz, J., Elblein, C., David, W.B. et al. Prospective analysis of home narcotic consumption and management of excess narcotic prescription following adolescent idiopathic scoliosis surgery. Spine Deform 11, 651–656 (2023). https://doi.org/10.1007/s43390-022-00637-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00637-y