Abstract
Purpose
To compare the incidence, timing, and microbiologic factors associated with late spinal infection (onset ≥ 6 months after index operation) in pediatric versus adult spinal deformity patients who underwent instrumented posterior spinal fusion (PSF).
Methods
We retrospectively queried our institutional database for pediatric (aged ≤ 21 years) and adult patients who underwent instrumented PSF from 2000 to 2015. Inclusion criteria were > 12-month follow-up, spinal arthrodesis spanning 4 or more levels, and idiopathic or degenerative spinal deformity. We included 1260 patients (755 pediatric, 505 adult). Incidence, timing, and microbiologic and operative parameters of late spinal infections were compared using chi-squared and Fisher exact tests. Alpha = 0.05.
Results
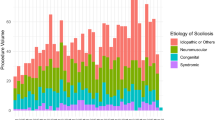
Late spinal infection occurred in 28 (3.7%) pediatric and 2 (0.39%) adult patients (p = 0.009). Mean onset of infection was 4.2 years (range 0.7–12) in pediatric patients and 4.0 years (range 0.7–7.3) in adults (p = 0.93). Pediatric patients underwent arthrodesis spanning more levels (mean ± standard deviation, 10 ± 2.0) compared with adults (8.4 ± 3.3) (p < 0.001). Adults experienced greater intraoperative blood loss (2085 ± 1491 mL) compared with pediatric patients (796 ± 452 mL) (p < 0.001). Culture samples yielded positive growth in 11 pediatric and 2 adult cases. Propionibacterium and coagulase-negative staphylococci were the most commonly detected microorganisms in both cohorts.
Conclusion
Late spinal infections were significantly more common in pediatric patients than in adults after instrumented PSF for spinal deformity. Skin and indolent microorganisms were the primary identifiable causative bacteria in both cohorts.
Level of evidence
III.

Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Kalfas F, Severi P, Scudieri C (2019) Infection with spinal instrumentation: a 20-year, single-institution experience with review of pathogenesis, diagnosis, prevention, and management. Asian J Neurosurg 14:1181–1189. https://doi.org/10.4103/ajns.AJNS_129_19
Haidar R, Najjar M, Boghossian AD et al (2010) Propionibacterium acnes causing delayed postoperative spine infection: review. Scand J Infect Dis 42:405–411. https://doi.org/10.3109/00365540903582459
Aydinli U, Karaeminoğullari O, Tişkaya K (1999) Postoperative deep wound infection in instrumented spinal surgery. Acta Orthop Belg 65:182–187
Kasliwal MK, Tan LA, Traynelis VC (2013) Infection with spinal instrumentation: review of pathogenesis, diagnosis, prevention, and management. Surg Neurol Int 4:S392–S403. https://doi.org/10.4103/2152-7806.120783
Lewkonia P, DiPaola C, Street J (2016) Incidence and risk of delayed surgical site infection following instrumented lumbar spine fusion. J Clin Neurol Neurosci 23:76–80. https://doi.org/10.1016/j.jocn.2015.05.039
Richards BS (1995) Delayed infections following posterior spinal instrumentation for the treatment of idiopathic scoliosis. J Bone Joint Surg Am 77:524–529
Soultanis K, Mantelos G, Pagiatakis A, et al (2003) Late infection in patients with scoliosis treated with spinal instrumentation. Clin Orthop Relat Res 411:116–123. https://doi.org/10.1097/01.blo.0000068357.47147.10
Clark CE, Shufflebarger HL (1999) Late-developing infection in instrumented idiopathic scoliosis. Spine 24:1909
Hahn F, Zbinden R, Min K (2005) Late implant infections caused by Propionibacterium acnes in scoliosis surgery. Eur Spine J 14:783–788. https://doi.org/10.1007/s00586-004-0854-6
Viola RW, King HA, Adler SM et al (1997) Delayed infection after elective spinal instrumentation and fusion: a retrospective analysis of eight cases. Spine 22:2444–2450
Yin D, Liu B, Chang Y et al (2018) Management of late-onset deep surgical site infection after instrumented spinal surgery. BMC Surg 18:121. https://doi.org/10.1186/s12893-018-0458-4
Ho C, Sucato DJ, Richards BS (2007) Risk factors for the development of delayed infections following posterior spinal fusion and instrumentation in adolescent idiopathic scoliosis patients. Spine 32:2272–2277. https://doi.org/10.1097/BRS.0b013e31814b1c0b
Dubousset J (1994) Late infection with CD instrumentation. Orthop Trans 18:121
Richards BR, Emara KM (2001) Delayed infections after posterior TSRH spinal instrumentation for idiopathic scoliosis: revisited. Spine 26:1990–1995
De Wald RL, Arlet V, Carl AL, et al (2003) Spinal deformities: the comprehensive text. Thieme Verlag
Bose B (2003) Delayed infection after instrumented spine surgery: case reports and review of the literature. Spine J 3:394–399. https://doi.org/10.1016/S1529-9430(03)00023-8
Heggeness MH, Esses SI, Errico T et al (1993) Late infection of spinal instrumentation by hematogenous seeding. Spine 18:492–496
Robertson PA, Taylor TK (1993) Late presentation of infection as a complication of Dwyer anterior spinal instrumentation. J Spinal Disord 6:256–259. https://doi.org/10.1097/00002517-199306030-00013
Di Silvestre M, Bakaloudis G, Lolli F et al (2011) Late-developing infection following posterior fusion for adolescent idiopathic scoliosis. Eur Spine J 20:121–127. https://doi.org/10.1007/s00586-011-1754-1
Pull ter Gunne AF, van Laarhoven CJHM, Cohen DB (2010) Incidence of surgical site infection following adult spinal deformity surgery: an analysis of patient risk. Eur Spine J 19:982–988. https://doi.org/10.1007/s00586-009-1269-1
Liu J-M, Deng H-L, Chen X-Y et al (2018) Risk factors for surgical site infection after posterior lumbar spinal surgery. Spine 43:732–737. https://doi.org/10.1097/BRS.0000000000002419
Peng X-Q, Sun C-G, Fei Z-G et al (2019) Risk factors for surgical site infection after spinal surgery: a systematic review and meta-analysis based on twenty-seven studies. World Neurosurg 123:e318–e329. https://doi.org/10.1016/j.wneu.2018.11.158
Sanfilippo AM, Barrio V, Kulp-Shorten C et al (2003) Common pediatric and adolescent skin conditions. J Pediatr Adolesc Gynecol 16:269–283. https://doi.org/10.1016/s1083-3188(03)00147-5
Wright ML, Skaggs DL, Matsumoto H et al (2016) Does the type of metal instrumentation affect the risk of surgical site infection in pediatric scoliosis surgery? Spine Deform 4:206–210. https://doi.org/10.1016/j.jspd.2015.11.002
Garcia D, Mayfield CK, Leong J et al (2020) Early adherence and biofilm formation of Cutibacterium acnes (formerly Propionibacterium acnes) on spinal implant materials. Spine J 20:981–987. https://doi.org/10.1016/j.spinee.2020.01.001
da Rocha LGDO, Ribeiro VST, de Andrade AP et al (2021) Evaluation of Staphylococcus aureus and Candida albicans biofilms adherence to PEEK and titanium-alloy prosthetic spine devices. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-021-03069-y
Krätzig T, Mende KC, Mohme M et al (2021) Bacterial adhesion characteristics on implant materials for intervertebral cages: titanium or PEEK for spinal infections? Eur Spine J 30:1774–1782. https://doi.org/10.1007/s00586-020-06705-z
Watanabe K, Fukuzaki S, Sugino A et al (2021) Cobalt–chromium alloy has superior antibacterial effect than titanium alloy. Spine 46:E911–E915. https://doi.org/10.1097/BRS.0000000000003970
Patel SS, Aruni W, Inceoglu S et al (2016) A comparison of Staphylococcus aureus biofilm formation on cobalt-chrome and titanium-alloy spinal implants. J Clin Neurol Neurosci 31:219–223. https://doi.org/10.1016/j.jocn.2016.03.013
Acknowledgements
For their editorial assistance, we thank Jenni Weems, MS, Kerry Kennedy, BA, and Rachel Box, MS, in the Editorial Services group of The Johns Hopkins Department of Orthopaedic Surgery.
Funding
The authors received no financial support for the research, authorship, or publication of this article.
Author information
Authors and Affiliations
Contributions
II: data collection, writing-original draft preparation, and approval of final version of manuscript, agree to be accountable for the work. GJB: data collection, approval of final version of manuscript, agree to be accountable for the work. AM: approval of final version of manuscript, agree to be accountable for the work. AJ: approval of final version of manuscript, agree to be accountable for the work. KMK: approval of final version of manuscript, agree to be accountable for the work. PDS: writing-original draft preparation, and approval of final version of manuscript, agree to be accountable for the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
Ethics approval
This study was approved by The Johns Hopkins Medicine Institutional Review Board.
Consent to participant
Formal consent was not required for this type of study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ikwuezunma, I., Beutler, G.J., Margalit, A. et al. Late spinal infections are more common after pediatric than after adult spinal deformity surgery. Spine Deform 10, 817–823 (2022). https://doi.org/10.1007/s43390-022-00494-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00494-9