Abstract
Purpose
To determine the proportions of patients returning to work at various points after adult spinal deformity (ASD) surgery and the associations between surgical invasiveness and time to return to work.
Methods
Using a multicenter database of patients treated surgically for ASD from 2008 to 2015, we identified 188 patients (mean age 51 ± 15 years) who self-reported as employed preoperatively and had 2-year follow-up. Per the ASD–Surgical and Radiographical Invasiveness Index (ASD–SR), 118 patients (63%) underwent high-invasiveness (HI) surgery (ASD–SR ≥ 100) and 70 (37%) had low-invasiveness (LI) surgery (ASD–SR < 100). Patients who self-reported ≥ 75% normal level of work/school activity were considered to be working full time. Chi-squared and Fisher exact tests were used to compare categorical variables (α = .05).
Results
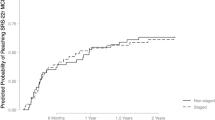
Preoperatively, 69% of employed patients worked full time. Postoperatively, 15% of employed patients were full time at 6 weeks, 70% at 6 months, 83% at 1 year, and 84% at 2 years. Percentage of employed patients working full time at 2 years was greater than preoperatively (p < .001); percentage of patients returning to full time at 6 weeks was lower in the HI (5%) than in the LI group (19%) (p = .03), a difference not significant at later points.
Conclusions
Most adults returned to full-time work after ASD surgery. A smaller percentage of patients in the HI group than in the LI group returned to full-time work at 6 weeks. Patients employed full time preoperatively will likely return to full-time employment after ASD surgery.
Level of evidence: III.

Similar content being viewed by others
References
Zygourakis CC, Liu CY, Keefe M, Moriates C, Ratliff J, Dudley RA, Gonzales R, Mummaneni PV, Ames CP (2018) Analysis of national rates, cost, and sources of cost variation in adult spinal deformity. Neurosurgery 82:378–387. https://doi.org/10.1093/neuros/nyx218
Diebo BG, Shah NV, Boachie-Adjei O, Zhu F, Rothenfluh DA, Paulino CB, Schwab FJ, Lafage V (2019) Adult spinal deformity. Lancet 394:160–172. https://doi.org/10.1016/S0140-6736(19)31125-0
Soroceanu A, Burton DC, Oren JH, Smith JS, Hostin R, Shaffrey CI, Akbarnia BA, Ames CP, Errico TJ, Bess S, Gupta MC, Deviren V, Schwab FJ, Lafage V, International Spine Study Group (2016) Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine (Phila Pa 1976) 41:1718–1723. https://doi.org/10.1097/BRS.0000000000001636
Puvanesarajah V, Rao SS, Hassanzadeh H, Kebaish KM (2018) Determinants of perioperative transfusion risk in patients with adult spinal deformity. J Neurosurg Spine 28:429–435
Riley MS, Bridwell KH, Lenke LG, Dalton J, Kelly MP (2018) Health-related quality of life outcomes in complex adult spinal deformity surgery. J Neurosurg Spine 28:194–200. https://doi.org/10.3171/2017.6.SPINE17357
Arutyunyan GG, Angevine PD, Berven S (2018) Cost-effectiveness in adult spinal deformity surgery. Neurosurgery 83:597–601. https://doi.org/10.1093/neuros/nyx575
Uddin OM, Haque R, Sugrue PA, Ahmed YM, El Ahmadieh TY, Press JM, Koski T, Fessler RG (2015) Cost minimization in treatment of adult degenerative scoliosis. J Neurosurg Spine 23:798–806. https://doi.org/10.3171/2015.3.SPINE14560
McGregor AH, Hughes SPF (2002) The evaluation of the surgical management of nerve root compression in patients with low back pain: Part 2: patient expectations and satisfaction. Spine (Phila Pa 1976) 27:1471–1476. https://doi.org/10.1097/00007632-200207010-00019 (discussion 1476-1477)
Kim EJ, Chotai S, Wick JB, Khan I, Sivaganesan A, Bydon M, Archer KR, Devin CJ (2019) Factors associated with return-to-work following cervical spine surgery in non-worker’s compensation setting. Spine (Phila Pa 1976) 44:903–907. https://doi.org/10.1097/BRS.0000000000002978
Faour M, Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU (2017) Return to work and multilevel versus single-level cervical fusion for radiculopathy in a workers’ compensation setting. Spine (Phila Pa 1976) 42:E111–E116. https://doi.org/10.1097/BRS.0000000000001713
Huysmans E, Goudman L, Van Belleghem G, De Jaeger M, Moens M, Nijs J, Ickmans K, Buyl R, Vanroelen C, Putman K (2018) Return to work following surgery for lumbar radiculopathy: a systematic review. Spine J 18:1694–1714. https://doi.org/10.1016/j.spinee.2018.05.030
Childs JD, Piva SR, Fritz JM (2005) Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 30:1331–1334. https://doi.org/10.1097/01.brs.0000164099.92112.29
Bridwell KH, Berven S, Glassman S, Hamill C, Horton WC, Lenke LG, Schwab F, Baldus C, Shainline M (2007) Is the SRS-22 instrument responsive to change in adult scoliosis patients having primary spinal deformity surgery? Spine (Phila Pa 1976) 32:2220–2225. https://doi.org/10.1097/BRS.0b013e31814cf120
Bridwell KH, Cats-Baril W, Harrast J, Berven S, Glassman S, Farcy J-P, Horton WC, Lenke LG, Baldus C, Radake T (2005) The validity of the SRS-22 instrument in an adult spinal deformity population compared with the Oswestry and SF-12: a study of response distribution, concurrent validity, internal consistency, and reliability. Spine (Phila Pa 1976) 30:455–461. https://doi.org/10.1097/01.brs.0000153393.82368.6b
Neuman BJ, Ailon T, Scheer JK, Klineberg E, Sciubba DM, Jain A, Zebala LP, Passias PG, Daniels AH, Burton DC, Protopsaltis TS, Hamilton DK, Ames CP, International Spine Study Group (2018) Development and validation of a novel adult spinal deformity surgical invasiveness score: analysis of 464 patients. Neurosurgery 82:847–853
Passias PG, Brown AE, Bortz C, Pierce K, Alas H, Ahmad W, Passfall L, Kummer N, Krol O, Lafage R, Lafage V, Burton D, Hart R, Anand N, Mundis G, Neuman B, Line B, Shaffrey C, Klineberg E, Smith J, Ames C, Schwab FJ, Bess S, International Spine Study Group (2021) A risk-benefit analysis of increasing surgical invasiveness relative to frailty status in adult spinal deformity surgery. Spine (Phila Pa 1976) 46:1087–1096. https://doi.org/10.1097/BRS.0000000000003977
Truszczyńska A, Rąpała K, Truszczyński O, Tarnowski A, Łukawski S (2013) Return to work after spinal stenosis surgery and the patient’s quality of life. Int J Occup Med Environ Health 26:394–400. https://doi.org/10.2478/s13382-013-0105-3
Krappel F, Brayda-Bruno M, Alessi G, Remacle J-M, Lopez LA, Fernández JJ, Maestretti G, Pfirrmann CWA (2017) Herniectomy versus herniectomy with the DIAM spinal stabilization system in patients with sciatica and concomitant low back pain: results of a prospective randomized controlled multicenter trial. Eur Spine J. https://doi.org/10.1007/s00586-016-4796-6
Lv Y, Chen J, Chen J, Wu Y, Chen X, Liu Y, Chu Z, Sheng L, Qin R, Chen M (2017) Three-year postoperative outcomes between MIS and conventional TLIF in1-segment lumbar disc herniation. Minim Invasive Ther Allied Technol 26:168–176. https://doi.org/10.1080/13645706.2016.1273837
Schade V, Semmer N, Main CJ, Hora J, Boos N (1999) The impact of clinical, morphological, psychosocial and work-related factors on the outcome of lumbar discectomy. Pain 80:239–249. https://doi.org/10.1016/s0304-3959(98)00210-3
Skouen JS, Larsen JL, Gjerde IO, Hegrestad SE, Vollset SE (1997) Cerebrospinal fluid protein concentrations in patients with sciatica caused by lumbar disc herniation: an investigation of biochemical, neurologic, and radiologic predictors of long-term outcome. J Spinal Disord 10:505–511
Than KD, Curran JN, Resnick DK, Shaffrey CI, Ghogawala Z, Mummaneni PV (2016) How to predict return to work after lumbar discectomy: answers from the NeuroPoint-SD registry. J Neurosurg Spine 25:181–186. https://doi.org/10.3171/2015.10.SPINE15455
Vucetic N, Astrand P, Güntner P, Svensson O (1999) Diagnosis and prognosis in lumbar disc herniation. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199904000-00016
Kim WJ, Lee JW, Hwang SY, Park KY, Chang SH, Song DG, Choy WS (2018) Activity of daily living after long level fusion in adult spinal deformity: compared with over 60-year-old degenerative spine patients without adult spinal deformity. Spine (Phila Pa 1976) 43:1638–1647. https://doi.org/10.1097/BRS.0000000000002676
Banczerowski P, Czigléczki G, Papp Z, Veres R, Rappaport HZ, Vajda J (2015) Minimally invasive spine surgery: systematic review. Neurosurg Rev 38:11–26. https://doi.org/10.1007/s10143-014-0565-3 (discussion 26)
Berjano P, Damilano M, Langella F, Pejrona M, Lamartina C (2014) Minimally invasive surgery for adult spinal deformity. J Neurosurg Sci 58:81–86
Chang P-Y, Wang MY (2016) Minimally invasive spinal deformity surgery: current state and future direction. Neurosurgery 63(Suppl 1):43–51. https://doi.org/10.1227/NEU.0000000000001296
Lovecchio F, Qureshi SA (2019) The current state of minimally invasive approaches to adult spinal deformity. Curr Rev Musculoskelet Med. https://doi.org/10.1007/s12178-019-09570-6
Wewel JT, Godzik J, Uribe JS (2019) The utilization of minimally invasive surgery techniques for the treatment of spinal deformity. J Spine Surg 5:S84–S90. https://doi.org/10.21037/jss.2019.04.22
Sjolinder PO, Nota DF (1994) Early return to work following an aggressive rehabilitation program initiated one day after spine surgery. J Occup Rehabil 4:211–228. https://doi.org/10.1007/BF02331617
Khan I, Bydon M, Archer KR, Sivaganesan A, Asher AM, Alvi MA, Kerezoudis P, Knightly JJ, Foley KT, Bisson EF, Shaffrey C, Asher AL, Spengler DM, Devin CJ (2019) Impact of occupational characteristics on return to work for employed patients after elective lumbar spine surgery. Spine J 19:1969–1976. https://doi.org/10.1016/j.spinee.2019.08.007
Daniels AH, Kuris EO, Kleinhenz DT, Palumbo MA (2017) Spine surgery outcomes in workers’ compensation patients. J Am Acad Orthop Surg 25:e225–e234. https://doi.org/10.5435/JAAOS-D-16-00895
Acknowledgements
For editorial assistance, we thank Denise Di Salvo, MS, Sandra Crump, MPH, and Rachel Box, MS, in the Editorial Services group of The Johns Hopkins Department of Orthopaedic Surgery. The International Spine Study Group: Behrooz Akbarnia, MD, SDS, emeritus; Christopher Ames, MD, UCSF, core member; Neel Anand, MD, CED, participant; Shay Bess, MD, COL, core member; Oheneba Boachie-Adjei, MD, HSS, emeritus; Keith Bridwell, MD, WUN, collaborator; Douglas Burton, MD, KS, core member; Dean Chou, MD, USF, participant; Cunningham, HSS, corresponding associate; Alan Daniels, MD, BU, collaborator; Vedat Deviren, MD, USF, participant; Robert Eastlack, MD, SDS, participant; Richard Fessler, MD, RUM, participant; Steven Glassman, MD, NLS, collaborator; Jeffrey Gum, MD, NLS, participant; Munish Gupta, MD, WUN, core member; D. Kojo Hamilton, MD, UPM, participant; Robert Hart, MD, OHS, core member; Naobumi Hosogane, MD, PHD, JPN, collaborator; Richard Hostin, MD, BSC, core member; Yashar Javidan, MD, UCD, corresponding associate; Kai Ming Fu, MD, NYC, corresponding associate; Adam Kanter, MD, FAANS, UPM, participant; Khaled Kebaish, MD, JHU, core member; Michael Kelly, MD, WUN, participant; Han Jo Kim, MD, HSS, core member; Eric Klineberg, MD, UCD, core member; Renaud Lafage, MSc, HSS, collaborator; Virginie Lafage, PhD, HSS, core member; Lawrence Lenke, MD, CU, participant; Breton Line, BS, COL, collaborator; Praveen Mummaneni, MD, UCSF, participant; Gregory Mundis, MD, SDS, core member; Brian Neuman, MD , JHU, corresponding associate; Pierce Nunley, MD, LOU, participant; David Okonkwo, MD, UPM, participant; Paul Park, MD, UMI, participant; Peter Passias, MD, NYU, participant; Themistocles Protopsaltis, MD, NYU, participant; Justin Scheer, MD, UCI, collaborator; Frank Schwab, MD, HSS, core member; Daniel Sciubba, MD, JHU, corresponding associate; Christopher Shaffrey, MD, UVA, core member; Justin S. Smith, MD, PhD, UVA, core member; Alexandra Soroceanu, MD, MPH, UCA, participant; Tamir Ailon, MD, VANC, corresponding associate; Khoi Than, MD, OHS, participant; Juan Uribe, MD, BNI, participant; Michael Wang, MD, UMF, participant; Mitsuru Yagi, MD, PhD, JPN, collaborator; Samrat Yeramaneni, MBBS, MS, PhD, BSC, collaborator.
Funding
DePuy Synthes Spine; NuVasive; K2M/Stryker; Biomet; Orthofix; Allosource; SI Bone.
Author information
Authors and Affiliations
Consortia
Contributions
BJN: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. KYW: acquisition of data; drafting the article; final approval of the version to be published; agreement to be accountable for all aspects of the work; analysis. ABH: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work; analysis. MR: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. RH: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. TP: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. CA: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. PP: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. MG: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. EOK: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. RH: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. SB: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. KMK: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work. International Spine Study Group: acquisition of data; substantial contributions to conception and design; revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethics approval
The study was approved by the institutional review board at each participating institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The Members of The International Spine Study Group are listed in Acknowledgements.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Neuman, B.J., Wang, K.Y., Harris, A.B. et al. Return to work after adult spinal deformity surgery. Spine Deform 11, 197–204 (2023). https://doi.org/10.1007/s43390-022-00552-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00552-2