Abstract
Purpose
To describe the clinical and radiographic profile of early-onset scoliosis (EOS) patients treated with traditional growing rods (TGR) during the magnetically-controlled growing rod (MCGR) era.
Methods
A US multicenter EOS database was reviewed to identify (1) patients who underwent TGR after MCGR surgery was introduced at their institution, (2) patients who underwent MCGR during the same time period. Of 19 centers, 8 met criteria with all EOS etiologies represented. Clinical notes were reviewed to determine the indication for TGR. Patient demographics and pre-operative radiographs were compared between groups.
Results
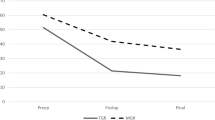
A total of 25 TGR and 127 MCGR patients were identified. The TGR patients were grouped by indication into the sagittal plane profile (n = 11), trunk height (n = 6), co-morbidities/need for MRI (n = 4), and other (ex: behavioral issues, remaining growth). Four patients had a combination of sagittal profile and short stature with sagittal profile listed as primary factor. The TGR short trunk group had a mean T1–S1 length of 192 mm vs 273 mm for the MCGR group (p = 0.0002). The TGR sagittal profile group, had a mean maximal kyphosis of 61° vs 55° for the MCGR group (p = 0.09).
Conclusion
TGR continues to have a role in the MCGR era. In this study, the most commonly reported indications for TGR were sagittal plane profile and trunk height. These results suggest that TGR is indicated in patients of short stature with stiff hyperkyphotic curves. As further experience is gained with MCGR, the indications for TGR will likely be refined.




Similar content being viewed by others
References
Skaggs DL, Akbarnia BA, Flynn JM et al (2014) A classification of growth friendly spine implants. J Pediatr Orthop 34(3):260–274
Cheung KM, Cheung JP, Samartzis D et al (2012) Magnetically controlled growing rods for severe spinal curvature in young children: a prospective case series. Lancet 379(9830):1967–1974
Hosseini P, Pawelek J, Mundis GM et al (2016) Magnetically controlled growing rods for early-onset scoliosis: a multicenter study of 23 cases with minimum 2 years follow-up. Spine 41(18):1456–1462
Schroerlucke SR, Akbarnia BA, Pawelek JB et al (2012) How does thoracic kyphosis affect patient outcomes in growing rod surgery? Spine 37(15):1303–1309
Upasani VV, Parvaresh KC, Pawelek JB et al (2016) Age at initiation and deformity magnitude influence complication rates of surgical treatment with traditional growing rods in early-onset scoliosis. Spine Deform 4(5):344–350
Cheung JP, Cahill P, Yaszay B, Akbarnia BA, Cheung KM (2015) Special article: update on the magnetically controlled growing rod: tips and pitfalls. J Orthop Surg (Hong Kong) 23(3):383–390
Tan KA, Sewell MD, Clarke AJ et al (2017) Recommendations for lengthening of magnetically controlled growing rods in children with pacemakers. J Pediatr Orthop 37(4):e250–e254
Hasler CC (2018) Early-onset scoliosis: contemporary decision-making and treatment options. J Pediatr Orthop 38(Suppl 1):S13–S20
Sanders JO, D’Astous J, Fitzgerald M, Khoury JG, Kishan S, Sturm PF (2009) Derotational casting for progressive infantile scoliosis. J Pediatr Orthop 29(6):581–587
Gussous YM, Tarima S, Zhao S et al (2015) Serial derotational casting in idiopathic and non-idiopathic progressive early-onset scoliosis. Spine Deform 3(3):233–238
Baulesh DM, Huh J, Judkins T, Garg S, Miller NH, Erickson MA (2012) The role of serial casting in early-onset scoliosis (EOS). J Pediatr Orthop 32(7):658–663
Newton PO, Kluck DG, Saito W, Yaszay B, Bartley CE, Bastrom TP (2018) Anterior spinal growth tethering for skeletally immature patients with scoliosis: a retrospective look two to four years postoperatively. J Bone Jt Surg Am 100(19):1691–1697
Luhmann SJ, Smith JC, McClung A et al (2017) Radiographic outcomes of shilla growth guidance system and traditional growing rods through definitive treatment. Spine Deform 5(4):277–282
Akbarnia BA, Pawelek JB, Cheung KM et al (2014) Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosis: a case-matched 2-year study. Spine Deform 2(6):493–497
Pawelek JB, Yaszay B, Nguyen S et al (2016) Case-matched comparison of spinal fusion versus growing rods for progressive idiopathic scoliosis in skeletally immature patients. Spine 41(3):234–238
Vitale MG, Gomez JA, Matsumoto H, Roye DP Jr, Chest W, Spine Deformity Study G (2011) Variability of expert opinion in treatment of early-onset scoliosis. Clin Orthop Relat Res. 469(5):1317–1322
Akbarnia BA, Marks DS, Boachie-Adjei O, Thompson AG, Asher MA (2005) Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine 30(17 Suppl):S46-57
La Rosa G, Oggiano L, Ruzzini L (2017) Magnetically controlled growing rods for the management of early-onset scoliosis: a preliminary report. J Pediatr Orthop 37(2):79–85
Doany ME, Olgun ZD, Kinikli GI et al (2018) Health-related quality of life in early-onset scoliosis patients treated surgically: EOSQ scores in traditional growing rod versus magnetically controlled growing rods. Spine 43(2):148–153
Bekmez S, Afandiyev A, Dede O, Karaismailoglu E, Demirkiran HG, Yazici M (2019) Is magnetically controlled growing rod the game changer in early-onset scoliosis? A preliminary report. J Pediatr Orthop 39(3):e195–e200
Bauer JM, Yorgova P, Neiss G et al (2018) Early onset scoliosis: is there an improvement in quality of life with conversion from traditional growing rods to magnetically controlled growing rods? J Pediatr Orthop. 39:e284–e288
Hardesty CK, Huang RP, El-Hawary R et al (2018) Early-onset scoliosis: updated treatment techniques and results. Spine Deform 6(4):467–472
Teoh KH, Winson DM, James SH et al (2016) Do magnetic growing rods have lower complication rates compared with conventional growing rods? Spine J 16(4 Suppl):S40-44
Thakar C, Kieser DC, Mardare M, Haleem S, Fairbank J, Nnadi C (2018) Systematic review of the complications associated with magnetically controlled growing rods for the treatment of early onset scoliosis. Eur Spine J 27(9):2062–2071
Choi E, Yaszay B, Mundis G et al (2017) Implant complications after magnetically controlled growing rods for early onset scoliosis: a multicenter retrospective review. J Pediatr Orthop 37(8):e588–e592
Watanabe K, Uno K, Suzuki T et al (2016) Risk factors for proximal junctional kyphosis associated with dual-rod growing-rod surgery for early-onset scoliosis. Clin Spine Surg 29(8):E428-433
Chen Z, Qiu Y, Zhu Z, Li S, Chen X, Sun X (2017) How does hyperkyphotic early-onset scoliosis respond to growing rod treatment? J Pediatr Orthop 37(8):e593–e598
Noordeen HM, Shah SA, Elsebaie HB, Garrido E, Farooq N, Al-Mukhtar M (2011) In vivo distraction force and length measurements of growing rods: which factors influence the ability to lengthen? Spine 36(26):2299–2303
Sankar WN, Skaggs DL, Yazici M et al (2011) Lengthening of dual growing rods and the law of diminishing returns. Spine 36(10):806–809
Poon S, Chen YH, Wendolowski SF et al (2018) Cadaveric study of the safety and device functionality of magnetically controlled growing rods after exposure to magnetic resonance imaging. Spine Deform 6(3):290–298
Poon S, Nixon R, Wendolowski S et al (2017) A pilot cadaveric study of temperature and adjacent tissue changes after exposure of magnetic-controlled growing rods to MRI. Eur Spine J 26(6):1618–1623
Acknowledgements
Pediatric Spine Study Group (Abdullah Saad Abdulfattah Abdullah MBChB, MRCS, Behrooz Akbarnia MD, Jason Anari MD, John Anderson MD, Richard Anderson MD, Lindsay Andras MD, Laura Bellaire MD, Randy Betz MD, Craig Birch MD, Laurel Blakemore MD, Oheneba Boachie-Adjei MD, Chris Bonfield MD, Douglas Brockmeyer MD, Jaysson Brooks MD, Pat Cahill MD, Jason Cheung MD, Kenneth Cheung MD, FRCS, FHKCOS, FHKAM, Haemish Crawford MD, Alvin Crawford MD, FACS, Gokhan Demirkiran PhD, Hazem El Sebaie MD, FRCS, Ron El-Hawary MD, MSc, FRCS(c), John Emans MD, Mark Erickson MD, Frances Farley MD, Graham Fedorak MD, Ryan Fitzgerald MD, Nicholas Fletcher MD, Lorena Floccari MD, Jack Flynn MD, Peter Gabos MD, Adrian Gardner MD, Sumeet Garg MD, Michael Glotzbecker MD, Jaime Gomez MD, Tenner Guillaume MD, Purnendu Gupta MD, Kyle Halvorson MD, Kim Hammerberg MD, Christina Hardesty MD, Daniel Hedequist MD, Michael Heffernan MD, John Heflin MD, Ilkka Helenius MD, PhD, Grant Hogue MD, Josh Holt MD, Jason Howard MD, Michael Timothy Hresko MD, Steven Hwang MD, Stephanie Ihnow MD, Brice Ilharreborde MD, PhD, Kenneth Illingworth MD, Andrew Jea MD, Charles Johnston MD, Judson Karlen MD, Lawrence Karlin MD, Noriaki Kawakami MD, Brian Kelly MD, Kenny Kwan BMBCh, FRCSEd, FHKCOS, FHKAM, Robert Lark MD, A. Noelle Larson MD, William Lavelle MD, Sean Lew MD, Gertrude Li MD, Scott Luhmann MD, Stuart Mackenzie MD, Sanchez Marquez MD, Jonathan Martin MD, Jeffrey Martus MD, MS, Oscar Mayer MD, Amy McIntosh MD, Jwalant Mehta MD, Daniel Miller MD, Firoz Miyanji MD, Greg Mundis MD, Josh Murphy MD, Robert Murphy MD, Susan Nelson MD, MPH, Peter Newton MD, Matthew Oetgen MD, MBA, Josh Pahys MD, Stefan Parent MD, PhD, Javier Pizones MD, PhD, Selina Poon MD, Nigel Price MD, Norman Ramirez-Lluch MD, Brandon Ramo MD, Gregory Redding MD, Luis Rodriguez MD, David Roye MD, Benjamin Roye MD, Lisa Saiman MD, PhD, Amer Samdani MD, Francisco Sanchez Perez-Grueso MD, James Sanders MD, Jeffrey Sawyer MD, Jacob Schulz MD, Richard Schwend MD, Suken Shah MD, David Skaggs MD, MMM, Kevin Smit MD, FRCSC, John Smith MD, Brian Snyder MD, PhD, Paul Sponseller MD, Peter Sturm MD, Michal Szczodry MD, John Thometz MD, George Thompson MD, Walter Truong MD, Raphael Vialle MD, Michael Vitale MD, MPH, John Vorhies MD, Stuart Weinstein MD, Michelle Welborn MD, Klane White MD, Burt Yaszay MD, Muharrem Yazici MD) are affiliated with Children’s Spine Foundation, Valley Forge, PA, USA.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Consortia
Contributions
ESV, JBP, GMMJr, MEO, PFS, BAA, PSSG, BY design, data acquisition, analysis and/or interpretation of work, manuscript drafting and/or critically revising, manuscript drafting and/or critically revising, final approval.
Corresponding author
Ethics declarations
Ethical approval
IRB approval was obtained for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Varley, E.S., Pawelek, J.B., Mundis Jr., G.M. et al. The role of traditional growing rods in the era of magnetically controlled growing rods for the treatment of early-onset scoliosis. Spine Deform 9, 1465–1472 (2021). https://doi.org/10.1007/s43390-021-00332-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00332-4