Abstract
Purpose
The purpose of this study was to determine peri-operative morbidity associated with anterior vertebral body tethering (aVBT) for idiopathic scoliosis.
Method
Of 175 patients treated with aVBT, 120 patients had 2 year follow up and were included in this study. Prospectively collected clinical and radiographic data was analyzed retrospectively.
Results
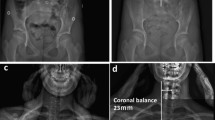
Pre-operatively, the mean patient age was 12.6 year (8.2–15.7 year), Risser 0–3, with main thoracic scoliosis 51.2° (40–70°). Immediately post-operative, scoliosis improved to 26.9° (6–53°; p < 0.05), at 1-year post-operative was 23.0° (− 11 to 50°; p < 0.01 vs immediate post-op) and at 2-year post-operative was 27.5° (− 5 to 52; p = 0.64 vs immediate post-op). Pre-operative T5–T12 kyphosis was 16.0° (− 23 to 52°), post-operative was 16.9° (− 7 to 44°), at 1-year was 17.5° (− 14 to 61°) and at 2-year was 17.0° (− 10 to 50°; p = 0.72 vs pre-op). All patients underwent thoracoscopic approach, EBL 200 ml (20–900 ml), surgical time 215.3 min (111–472 min), anesthesia time 303.5 min (207–480 min), ICU stay of 0.2 day (0–2 days), and post-operative hospital stay 4.5 days (2–9 days). During the in-hospital peri-operative period, there were no unplanned return to the operating room (UPROR) and there was a 0.8% rate of complication: one pneumothorax requiring reinsertion of chest tube. By 90 days post-operative, there was no UPROR and a 5% rate of complication. Five additional patients developed complications after discharge: one CSF leak treated with blood patch injection in the clinic and resolved, two pleural effusions requiring chest tubes, one superficial wound infection and one pneumonia treated with outpatient antibiotics. By 1-year post-op, there was a 1.7% rate of UPROR and 8.3% rate of complication. Four additional patients developed complications beyond 90 days: two upper limb paresthesia required outpatient medical management, one CSF leak which initially treated blood patch injection in the clinic initially which then required UPROR, and one compensatory lumbar curve add on that was treated with extension of the tether. By 2-years post-op, there was a 6.7% rate of UPROR and 15.8% rate of complication. 9 additional complications developed after 1 year. One curve progression, one keloid scar, one right leg weakness, 4 cable failures and 2 curve overcorrections.
Conclusion
This large, multicenter series of aVBT demonstrated a 15.8% complication rate and a 6.7% UPROR rate at 2 year post-operatively. This early study during the learning curve of aVBT found higher rates of CSF leaks and overall complications than would be expected for PSFI at 1 year post-operatively and a higher rate of overall complications and of UPROR than would be expected for PSFI at 2 year post-operatively. As is common with new procedures, the complication rate may fall with further experience.



Similar content being viewed by others
Data availability
Registry data is available to member institutions. Measurements and analysis done at the IWK Health Centre are on a password protected server. Access may be arranged through application to the REB.
Code availability
Statistical analysis was conducted using SPSS v20 (IBM Corporation, Armonk, NY, USA).
References
Grivas TB, Burwell GR, Vasiliadis ES, Webb JK (2006) A segmental radiological study of the spine and rib-cage in children with progressive Infantile Idiopathic Scoliosis. Scoliosis 1:17 (PMC free article) (PubMed) (Google Scholar)
Deacon P, Flood BM, Dickson RA (1984) Idiopathic scoliosis in three dimensions. A radiographic and morphometric analysis. J Bone Jt Surg 66(4):509–512 (Citation Time(s):2)
Cobb JR (1948) Outline for the study of scoliosis. In: Ann Arbor JW Edwards (ed) Instructional course lectures, The American Academy of Orthopaedic Surgeons, vol 5, pp 261–275
Morrissy RT, Weinstein SL (2006) Idiopathic scoliosis in Lovell & Winter’s pediatric orthopedics. Lippincott Williams & Wilkins, Philadelphia, pp 694–762
Horton D (2002) Common skeletal deformities. In: Rimoin DL, Conner MJ, Pyeritz RE, Korf BR (eds) Emery & Rimoins principles and practices of medical genetics. Churchill Livingstone Elsevier, Amsterdam, pp 4236–4244
Bunnell WP (1988) The natural history of idiopathic scoliosis. Clin Orthop Relat Res 229:20–25
Kuroki H (2018) Brace treatment for adolescent idiopathic scoliosis. J Clin Med. 7(6):136. https://doi.org/10.3390/jcm7060136(Published online 2018 Jun 4)
Janicki JA, Poe-Kochert C, Armstrong DG, Thompson GH (2007) A comparison of the thoracolumbosacral orthoses and Providence orthosis in the treatment of adolescent idiopathic scoliosis: results using the new SRS inclusion and assessment criteria for bracing studies. J Pediatr Orthop 27:369–374. https://doi.org/10.1097/01.bpb.0000271331.71857.9a.[PubMed][CrossRef][GoogleScholar]
Kepler CK, Meredith DS, Green DW, Widmann RF (2012) Longterm outcomes after posterior spine fusion for adolescent idiopathic scoliosis. Curr Opin Pediatr 24(1):68–75
Green DW, Lawhorne TW, Widmann RF, Kepler CK, Ahern C, Mintz DN, Rawlins BA, Burke SW, Boachie-Adjei O (2011) Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine (Phila Pa, 1976) 36(23):1948–1954
Samdani AF, Ames RJ, Kimball JS et al (2015) Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J 24:1533–1539 (PubMed) (Google Scholar)
Newton PO, Kluck DG, Saito W et al (2018) Anterior spinal growth tethering for skeletally immature patients with scoliosis: a retrospective look two to four years postoperatively. J Bone Jt Surg Am 100(19):1691–1697. https://doi.org/10.2106/JBJS.18.00287
Anari JB, Flynn JM, Cahill PJ et al (2020) Unplanned return to OR (UPROR) for children with early onset scoliosis (EOS): a comprehensive evaluation of all diagnoses and instrumentation strategies. Spine Deform 8(2):295–302. https://doi.org/10.1007/s43390-019-00024-0(Epub 2020 Feb 6)
Smith JT, Johnston C, Skaggs D, Flynn J, Vitale M (2015) A new classification system to report complications in growing spine surgery: a multicenter consensus study. J PediatrOrthop 35(8):798–803. https://doi.org/10.1097/BPO.0000000000000386
Dodwell ER, Pathy R, Widmann RF et al (2018) Reliability of the modified Clavien–Dindo–Sink complication classification system in pediatric orthopaedic surgery. JB JS Open Access 3(4):0020. https://doi.org/10.2106/JBJS.OA.18.00020(Published online 2018 Oct 23)
Lamarre ME, Parent S, Labelle H, Aubin CE, Joncas J, Cabral A, Petit Y (2009) Assessment of spinal flexibility in adolescent idiopathic scoliosis: suspension versus side-bending radiography. Spine (Phila Pa, 1976) 34(6):591–597. https://doi.org/10.1097/BRS.0b013e318193a23d
Ameri E, Behtash H, Mobini B, Daraie A (2015) Predictors of curve flexibility in adolescent idiopathic scoliosis: a retrospective study of 100 patients. Acta Med Iran 53(3):182–185
Crawford CH 3rd, Lenke LG (2010) Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: a case report. J Bone Jt Surg Am 92(1):202–209
Smith AD, Von Lackum WH, Wylie R (1954) An operation for stapling vertebral bodies in congenital scoliosis. J Bone Jt Surg Am 36(A2):342–348
Betz RR, Kim J, D’Andrea LP, Mulcahey MJ, Balsara RK, Clements DH (2003) An innovative technique of vertebral body stapling for the treatment of patients with adolescent idiopathic scoliosis: a feasibility, safety, and utility study. Spine 28(20):S255–S265. https://doi.org/10.1097/01.BRS.0000092484.31316.32
Puttlitz CM, Masaru F, Barkley A, Diab M, Acaroglu E (2007) A biomechanical assessment of thoracic spine stapling. Spine 32(7):766–771. https://doi.org/10.1097/01.brs.0000259073.16006.ed
Padhye K, Soroceanu A, Russell D, El-Hawary R (2018) Thoracoscopic anterior instrumentation and fusion as a treatment for adolescent idiopathic scoliosis: a systematic review of the literature. Spine Deform 6(4):384–390. https://doi.org/10.1016/j.jspd.2017.12.013
El-Hawary R, Sucato DJ (2005) Thoracoscopic approach for pediatric spinal deformity. Curr Opin Orthop 16(6):457–463
Wong HK, Ruiz JNM, Newton PO et al (2019) Non-fusion surgical correction of thoracic idiopathic scoliosis using a novel, braided vertebral body tethering device: minimum follow-up of 4 years. JB JS Open Access 4(4):e0026. https://doi.org/10.2106/JBJS.OA.19.00026(eCollection 2019 Oct–Dec)
Newton PO, Bartley CE, Bastrom TP et al (2020) Anterior spinal growth modulation in skeletally immature patients with idiopathic scoliosis: a comparison with posterior spinal fusion at 2 to 5 years postoperatively. J Bone Jt Surg Am. https://doi.org/10.2106/JBJS.19.01176
Coe JD, Arlet V, Donaldson W, et al. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine. 2006;31:345–9
Weiss H-R, Goodall D (2008) Rate of complications in scoliosis surgery—a systematic review of the pub med literature. Scoliosis 3:9. https://doi.org/10.1186/1748-7161-3-9
Halanski MA, Elfman CM, Cassidy JA et al (2013) Comparing results of posterior spine fusion in patients with AIS: are two surgeons better than one? J Orthop 10:54–58
Elnady B, El-Sharkawi MM, El-Meshtawy M, Adam FF, Said GZ (2017) Posterior-only surgical correction of adolescent idiopathic scoliosis: an Egyptian experience. SICOT J 3:69. https://doi.org/10.1051/sicotj/2017057(Epub 2017 Dec 11)
Verhofste BP, Berry JG, Miller PE, Crofton CN, Garrity BM, Fletcher ND, Marks MC, Shah SA, Newton PO, Samdani AF, Abel MF, Sponseller PD, Harms Study Group, Glotzbecker MP (2020) Risk factors for gastrointestinal complications after spinal fusion in children with cerebral palsy. Spine Deform. https://doi.org/10.1007/s43390-020-00233-y(Epub ahead of print)
Verhofste BP, Glotzbecker MP, Birch CM, O’Neill NP, Hedequist DJ (2019) Halo-gravity traction for the treatment of pediatric cervical spine disorders. J Neurosurg Pediatr 27:1–10. https://doi.org/10.3171/2019.10.PEDS19513(Epub ahead of print)
Cohen LL, Przybylski R, Marshall AC, Emans JB, Hedequist DJ (2020) Surgical correction of scoliosis in children with severe congenital heart disease and palliated single ventricle physiology. Spine (Phila Pa, 1976). https://doi.org/10.1097/BRS.0000000000003905(Epub ahead of print)
Funding
No funding was received for this work
Author information
Authors and Affiliations
Contributions
AA: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable. SP: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable. FM: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable. KS: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable. JM: design or the acquisition, analysis, or interpretation of datadrafted the work or revised it critically, approved, accountable. DS: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable. PG: design or the acquisition, analysis, or interpretation of datadrafted the work or revised it critically, approved, accountable. MV: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable. JO: design or the acquisition, analysis, or interpretation of datadrafted the work or revised it critically, approved, accountable. NS: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable. RHC: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable. Pediatric Spine Study Group: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable. RE-H: design or the acquisition, analysis, or interpretation of data, drafted the work or revised it critically, approved, accountable.
Corresponding author
Ethics declarations
Conflict of interest
Abdullah Abdullah has nothing to disclose. Stefan Parent (No PDF). Firoz Miyanji consults for Zimmer Biomet. Kevin Smit receives grant from Zimmer Biomet. Joshua Murphy consults for OrthoPediatrics, Depuy Synthes Spine and is a member of the physician advisory board. David Skaggs consults for Zimmer Biomet, orthobullets, Nuvasive, grand Rounds and Medtronic, is a board member of Growing Spine Foundation, Growing Spine Study Group, CHLA Foundation, is a member of the editorial board of Orthopedic Today, Spine Deformity, Wolter Kluwer Health, and Journal of Children's Orthopaedics, and has stocks or stock Options in Green Sun Medical, and Zipline Medical. Purnendu Gupta consults for DePuy Synthes. Michael Vitale Consults for Zimmer Biomet, Stryker, and Nuvvasive, is a board member of Pediatric Orthopedic Society of North America (POSNA), Scoliosis Research Society (SRS), Orthopedic Research and Education Foundation (OREF), and Children’s Spine Foundation (CSF). Jean Ouellet reports grants from AONA Foundation. Neil Saran has nothing to disclose. Robert H. Cho consults for DePuy Synthes, Prosidyan, NuVasive, and OrthoPediatrics. Pediatric Spine Study Group reports grants from Pediatric Orthopaedic Society of North America, grants from Food and Drug Administration, grants from NuVasive, grants from DePuy Synthes Spine, grants from Children’s Spine Foundation, and grants from Growing Spine Foundation. Ron El-Hawary consults for Depuy Synthes Spine, Medronic Spine, Globus Medical, Wishbone Medical, and Apifix Ltd, works in research and education with Depuy Synthes Spine, Joint Solutions and Medronic Spine, receives IP royalties from Wishbone Medical, and is a board member of the Pediatric Orthopaedic Society of North America, Scoliosis Research Society and the Children’s Spine Study Group.
Ethics approval
This work is a sub-study of the Pediatric Spine Study Group Registry which was approved by the Research Ethics Board at the IWK Health Centre (#1002256) in accordance with the ethical standards outlined in the Tri-Council Policy Statement and the 1964 Declaration of Helsinki and its later amendments. All sites have research ethics board approval for entry of subject data into the pediatric spine study group database (formerly the children’s spine study group database and the growing spine study group data base).
Consent to participate
All research participants or their legal guardians provided written consent to be a part of the registry and have the data collected be used in ongoing research on scoliosis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Grade | Definition |
|---|---|
I | A complication that does not result in deviation from routine follow-up in the postoperative period and has minimal clinical relevance and requires minimal treatment (e.g., antiemetics, antipyretics, analgesics, diuretics, electrolytes, antibiotics, and physiotherapy) or no treatment |
II | A deviation from the normal postoperative course (including unplanned clinic/office visits) that requires outpatient treatment, either pharmacological or close monitoring as an outpatient |
III | A complication that is treatable but requires surgical, endoscopic, or interventional radiology procedure(s), or an unplanned hospital readmission |
IVa | A complication that is life or limb-threatening, and/or requires ICU admission, a complication with potential for permanent disability but treatable, a complication that may require organ/joint resection/replacement. No long-term disability) |
IVb | A complication that is life or limb-threatening, and/or requires ICU admission, a complication that is not treatable, a complication that requires organ/joint resection/replacement or salvage surgery. With long-term disability |
V | Death |
Rights and permissions
About this article
Cite this article
Abdullah, A., Parent, S., Miyanji, F. et al. Risk of early complication following anterior vertebral body tethering for idiopathic scoliosis. Spine Deform 9, 1419–1431 (2021). https://doi.org/10.1007/s43390-021-00326-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00326-2