Abstract
Purpose
To determine the association of preoperative opioid prescriptions with reoperations and postoperative opioid prescriptions after adult spina deformity (ASD) surgery.
Summary of background data
With the current opioid crisis, patients undergoing surgery for ASD are at particular risk for opioid-related complications due to significant preoperative disability and surgical morbidity. No previous studies consider preoperative opioids in this population.
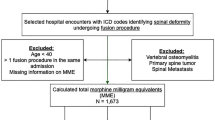
Methods
A retrospective cohort study of patients undergoing posterior spinal fusion (7 or more levels) for ASD was performed. All patients had at least 3 years of postoperative follow-up 3 years postoperatively. Prescriptions for 4 different opioid medications (hydromorphone, oxycodone, hydrocodone, and tramadol) were identified within 3 months preoperatively and up to 3 years postoperatively. Multivariate regression was utilized to determine the association of preoperative use with reoperations and with postoperative opioid use, controlling for both patient and surgery-related confounding factors.
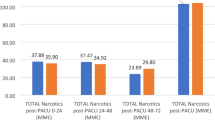
Results
A total of 743 patients were identified and 59.6% (443) had opioid prescriptions within 3 months preoperatively. Postoperative opioid prescriptions were identified in 66.9% of patients at 12 months postoperatively, and in 54.8% at 36 months postoperatively. The 3-year reoperation rate was 11.0% in patients without preoperative prescriptions, 16.0% in patients with preoperative any opioid prescriptions (P = 0.07), and 34.8% in patients with preoperative hydromorphone prescriptions (P < 0.01). In multivariate analysis, preoperative opioid prescriptions were associated with increased reoperations (odds ratio [OR]: 1.62, P = 0.04), and chronic postoperative opioid use (OR: 4.40, P < 0.01). Preoperative hydromorphone prescriptions had the strongest association with both reoperations (OR: 4.96; P < 0.01) and chronic use (OR: 5.19: P = 0.03).
Conclusion
In the ASD population, preoperative opioids are associated with both reoperations and chronic opioid use, with hydromorphone having the strongest association. Further investigation of the benefits of preoperative weaning programs is warranted.


Similar content being viewed by others
Availability of data and material
Data are publicly available.
Code availability
PearlDiver BellWeather queries available upon request.
References
Wilson N, Kariisa M, Seth P et al (2020) Drug and opioid-involved overdose deaths—United States, 2017–2018. MMWR Morb Mortal Wkly Rep 69(11):290–297. https://doi.org/10.15585/mmwr.mm6911a4
Scholl L, Seth P, Kariisa M et al (2018) Drug and opioid-involved overdose deaths—United States, 2013–2017. MMWR Morb Mortal Wkly Rep 67(5152):1419–1427. https://doi.org/10.15585/mmwr.mm675152e1
Schoenfeld AJ, Jiang W, Chaudhary MA et al (2017) Sustained prescription opioid use among previously opioid-naive patients insured through TRICARE (2006–2014). JAMA Surg 152(12):1175–1176. https://doi.org/10.1001/jamasurg.2017.2628
Jain N, Brock JL, Phillips FM et al (2018) Chronic preoperative opioid use is a risk factor for increased complications, resource use, and costs after cervical fusion. Spine J Off J N Am Spine Soc 18(11):1989–1998. https://doi.org/10.1016/j.spinee.2018.03.015
Hockley A, Ge D, Vasquez-Montes D et al (2020) Predictors of long-term opioid dependence in transforaminal lumbar interbody fusion with a focus on pre-operative opioid usage. Eur Spine J. https://doi.org/10.1007/s00586-020-06345-3
Kalakoti P, Volkmar AJ, Bedard NA et al (2019) Preoperative chronic opioid therapy negatively impacts long-term outcomes following cervical fusion surgery. Spine (Phila Pa 1976) 44(18):1279–1286. https://doi.org/10.1097/BRS.0000000000003064
Jain N, Phillips FM, Weaver T et al (2018) Preoperative Chronic opioid therapy: a risk factor for complications, readmission, continued opioid use and increased costs after one- and two-level posterior lumbar fusion. Spine (Phila Pa 1976) 43(19):1331–1338. https://doi.org/10.1097/BRS.0000000000002609
Sharma M, Ugiliweneza B, Sirdeshpande P et al (2019) Opioid dependence and health care utilization after decompression and fusion in patients with adult degenerative scoliosis. Spine (Phila Pa 1976) 44(4):280–290. https://doi.org/10.1097/BRS.0000000000002794
Pitter FT, Sikora M, Lindberg-Larsen M et al (2019) Use of opioids and other analgesics before and after primary surgery for adult spinal deformity: a 10-year nationwide study. Neurospine. https://doi.org/10.14245/ns.1938106.053
Bess S, Line B, Fu KM et al (2016) The health impact of symptomatic adult spinal deformity: comparison of deformity types to united states population norms and chronic diseases. Spine (Phila Pa 1976) 41(3):224–233. https://doi.org/10.1097/BRS.0000000000001202
Li Z, Shen J, Qiu G et al (2014) Unplanned reoperation within 30 days of fusion surgery for spinal deformity. PLoS ONE 9(3):e87172. https://doi.org/10.1371/journal.pone.0087172
Mok JM, Cloyd JM, Bradford DS et al (2009) Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine (Phila Pa 1976) 34(8):832–839. https://doi.org/10.1097/BRS.0b013e31819f2080
Anand N, Sardar ZM, Simmonds A et al (2016) Thirty-day reoperation and readmission rates after correction of adult spinal deformity via circumferential minimally invasive surgery-analysis of a 7-year experience. Spine Deform 4(1):78–83. https://doi.org/10.1016/j.jspd.2015.08.002
Opioid Oral Morphine Milligram Equivalent (MME) Conversion Factors. U.S. Centers for Medicare and Medicaid Services. 2019. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-Aug-2017.pdf
D’Hoore W, Bouckaert A, Tilquin C (1996) Practical considerations on the use of the Charlson Comorbidity Index with administrative data bases. J Clin Epidemiol 49(12):1429–1433
Okie S (2010) A flood of opioids, a rising tide of deaths. N Engl J Med 363(21):1981–1985. https://doi.org/10.1056/NEJMp1011512
Wick JB, Sivaganesan A, Chotai S et al (2018) Is there a preoperative morphine equianalgesic dose that predicts ability to achieve a clinically meaningful improvement following spine surgery? Neurosurgery 83(2):245–251. https://doi.org/10.1093/neuros/nyx382
Armaghani SJ, Lee DS, Bible JE et al (2014) Preoperative opioid use and its association with perioperative opioid demand and postoperative opioid independence in patients undergoing spine surgery. Spine (Phila Pa 1976) 39(25):E1524–E1530. https://doi.org/10.1097/BRS.0000000000000622
Lee D, Armaghani S, Archer KR et al (2014) Preoperative opioid use as a predictor of adverse postoperative self-reported outcomes in patients undergoing spine surgery. J Bone Jt Surg Am 96(11):e89. https://doi.org/10.2106/jbjs.m.00865
Hills JM, Pennings JS, Archer KR et al (2019) Preoperative opioids and 1-year patient-reported outcomes after spine surgery. Spine (Phila Pa 1976) 44(12):887–895. https://doi.org/10.1097/BRS.0000000000002964
Jain N, Brock JL, Malik AT et al (2019) Prediction of complications, readmission, and revision surgery based on duration of preoperative opioid use: analysis of major joint replacement and lumbar fusion. J Bone Jt Surg Am 101(5):384–391. https://doi.org/10.2106/JBJS.18.00502
Auerbach JD, Lenke LG, Bridwell KH et al (2012) Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 37(14):1198–1210. https://doi.org/10.1097/BRS.0b013e31824fffde
Hassanzadeh H, Jain A, El Dafrawy MH et al (2013) Three-column osteotomies in the treatment of spinal deformity in adult patients 60 years old and older: outcome and complications. Spine (Phila Pa 1976) 38(9):726–731. https://doi.org/10.1097/BRS.0b013e31827c2415
Kim SS, Cho BC, Kim JH et al (2012) Complications of posterior vertebral resection for spinal deformity. Asian Spine J 6(4):257–265. https://doi.org/10.4184/asj.2012.6.4.257
La Maida GA, Luceri F, Gallozzi F et al (2015) Complication rate in adult deformity surgical treatment: safety of the posterior osteotomies. Eur Spine J 24(Suppl 7):879–886. https://doi.org/10.1007/s00586-015-4275-5
Suk SI, Kim JH, Kim WJ et al (2002) Posterior vertebral column resection for severe spinal deformities. Spine (Phila Pa 1976) 27(21):2374–2382. https://doi.org/10.1097/00007632-200211010-00012
Angst MS, Clark JD (2006) Opioid-induced hyperalgesia: a qualitative systematic review. Anesthesiology 104(3):570–587. https://doi.org/10.1097/00000542-200603000-00025
Lee M, Silverman SM, Hansen H et al (2011) A comprehensive review of opioid-induced hyperalgesia. Pain Physician 14(2):145–161
Jain N, Himed K, Toth JM et al (2018) Opioids delay healing of spinal fusion: a rabbit posterolateral lumbar fusion model. Spine J 18(9):1659–1668. https://doi.org/10.1016/j.spinee.2018.04.012
Kelly MP, Anderson PA, Sasso RC et al (2015) Preoperative opioid strength may not affect outcomes of anterior cervical procedures: a post hoc analysis of 2 prospective, randomized trials. J Neurosurg Spine 23(4):484–489. https://doi.org/10.3171/2015.1.SPINE14985
Mazer-Amirshahi M, Ladkany D, Mullins PM et al (2018) Trends in and predictors of hydromorphone administration in US emergency departments (2007–2014). J Opioid Manag 14(4):265–272. https://doi.org/10.5055/jom.2018.0458
Dunn LK, Yerra S, Fang S et al (2018) Incidence and risk factors for chronic postoperative opioid use after major spine surgery: a cross-sectional study with longitudinal outcome. Anesth Analg 127(1):247–254. https://doi.org/10.1213/ane.0000000000003338
Kalakoti P, Hendrickson NR, Bedard NA et al (2018) Opioid utilization following lumbar arthrodesis: trends and factors associated with long-term use. Spine (Phila Pa 1976) 43(17):1208–1216. https://doi.org/10.1097/brs.0000000000002734
Wang MC, Lozen AM, Laud PW et al (2019) Factors associated with chronic opioid use after cervical spine surgery for degenerative conditions. J Neurosurg Spine. https://doi.org/10.3171/2019.7.Spine19563
Larach DB, Sahara MJ, As-Sanie S et al (2019) Patient factors associated with opioid consumption in the month following major surgery. Ann Surg. https://doi.org/10.1097/SLA.0000000000003509
Funding
No direct funding was received for this study. However, this study used REDCap (Research Electronic Data Capture) hosted at Weill Cornell Medicine Clinical and Translational Science Center supported by the National Center For Advancing Translational Science of the National Institute of Health under award number: UL1 TR002384. KWM was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under award number T32-AR078751. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by AMS, KM, and YP. The first draft of the manuscript was written by AMS, KWM, and YP and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest related to the topic of this study. AMS, KM, YP, ASV, CHG: No relevant financial or non-financial interests to disclose. HJK: Financial interests: Royalties: Zimmer Biomet, K2M; Private investments: HS2, Spine Stud; Consulting: Zimmer Biomet Holdings, K2M; Research Support: ISSG; Travel: Zimmer Biomet Holdings, Nuvasive, Inc. Innovasis, Inc. Non-financial interests: Board or committee member: AAOS, AO Spine, Cervical Spine Research Society, Scoliosis Research Society; SAQ: Financial interests: Consulting: Globus Medical, Inc., Paradigm Spine (Past relationship), Stryker K2M; Other: Simplify Medical, Inc. (Clinical Events Committee Member); Private Investments: Tissue Differentiation Intelligence, Vital 5 (Past relationship); Royalties: Globus Medical, Inc., Stryker K2M; Scientific Advisory Board: Healthgrades (Past relationship), Lifelink.Com Inc., Spinal Simplicity, LLC; Speaking and/or Teaching Arrangements: Amopportunities (Honoraria), Globus Medical, Inc. (Speakers' Bureau), RTI Surgical Inc.; Trips/Travel: Globus Medical, Inc., Integrity Implants Inc, Medical Device Business Services, Medtronic USA, Inc., Nuvasive, Inc., Paradigm Spine, Stryker K2M. Non-financial interests: Board of Directors: Society Of Minimally Invasive Spine Surgery; Editorial Board Member: Annals Of Translational Medicine, Contemporary Spine Surgery; Committee Member: Association Of Bone And Joint Surgeons, Cervical Spine Research Society, International Society For The Advancement Of Spine Surgery, Lumbar Spine Research Society, North American Spine Society, Society Of Minimally Invasive Spine Surgery; Board Member: Minimally Invasive Spine Study Group, Society Of Minimally Invasive Spine Surgery.
Ethical approval
This study was performed under an Approved Exemption by the Hospital for Special Surgery Institutional Review Board (protocol number 2020-0327).
Consent to participate
All patients signed freely given, informed consent to participate, prior to inclusion in this clinical data registry. All data were then de-identified prior to use by the study authors.
Consent for publication
All patients signed freely given, informed consent for publication, prior to inclusion in this clinical data registry. All data were then de-identified prior to use by the study authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Samuel, A.M., Morse, K.W., Pompeu, Y.A. et al. Preoperative opioids before adult spinal deformity surgery associated with increased reoperations and high rates of chronic postoperative opioid use at 3-year follow-up. Spine Deform 10, 615–623 (2022). https://doi.org/10.1007/s43390-021-00450-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00450-z