Abstract
Background
Cerebral palsy (CP) is a static encephalopathy with progressive musculoskeletal pathology. Non-ambulant children (GMFCS IV and V) with CP have high rates of spastic hip disease and neuromuscular scoliosis. The effect of spinal fusion and spinal deformity on hip dislocation following total hip arthroplasty has been well studied, however in CP this remains largely unknown. This study aimed to identify factors associated with worsening postoperative hip status (WHS) following corrective spinal fusion in children with GMFCS IV and V CP.
Methods
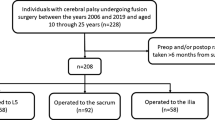
Retrospective review of GMFSC IV and V CP patients in a prospective multicenter database undergoing spinal fusion, with 5 years follow-up. WHS was determined by permutations of baseline (BL), 1 year, 2 years, and 5 years hip status and defined by a change from an enlocated hip at BL that became subluxated, dislocated or resected post-op, or a subluxated hip that became dislocated or resected. Hip status was analyzed against patient demographics, hip position, surgical variables, and coronal and sagittal spinal alignment parameters. Cutoff values for parameters at which the relationship with hip status was significant was determined using receiver operating characteristic curves. Logistic regression determined odds ratios for predictors of WHS.
Results
Eighty four patients were included. 37 (44%) had WHS postoperatively. ROC analysis and logistic regression demonstrated that the only spinopelvic alignment parameter that significantly correlated with WHS was lumbar hyperlordosis (T12-L5) > 60° (p = 0.028), OR = 2.77 (CI 1.10–6.94). All patients showed an increase in pre-to-postop LL. Change in LL pre-to-postop was no different between groups (p = 0.318), however the WHS group was more lordotic at BL and postop (pre44°/post58° vs pre32°/post51° in the no change group). Age, sex, Risser, hip position, levels fused, coronal parameters, global sagittal alignment (SVA), thoracic kyphosis, and reoperation were not associated with WHS.
Conclusion
Postoperative hyperlordosis(> 60°) is a risk factor for WHS at 5 years after spinal fusion in non-ambulant CP patients. WHS likely relates to anterior pelvic tilt and functional acetabular retroversion due to hyperlordosis, as well as loss of protective lumbopelvic motion causing anterior femoracetabular impingement.
Level of evidence
III.





Similar content being viewed by others
References
Rosenbaum P, Paneth N, Leviton A et al (2007) A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl 109:8–14
Palisano R, Rosenbaum P, Walter S et al (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39:214–223. https://doi.org/10.1111/j.1469-8749.1997.tb07414.x
Soo B, Howard JJ, Boyd RN et al (2006) Hip displacement in cerebral palsy. J Bone Jt Surg Am 88:121–129. https://doi.org/10.2106/JBJS.E.00071
Persson-Bunke M, Hägglund G, Lauge-Pedersen H et al (2012) Scoliosis in a total population of children with cerebral palsy. Spine 37:E708–E713. https://doi.org/10.1097/BRS.0b013e318246a962
Stanitski CL, Micheli LJ, Hall JE, Rosenthal RK (1982) Surgical correction of spinal deformity in cerebral palsy. Spine 7:563–569. https://doi.org/10.1097/00007632-198211000-00009
Yildiz C, Demirkale I (2014) Hip problems in cerebral palsy: screening, diagnosis and treatment. Curr Opin Pediatr 26:85–92. https://doi.org/10.1097/MOP.0000000000000040
Terjesen T (2012) The natural history of hip development in cerebral palsy. Dev Med Child Neurol 54:951–957. https://doi.org/10.1111/j.1469-8749.2012.04385.x
Lonstein JE, Beck K (1986) Hip dislocation and subluxation in cerebral palsy. J Pediatr Orthop 6:521–526. https://doi.org/10.1097/01241398-198609000-00001
Narayanan UG, Fehlings D, Weir S et al (2006) Initial development and validation of the caregiver priorities and child health index of life with disabilities (CPCHILD). Dev Med Child Neurol 48:804–812. https://doi.org/10.1017/S0012162206001745
DiFazio R, Shore B, Vessey JA et al (2016) Effect of hip reconstructive surgery on health-related quality of life of non-ambulatory children with cerebral palsy. J Bone Jt Surg Am 98:1190–1198. https://doi.org/10.2106/JBJS.15.01063
Shore BJ, Graham HK (2017) Management of moderate to severe hip displacement in nonambulatory children with cerebral palsy. JBJS Rev 5
Pountney T, Green EM (2006) Hip dislocation in cerebral palsy. BMJ (Clin Res Ed) 332:772–775. https://doi.org/10.1136/bmj.332.7544.772
McCarthy JJ, D’Andrea LP, Betz RR, Clements DH (2006) Scoliosis in the child with cerebral palsy. J Am Acad Orthopaedic Surg 14:367–375. https://doi.org/10.5435/00124635-200606000-00006
BC Children’s Hospital. Hip displacement surgery. http://www.bcchildrens.ca/our-services/clinics/orthopaedics/orthopaedic-cerebral-palsy/hip-displacement-surgery. Accessed 22 Apr 2019
Rubin CG, Rubin PG (2014) Surface arthroplasty in a cerebral palsied patient with hip dysplasia and dislocation. F1000Research 3:16. https://doi.org/10.12688/f1000research.3-16.v1
Burns F, Stewart R, Reddihough D et al (2014) The cerebral palsy transition clinic: administrative chore, clinical responsibility, or opportunity for audit and clinical research? J Child Orthopaedics 8:203–213. https://doi.org/10.1007/s11832-014-0569-0
Scoliosis Research Society. SRS terminology committee and working group on spinal classification revised glossary of terms. March 2000. https://www.srs.org/professionals/online-education-and-resources/glossary/revised-glossary-of-terms#pobl. Accessed 22 Apr 2019
Patel J, Shapiro F (2015) Simultaneous progression patterns of scoliosis, pelvic obliquity, and hip subluxation/dislocation in non-ambulatory neuromuscular patients: an approach to deformity documentation. J Child Orthopaedics 9:345–356. https://doi.org/10.1007/s11832-015-0683-7
Hägglund G, Andersson S, Düppe H et al (2005) Prevention of dislocation of the hip in children with cerebral palsy. The first ten years of a population-based prevention programme. J Bone Jt Surg Br 87:95–101
Karampalis C, Tsirikos AI (2014) The surgical treatment of lordoscoliosis and hyperlordosis in patients with quadriplegic cerebral palsy. Bone Jt J 96-B:800–806. https://doi.org/10.1302/0301-620X.96B6.33020
Buckland AJ, Vigdorchik J, Schwab FJ et al (2015) Acetabular anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Jt Surg Am 97:1913–1920. https://doi.org/10.2106/JBJS.O.00276
Park T, Dobbs MB, Cho J (2018) Evidence supporting selective dorsal rhizotomy for treatment of spastic cerebral palsy. Cureus. https://doi.org/10.7759/cureus.3466
Peter C, Arens LJ, Peacock WJ (1990) Incidence of spinal deformity in children after multiple level laminectomy for selective posterior rhizotomy. Springer, Berlin
Henebry A, Gaskill T (2013) The effect of pelvic tilt on radiographic markers of acetabular coverage. Am J Sports Med 41:2599–2603. https://doi.org/10.1177/0363546513500632
Miki H, Kyo T, Kuroda Y et al (2014) Risk of edge-loading and prosthesis impingement due to posterior pelvic tilting after total hip arthroplasty. Clin Biomech (Bristol, Avon) 29:607–613. https://doi.org/10.1016/j.clinbiomech.2014.05.002
Crawford L, Herrera-Soto J, Ruder JA et al (2017) The fate of the neuromuscular hip after spinal fusion. J Pediatr Orthop 37:403–408. https://doi.org/10.1097/bpo.0000000000000689
Vialle R, Delecourt C, Morin C (2006) Surgical treatment of scoliosis with pelvic obliquity in cerebral palsy: the influence of intraoperative traction. Spine 31:1461–1466. https://doi.org/10.1097/01.brs.0000219874.46680.87
Drummond D, Breed AL, Narechania R (1985) Relationship of spine deformity and pelvic obliquity on sitting pressure distributions and decubitus ulceration. J Pediatr Orthop 5:396–402. https://doi.org/10.1097/01241398-198507000-00002
Winter RB, Pinto WC (1986) Pelvic obliquity. Its causes and its treatment. Spine 11:225–234
Heidt C, Hollander K, Wawrzuta J et al (2015) The radiological assessment of pelvic obliquity in cerebral palsy and the impact on hip development. Bone Jt J 97:1435–1440. https://doi.org/10.1302/0301-620X.97B10.35390
Jain A, Sponseller PD, Shah SA et al (2016) Subclassification of GMFCS level-5 cerebral palsy as a predictor of complications and health-related quality of life after spinal arthrodesis. J Bone Jt Surg Am 98:1821–1828. https://doi.org/10.2106/JBJS.15.01359
Funding
Support provided by The Harms Study Group (HSG) and the Setting Scoliosis Straight Foundation. The collaboration and non-financial support of the NHMRC funded Centre of Research Excellence in Cerebral Palsy (CPAchieve) is acknowledged.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by DW, DVM and AJB. The first draft of the manuscript was written by DW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript, and agree to be accountable for all aspects of the work ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
IRB approval
IRB approval was obtained at each participating site and informed consent was given by each patient. Spine Research Center - NYU Langone Health, Department of Orthopaedic Surgery, Spine Division.
Device/drug statement
The manuscript submitted does not contain information about medical device(s)/drug(s).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Buckland, A.J., Woo, D., Kerr Graham, H. et al. Residual lumbar hyperlordosis is associated with worsened hip status 5 years after scoliosis correction in non-ambulant patients with cerebral palsy. Spine Deform 9, 1125–1136 (2021). https://doi.org/10.1007/s43390-020-00281-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00281-4