Abstract
Purpose
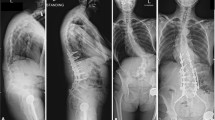
To explore the changes in health-related quality of life parameters observed in patients experiencing varying degrees of proximal junctional kyphosis following corrective adult spinal deformity fusions.
Methods
Inclusion: adult spinal deformity patients > 18 y/o, undergoing spinal fusion. PJK: ≥ 10° measure of the sagittal Cobb angle between the inferior endplate of the UIV and the superior endplate of the UIV + 2. Severe PJK: > 28° PJK. Mild PJK: ≥ 10oand ≤ 28°. ANOVA, followed by ANCOVA, compared the change in HRQoLs between time points (BL, 1Y, 2Y) among PJK groups. Correlation-related change in PJK and change in HRQoL for mild and severe groups.
Results
969 patients (age: 64.5 y/o,75% F, posterior levels fused:12.3) were studied. 59% no PJK, 32% mild PJK, 9% severe PJK. No differences in HRQoLs were seen between no PJK and PJK groups at baseline, one year, and 2 years. Adjusted analysis revealed Severe PJK patients improved less in SRS-22 Satisfaction (NoPJK: 1.6, MildPJK: 1.6, SeverePJK: 1.0; p = 0.022) scores at 2 years. Linear regression analysis only found clinical improvement in SRS-22 Satisfaction to correlate with the change of the PJK angle by 2 years (R = 0.176, P = 0.008). No other HRQoL metric correlated with either the incidence of PJK or the change in the PJK angle by one or 2 years.
Conclusions
These results maintain that patients presenting with and without proximal junctional kyphosis report similar health-related qualities of life following corrective adult spinal deformity surgery, and SRS-22 Satisfaction may be a clinical correlate to the degree of PJK. Rather than proving proximal junctional kyphosis to have a minimal clinical impact overall on HRQoL metrics, these data suggest that future analysis of this phenomenon requires different assessments.
Level of evidence
Level of evidence: III.
Similar content being viewed by others
Data availability
Data are available from the corresponding author upon request.
References
Lau D, Clark AJ, Scheer JK et al (2014) Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 39(25):2093–2102. https://doi.org/10.1097/BRS.000000000000062
Glattes RC, Bridwell KH, Lenke LG et al (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30(14):1643–1649. https://doi.org/10.1097/01.brs.0000169451.76359.49
Yagi M, King AB, Boachie-Adjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis Minimum 5 years of follow-up. Spine (Phila Pa 1976) 37(17):1479–1489. https://doi.org/10.1097/BRS.0b013e31824e4888
Kim YJ, Bridwell KH, Lenke LG et al (2008) Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 33(20):2179–2184. https://doi.org/10.1097/BRS.0b013e31817c0428
Maruo K, Ha Y, Inoue S et al (2013) Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 38(23):E1469–E1476. https://doi.org/10.1097/BRS.0b013e3182a51d43
Kim HJ, Yagi M, Nyugen J, Cunningham ME, Boachie-Adjei O (2012) Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res 470(6):1633–1639. https://doi.org/10.1007/s11999-011-2179-1
Yagi M, Akilah KB, Boachie-Adjei O (2011) Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976) 36(1):E60–E68. https://doi.org/10.1097/BRS.0b013e3181eeaee2
Lau D, Funao H, Clark AJ et al (2016) The clinical correlation of the hart-ISSG proximal junctional kyphosis severity scale with health-related quality-of-life outcomes and need for revision surgery. Spine (Phila Pa 1976) 41(3):213–223. https://doi.org/10.1097/BRS.0000000000001326
Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK (2005) Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine (Phila Pa 1976) 30(18):2045–2050. https://doi.org/10.1097/01.brs.0000179084.45839.ad
Hart RA, McCarthy I, Ames CP et al (2013) Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am 24(2):213–218. https://doi.org/10.1016/j.nec.2013.01.001
Kim HJ, Iyer S (2016) Proximal Junctional Kyphosis. J Am Acad Orthop Surg 24(5):318–326. https://doi.org/10.5435/JAAOS-D-14-00393
Yagi M, Rahm M, Gaines R et al (2014) Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine (Phila Pa 1976) 39(10):E607–E614. https://doi.org/10.1097/BRS.0000000000000266
Hassanzadeh H, Gupta S, Jain A et al (2013) Type of anchor at the proximal fusion level has a significant effect on the incidence of proximal junctional kyphosis and outcome in adults after long posterior spinal fusion. Spine Deform 1(4):299–305. https://doi.org/10.1016/j.jspd.2013.05.008
Smith JS, Klineberg E, Schwab F et al (2013) Change in classification grade by the SRS-schwab adult spinal deformity classification predicts impact on health-related quality of life measures: prospective analysis of operative and nonoperative treatment. Spine (Phila Pa 1976) 38(19):1663–1671. https://doi.org/10.1097/BRS.0b013e31829ec563
Moal B, Lafage V, Smith JS, et al (2012) Clinical improvement through surgery for adult spinal deformity (ASD): what can be expected and who is likely to benefit most? In: Proceedings of the NASS 27th Annual Meeting, vol 12. The Spine Journal, pp 99S-165S. doi: https://doi.org/10.1016/j.jspd.2015.04.004
Ostelo RWJG, de Vet HCW (2005) Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol 19(4):593–607. https://doi.org/10.1016/j.berh.2005.03.003
Albert TJ, Purtill J, Mesa J, McIntosh T, Balderston RA (1995) Health outcome assessment before and after adult deformity surgery. A prospective study. Spine (Phila Pa 1976) 20(18):2002–2004. https://doi.org/10.1097/00007632-199509150-00009
Glassman SD, Hamill CL, Bridwell KH et al (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 32(24):2764–2770. https://doi.org/10.1097/BRS.0b013e31815a7644
Emami A, Deviren V, Berven S et al (2002) Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976) 27(7):776–786. https://doi.org/10.1097/00007632-200204010-00017
Cho SK, Shin JI, Kim YJ (2014) Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J 23(12):2726–2736. https://doi.org/10.1007/s00586-014-3531-4
Schwab F, Patel A, Ungar B et al (2010) Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35(25):2224–2231. https://doi.org/10.1097/BRS.0b013e3181ee6bd4
Berthonnaud E, Dimnet J, Roussouly P, Labelle H (2005) Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 18(1):40–47. https://doi.org/10.1097/01.bsd.0000117542.88865.77
Funding
ISSG: The International Spine Study Group (ISSG) is funded through research grants from DePuy Synthes and individual donations, and supported the current work.
Author information
Authors and Affiliations
Consortia
Contributions
PP, NJF, TKW, KAM, RL, VL, JSS, KMK, DCB, RAH, CPA, SB, CIS, FJS, International Spine Study Group (ISSG): Made Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work. PP, NJF, TKW, KAM, RL, VL, JSS, KMK, DCB, RAH, CPA, SB, CIS, FJS, International Spine Study Group (ISSG): Drafted the work or revised it critically for important intellectual content. PP, NJF, TKW, KAM, RL, VL, JSS, KMK, DCB, RAH, CPA, SB, CIS, FJS, International Spine Study Group (ISSG): Approved the version to be published. PP, NJF, TKW, KAM, RL, VL, JSS, KMK, DCB, RAH, CPA, SB, CIS, FJS, International Spine Study Group (ISSG): Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy of the integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethical review committee statement
Each institution obtained approval from their local Institutional Review Board to enroll patients in the prospective database and informed consent was obtained from each patient.
Statement of approval
All authors have read and approved the manuscript and all requirements for authorship have been met by each author and each author believes the manuscript represents honest work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Passias, P.G., Frangella, N.J., Williamson, T.K. et al. Changes in health-related quality of life measures associated with degree of proximal junctional kyphosis. Spine Deform 11, 699–706 (2023). https://doi.org/10.1007/s43390-022-00607-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00607-4