Abstract
Purpose
Intraoperative neuromonitoring (IONM) has historically been difficult to obtain in patients with Charcot–Marie–Tooth (CMT) disease. Transcranial motor-evoked potentials (TcMEPs) have been found to be safe and effective for other spinal deformity patients. Our objective was to determine the effectiveness of TcMEP monitoring in patients with CMT.
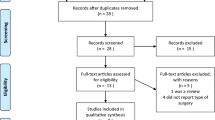
Methods
An IRB-approved, retrospective review of CMT patients undergoing spinal deformity surgery assessing TcMEP, somatosensory-evoked potential (SSEP), and neurogenic motor evoked potential (NMEP) IONM was performed. A 2:1 matched cohort control group of idiopathic spinal deformity patients was used. A waveform grading system was applied to review baseline TcMEP reliability and quality, which was validated via intraclass correlation coefficient amongst five raters.
Results
Twenty-three CMT patients (26 surgical cases) were identified. The use of TcMEP improved the ability to obtain baseline IONM when compared to SSEP (83% vs. 20%; p < 0.001) and NMEP (83% vs. 18%; p = 0.003). Baseline monitoring was obtained less often for CMT patients using SSEP (20% vs. 100%; p < 0.001) and TcMEP (83% vs. 100%; p = 0.111) compared to idiopathic patients. Sweep length (time from stimulation waveform evaluation) and maximum stimulation voltage were higher in the CMT group (289 ms vs. 111 ms p = 0.007 and 740 V vs. 345 V p = 0.089, respectively).
Conclusion
TcMEP monitoring significantly improves the ability to provide IONM for CMT patients undergoing spinal deformity surgery. Utilizing longer sweep lengths enhances the ability to attain baseline TcMEP readings, allowing surgeons to more safely proceed with surgery for these complex patients.
Level of evidence
Therapeutic-Level III.




Similar content being viewed by others
References
Harding AE, Thomas PK (1980) Genetic aspects of hereditary motor and sensory neuropathy (types I and II). J Med Genet 17(5):329–336
Skre H (1974) Genetic and clinical aspects of Charcot-Marie-Tooth’s disease. Clin Genet 6(2):98–118
Karol LA, Elerson E (2007) Scoliosis in patients with Charcot-Marie-Tooth disease. J Bone Jt Surg Am 89(7):1504–1510. https://doi.org/10.2106/jbjs.F.01161
Hensinger RN, MacEwen GD (1976) Spinal deformity associated with heritable neurological conditions: spinal muscular atrophy, Friedreich’s ataxia, familial dysautonomia, and Charcot-Marie-Tooth disease. J Bone Jt Surg Am 58(1):13–24
Walker JL, Nelson KR, Stevens DB et al (1994) Spinal deformity in Charcot-Marie-Tooth disease. Spine 19(9):1044–1047
Horacek O, Mazanec R, Morris CE et al (2007) Spinal deformities in hereditary motor and sensory neuropathy: a retrospective qualitative, quantitative, genotypical, and familial analysis of 175 patients. Spine 32(22):2502–2508. https://doi.org/10.1097/BRS.0b013e3181573d4e
Pastorelli F, Di Silvestre M, Plasmati R et al (2011) The prevention of neural complications in the surgical treatment of scoliosis: the role of the neurophysiological intraoperative monitoring. Eur Spine J 20(Suppl 1):S105-114. https://doi.org/10.1007/s00586-011-1756-z
Nuwer MR, Emerson RG, Galloway G et al (2012) Evidence-based guideline update: intraoperative spinal monitoring with somatosensory and transcranial electrical motor evoked potentials: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Clinical Neurophysiology Society. Neurology 78(8):585–589. https://doi.org/10.1212/WNL.0b013e318247fa0e
Fehlings MG, Brodke DS, Norvell DC et al (2010) The evidence for intraoperative neurophysiological monitoring in spine surgery: does it make a difference? Spine 35(9 Suppl):S37-46. https://doi.org/10.1097/BRS.0b013e3181d8338e
Langeloo DD, Lelivelt A, Louis Journee H et al (2003) Transcranial electrical motor-evoked potential monitoring during surgery for spinal deformity: a study of 145 patients. Spine 28(10):1043–1050. https://doi.org/10.1097/01.Brs.0000061995.75709.78
Schwartz DM, Auerbach JD, Dormans JP et al (2007) Neurophysiological detection of impending spinal cord injury during scoliosis surgery. J Bone Jt Surg Am 89(11):2440–2449. https://doi.org/10.2106/jbjs.F.01476
MacDonald DB, Al Zayed Z, Khoudeir I et al (2003) Monitoring scoliosis surgery with combined multiple pulse transcranial electric motor and cortical somatosensory-evoked potentials from the lower and upper extremities. Spine 28(2):194–203. https://doi.org/10.1097/01.Brs.0000041583.59280.24
Schmidt R, Mani P, Weber D (2015) Case studies of transcranial electrical motor evoked potentials (TCeMEP) on patients with Charcot-Marie-Tooth disease during posterior spinal instrumentation and fusion. Neurodiagn J 55(2):97–106
El-Hawary R, Sucato DJ, Sparagana S et al (2006) Spinal cord monitoring in patients with spinal deformity and neural axis abnormalities: a comparison with adolescent idiopathic scoliosis patients. Spine 31(19):E698-706. https://doi.org/10.1097/01.brs.0000232707.98076.37
Calancie B (2017) Intraoperative neuromonitoring and alarm criteria for judging MEP responses to transcranial electric stimulation: the threshold-level method. J Clin Neurophysiol 34(1):12–21. https://doi.org/10.1097/wnp.0000000000000339
Jones SJ, Harrison R, Koh KF et al (1996) Motor evoked potential monitoring during spinal surgery: responses of distal limb muscles to transcranial cortical stimulation with pulse trains. Electroencephalogr Clin Neurophysiol 100(5):375–383
Thomas PK, Calne DB, Stewart G (1974) Hereditary motor and sensory polyneuropathy (peroneal muscular atrophy). Ann Hum Genet 38(2):111–153. https://doi.org/10.1111/j.1469-1809.1974.tb01945.x
Krishna M, Taylor JF, Brown MC et al (1991) Failure of somatosensory-evoked-potential monitoring in sensorimotor neuropathy. Spine 16(4):479. https://doi.org/10.1097/00007632-199104000-00018
Muchow RD, McClung A, Rampy P et al (2013) Spinal cord monitoring with transcranial motor evoked potentials in patients with neural axis abnormalities undergoing spinal deformity surgery. Spine Deform 1(3):205–210. https://doi.org/10.1016/j.jspd.2013.02.002
Dyck PJ, Lambert EH (1968) Lower motor and primary sensory neuron diseases with peroneal muscular atrophy. I. Neurologic, genetic, and electrophysiologic findings in hereditary polyneuropathies. Arch Neurol 18(6):603–618
Dyck PJ, Lambert EH (1968) Lower motor and primary sensory neuron diseases with peroneal muscular atrophy. II. Neurologic, genetic, and electrophysiologic findings in various neuronal degenerations. Arch Neurol 18(6):619–625
Funding
This work was supported by the Texas Scottish Rite Hospital for Children.
Author information
Authors and Affiliations
Contributions
JP: concept, study design, acquisition, analysis, interpretation of data, drafting of manuscript, critical revision of manuscript, final approval of manuscript; KP: concept, study design, acquisition, analysis, critical revision of manuscript, final approval of manuscript; SS: acquisition, analysis, interpretation of data, critical revision of manuscript, final approval of manuscript; PR: acquisition, analysis, interpretation of data, critical revision of manuscript, final approval of manuscript; SF: acquisition, analysis, interpretation of data, critical revision of manuscript, final approval of manuscript; C-HJ: study design, acquisition, analysis, interpretation of data, critical revision of manuscript, final approval of manuscript; DS: concept, study design, acquisition, analysis, interpretation of data, critical revision of manuscript, final approval of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Kiley Poppino, Steven Sparagana, Patricia Rampy, Spender Freeman, Chan-Hee Jo, and Daniel Sucato declare they have no conflicts of interest. Jeffrey B. Peck declares a relationship with Smith and Nephew, which consisted of Smith and Nephew providing funds to the Hospital for Special Surgery (HSS) for the purpose of advancing the hospital’s research endeavors during his fellowship there.
Ethics approval
The study was approved by the Texas Scottish Rite Hospital Institutional Review Board and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This investigation was IRB-approved.
Consent to participate
This was a retrospective chart review. A waiver of consent was applied to all study participants.
Consent for publication
A waiver of consent was applied for all study participants.
Available of data and material
The data pertaining to this study is available and accessible for review as allowed by the guidelines of our Institutional Review Board and other research regulatory entities.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peck, J., Poppino, K., Sparagana, S. et al. Use of transcranial motor-evoked potentials to provide reliable intraoperative neuromonitoring for the Charcot–Marie–Tooth population undergoing spine deformity surgery. Spine Deform 10, 411–418 (2022). https://doi.org/10.1007/s43390-021-00409-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00409-0