Abstract
Purpose
Spinal muscles are a major component of posture in spinal pathologies and changes to the spine with aging. Specifically, spinopelvic muscles may compensate for underlying anomalies such as pelvic retroversion, knee flexion, and cervical or thoracic spinal balance abnormalities. To increase understanding between muscular characteristics and compensatory mechanisms, this study aimed to compare the volume of spinopelvic muscles in adults with a spinal deformity (ASD) to a control group of well-aligned adult subjects.
Methods
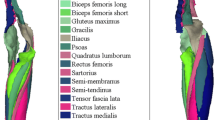
Twenty-eight lumbar ASD patients [Cobb angle > 20°, > 40 years old (yo)] were prospectively included and compared to 35 normal subjects divided into 2 different groups: one group of young (Y) subjects (n = 23, < 20 yo) and one group of old (O) subjects (n = 12, > 40 yo). All subjects had a fat/water separation MRI (from C7 to the knees). Volumetric 3D reconstructions of 30 spinopelvic muscles were performed and muscles volumes were compared.
Results
Mean age was 60 ± 16 yo, without significant differences between the ASD and O groups (57 ± 11 yo). Age and BMI were smaller in the young group. Mean Cobb angle of the ASD group was 45 ± 11°. Comparing the ASD and O groups, total muscular volume was similar; however, erector spinae (0.24 ± 0.06 vs 0.68 ± 0.08 dm3, p = 0.001), iliopsoas (0.49 ± 0.09 vs 0.60 ± 0.09 dm3, p = 0.001) and obliquus (0.42 ± 0.08 vs 0.50 ± 0.08 dm3, p = 0.02) were significantly smaller in the ASD group. Comparing the Y and the ASD groups, total muscular volume was higher in the Y group than the ASD group (+ 3.3 dm3, p = 0.003) and erector spinae (0.24 ± 0.06 vs 0.74 ± 0.08, p = 0.0001), gluteus medius (0.51 ± 0.07 vs 0.62 ± 0.13, p = 0.01) and vastus lateralis (1.33 ± 0.21 vs 2.08 ± 0.29, p = 0.001) were significantly bigger in the Y group.
Conclusion
This is the first study to compare volume of spinopelvic muscles between ASD patients and a control group without spinal deformity. Our results demonstrate that muscular degeneration has a double origin: aging and deformity. Erector spinae, iliopsoas, and obliquus are the muscles most affected by degeneration.




Similar content being viewed by others
References
Kebaish KM, Neubauer PR, Voros GD, Khoshnevisan MA, Skolasky RL (2011) Scoliosis in adults aged forty years and older: prevalence and relationship to age, race, and gender. Spine 36(9):731–736
Yadla S, Maltenfort MG, Ratliff JK, Harrop JS (2010) Adult scoliosis surgery outcomes: a systematic review. Neurosurg Focus 28(3):E3
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC et al (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303(13):1259–1265
Benoist M (2003) Natural history of the aging spine. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 12(Suppl 2):S86-89
Trammell TR, Schroeder RD, Reed DB (1988) Rotatory olisthesis in idiopathic scoliosis. Spine 13(12):1378–1382
Schwab F, Farcy J-P, Bridwell K, Berven S, Glassman S et al (2006) A clinical impact classification of scoliosis in the adult. Spine 31(18):2109–2114
Lafage V, Schwab F, Patel A, Hawkinson N, Farcy J-P (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 34(17):E599-606
Ferrero E, Liabaud B, Challier V, Lafage R, Diebo BG et al (2016) Role of pelvic translation and lower-extremity compensation to maintain gravity line position in spinal deformity. J Neurosurg Spine 24(3):436–446
Diebo BG, Ferrero E, Lafage R, Challier V, Liabaud B et al (2015) Recruitment of compensatory mechanisms in sagittal spinal malalignment is age and regional deformity dependent: a full-standing axis analysis of key radiographical parameters. Spine 40(9):642–649
Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V (2015) Sagittal alignment of the spine: what do you need to know? Clin Neurol Neurosurg 139(295):301
Meakin JR, Fulford J, Seymour R, Welsman JR, Knapp KM (2013) The relationship between sagittal curvature and extensor muscle volume in the lumbar spine. J Anat 222(6):608–614
Ferrero E, Skalli W, Lafage V, Maillot C, Carlier R et al (2019) Relationships between radiographic parameters and spinopelvic muscles in adult spinal deformity patients. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. https://doi.org/10.1007/s00586-019-06243-3
Kang CH, Shin MJ, Kim SM, Lee SH, Lee C-S (2007) MRI of paraspinal muscles in lumbar degenerative kyphosis patients and control patients with chronic low back pain. Clin Radiol 62(5):479–486
Teichtahl AJ, Urquhart DM, Wang Y, Wluka AE, Wijethilake P et al (2015) Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J Off J North Am Spine Soc 15(7):1593–1601
Amabile C, Moal B, Chtara OA, Pillet H, Raya JG et al (2017) Estimation of spinopelvic muscles’ volumes in young asymptomatic subjects: a quantitative analysis. Surg Radiol Anat SRA 39(4):393–403
Zhang C, Moal B, Dubois G, Raya J, Lafage V, Skalli W (2014) Comparison of two MRI sequences for subject-specific 3D thigh muscle reconstruction. Comput Methods Biomech Biomed Engin 17(Suppl 1):136–137
Moal B, Bronsard N, Raya JG, Vital J-M, Schwab F et al (2015) Volume and fat infiltration of spino-pelvic musculature in adults with spinal deformity. World J Orthop 6(9):727–737
Moal B, Schwab F, Ames CP, Smith JS, Ryan D et al (2014) Radiographic outcomes of adult spinal deformity correction: a critical analysis of variability and failures across deformity patterns. Spine Deform 2(3):219–225
Dixon WT (1984) Simple proton spectroscopic imaging. Radiology 153(1):189–194
Ragan DK, Bankson JA (2010) Two-point dixon technique provides robust fat suppression for multi-mouse imaging. J Magn Reson Imaging JMRI 31(2):510–514
Hausselle J, Assi A, El Helou A, Jolivet E, Pillet H et al (2014) Subject-specific musculoskeletal model of the lower limb in a lying and standing position. Comput Methods Biomech Biomed Engin 17(5):480–487
Hyun S-J, Kim YJ, Rhim S-C (2016) Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J Off J North Am Spine Soc 16(9):1095–1101
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
EF: Conception, data acquisition, formal analysis, and writing (draft-editing). WS: Conception, software, and revision. MK: Data acquisition, methodology, and revision. RC, AF, AF: Data acquisition and revision. PG: Conception, supervision, and revision. VL: Conception, software, and revision. All the authors approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
EF, MK, RC, AF, AF, and PG none. WS with Euros. VL with Globus, Nuvasive, Implanet, and Depuy Synthes.
Ethical approval
Approved by local ethic committee.
Rights and permissions
About this article
Cite this article
Ferrero, E., Skalli, W., Khalifé, M. et al. Volume of spinopelvic muscles: comparison between adult spinal deformity patients and asymptomatic subjects. Spine Deform 9, 1617–1624 (2021). https://doi.org/10.1007/s43390-021-00357-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00357-9