Abstract
Purpose
Retrospective observational cohort study of primary adult spinal deformity (ASD) surgery during the transitional period prior to and after the implementation of Enhanced Surgical Recovery (ESR) at a single center. We sought to determine if ESR reduces in-hospital and 90-day post-operative opioid consumption for ASD surgery.
Methods
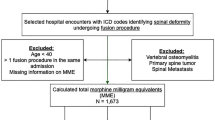
We evaluated patients undergoing primary ASD surgery in the transition period prior to (N = 29) and after (N = 56) adoption of ESR, comparing in-hospital and 90-day post-operative opioid consumption. Regression analysis was used to control for confounders including age, number of surgical levels, surgical approach, staged vs same-day surgery, insurance type and pre-op opioid use.
Results
Mean age of the cohort was 53 years with 57 (60%) females. Regression analysis showed that pre-operative opioid use and number of levels fused were associated with higher in-hospital and 90-day post-operative opioid consumption, while use of ESR was associated with lower in-hospital and 90-day post-operative opioid consumption. Secondary analysis showed that patients on ESR ambulated earlier (0.6 days vs 1.1, p = 0.028) and had their urinary catheter removed earlier (2.7 days vs 3.9, p = 0.006) compared to non-ESR patients.
Conclusions
ESR was associated with a significantly decreased in-hospital and 90-day post-operative opioid consumption and earlier mobilization with earlier urinary catheter removal in patients undergoing primary ASD surgery. These results demonstrate ESR’s potential to improve outcomes in ASD perioperative care.
Level of evidence
3.
Similar content being viewed by others
Availability of data and material
Data available upon request.
Code availability
Not applicable.
References
Hah JM, Bateman BT, Ratliff J et al (2017) Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg 125:1733–1740. https://doi.org/10.1213/ANE.0000000000002458
Naik BI, Nemergut EC, Kazemi A et al (2016) The effect of dexmedetomidine on postoperative opioid consumption and pain after major spine surgery. Anesth Analg 122:1646–1653. https://doi.org/10.1213/ANE.0000000000001226
Alam A, Gomes T, Zheng H et al (2012) Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med 172:425–430. https://doi.org/10.1001/archinternmed.2011.1827
Fearon KCH, Ljungqvist O, Von Meyenfeldt M et al (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24:466–477. https://doi.org/10.1016/j.clnu.2005.02.002
The Center for Disease Control and Prevention (2019). Calculating total daily dose of opioids for safer dosage. Retrieved from https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf
Meyer LA, Lasala J, Iniesta MD et al (2018) Effect of an enhanced recovery after surgery program on opioid use and patient-reported outcomes. Obstet Gynecol 132:281–290. https://doi.org/10.1097/AOG.0000000000002735
Clark BS, Swanson M, Widjaja W et al (2021) ERAS for head and neck tissue transfer reduces opioid usage, peak pain scores, and blood utilization. Laryngoscope 131:E792–E799. https://doi.org/10.1002/lary.28768
Soffin EM, Wetmore DS, Beckman JD et al (2019) Opioid-free anesthesia within an enhanced recovery after surgery pathway for minimally invasive lumbar spine surgery: a retrospective matched cohort study. Neurosurg Focus. https://doi.org/10.3171/2019.1.FOCUS18645
Kennedy GT, Hill CM, Huang Y et al (2020) Enhanced recovery after surgery (ERAS) protocol reduces perioperative narcotic requirement and length of stay in patients undergoing mastectomy with implant-based reconstruction. Am J Surg 220:147–152. https://doi.org/10.1016/j.amjsurg.2019.10.007
Gridley C, Robles J, Calvert J et al (2020) Enhanced recovery after surgery protocol for patients undergoing ureteroscopy: prospective evaluation of an opioid-free protocol. J Endourol 34:647–653. https://doi.org/10.1089/end.2019.0552
Movilla PR, Kokroko JA, Kotlyar AG et al (2020) Postoperative opioid use using enhanced recovery after surgery guidelines for benign gynecologic procedures. J Minim Invasive Gynecol 27:510–517. https://doi.org/10.1016/j.jmig.2019.04.017
Ali ZS, Flanders TM, Ozturk AK et al (2019) Enhanced recovery after elective spinal and peripheral nerve surgery: pilot study from a single institution. J Neurosurg Spine 30:532–540. https://doi.org/10.3171/2018.9.SPINE18681
Brusko GD, Kolcun JPG, Heger JA et al (2019) Reductions in length of stay, narcotics use, and pain following implementation of an enhanced recovery after surgery program for 1- to 3-level lumbar fusion surgery. Neurosurg Focus. https://doi.org/10.3171/2019.1.FOCUS18692
Jazini E, Thomson AE, Sabet AD et al (2021) Adoption of enhanced surgical recovery (ESR) protocol for lumbar fusion decreases in-hospital postoperative opioid consumption. Glob Spine J. https://doi.org/10.1177/21925682211015652
Adeyemo EA, Aoun SG, Barrie U et al (2021) Enhanced recovery after surgery reduces postoperative opioid use and 90-day readmission rates after open thoracolumbar fusion for adult degenerative deformity. Neurosurgery 88:295–300. https://doi.org/10.1093/neuros/nyaa399
Bradywood A, Farrokhi F, Williams B et al (2017) Reduction of inpatient hospital length of stay in lumbar fusion patients with implementation of an evidence-based clinical care pathway. Spine (Phila Pa 1976) 42:169–176. https://doi.org/10.1097/BRS.0000000000001703
Talec P, Gaujoux S, Samama CM (2016) Early ambulation and prevention of post-operative thrombo-embolic risk. J Visc Surg 153:S11–S14. https://doi.org/10.1016/j.jviscsurg.2016.09.002
Zakaria HM, Bazydlo M, Schultz L et al (2020) Ambulation on postoperative day #0 is associated with decreased morbidity and adverse events after elective lumbar spine surgery: analysis from the Michigan Spine Surgery Improvement Collaborative (MSSIC). Neurosurgery 87:320–328. https://doi.org/10.1093/neuros/nyz501
Adogwa O, Elsamadicy AA, Fialkoff J et al (2017) Early ambulation decreases length of hospital stay, perioperative complications and improves functional outcomes in elderly patients undergoing surgery for correction of adult degenerative scoliosis. Spine (Phila Pa 1976) 42:1420–1425. https://doi.org/10.1097/BRS.0000000000002189
Dietz N, Sharma M, Adams S et al (2019) Enhanced recovery after surgery (ERAS) for spine surgery: a systematic review. World Neurosurg 130:415–426. https://doi.org/10.1016/j.wneu.2019.06.181
Gornitzky AL, Flynn JM, Muhly WT et al (2016) A Rapid recovery pathway for adolescent idiopathic scoliosis that improves pain control and reduces time to inpatient recovery after posterior spinal fusion. Spine Deform 4:288–295. https://doi.org/10.1016/j.jspd.2016.01.001
Rao RR, Hayes M, Lewis C et al (2017) Mapping the road to recovery: shorter stays and satisfied patients in posterior spinal fusion. J Pediatr Orthop 37:e536–e542. https://doi.org/10.1097/BPO.0000000000000773
Fletcher ND, Andras LM, Lazarus DE et al (2017) Use of a novel pathway for early discharge was associated with a 48% shorter length of stay after posterior spinal fusion for adolescent idiopathic scoliosis. J Pediatr Orthop 37:92–97. https://doi.org/10.1097/BPO.0000000000000601
Debono B, Wainwright TW, Wang MY et al (2021) Consensus statement for perioperative care in lumbar spinal fusion: enhanced recovery after surgery (ERAS®) society recommendations. Spine J 21:729–752. https://doi.org/10.1016/j.spinee.2021.01.001
Funding
No outside funds were received for this study.
Author information
Authors and Affiliations
Contributions
EJ, AET, ADS, OS, LYC, LO, FRB, RR, CMH, TCS, CRG: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; EJ, AET, ADS, OS, LYC, LO, FRB, RR, CMH, TCS, CRG: drafted the work or revised it critically for important intellectual content; EJ, AET, ADS, OS, LYC, LO, FRB, RR, CMH, TCS, CRG: approved the version to be published; and EJ, AET, ADS, OS, LYC, LO, FRB, RR, CMH, TCS, CRG: agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflicts of interest/Competing interests
CRG has received consulting fees from K2M, Stryker, Medtronic, Mazor and is on an advisory board for Stryker, Augmedics, Medtronic, has received royalties from K2M and has stock in Augmedics and NSite. LYC is an employee of Norton Healthcare and the University of Southern Denmark; received consulting fees from the National Spine Health Foundation; member, Editorial Advisory Board, Spine Deformity, The Spine Journal and Spine; member University of Louisville IRB; institution received research funds from OREF, NIH, ISSG, SRS, TSRH, Pfizer, Lifesciences Corporation, IntelliRod, Cerapedics, Medtronic, Empirical Spine and NeuroPoint Alliance. EJ has received consulting fees from Medtronic, Stryker, and Precision Spine. CMH has received consulting fees from Medtronic, Globus Medical, and Spineart. The authors have no other conflicts of interest to declare.
Ethics approval
Quorum Review serves as a central IRB and approved the study protocol (File #: 33866/1) on February 3rd, 2019. Migration of IRB from Quorum to Advarra occurred September 4th, 2019, with the study approval for ERAS-001 (Pro00036529). This study was conducted in accordance with the 1964 Helsinki Declaration, its amendments, and other equivalent ethical standards.
Consent to participate
All study participants or their legally authorized representative signed written informed consent for study participation prior to surgery, included in the Notice of Privacy Practices.
Consent for publication
All study participants or their legally authorized representative signed written informed consent for publication prior to surgery, included in the Notice of Privacy Practices.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jazini, E., Thomson, A.E., Sabet, A.D. et al. Adoption of enhanced surgical recovery (ESR) protocol for adult spinal deformity (ASD) surgery decreases in-hospital and 90-day post-operative opioid consumption. Spine Deform 10, 443–448 (2022). https://doi.org/10.1007/s43390-021-00437-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00437-w